Cardinal Presentations
This post is part of a series called “Cardinal Presentations”, based on Rosen’s Emergency Medicine (8th edition).
Brief HPI:
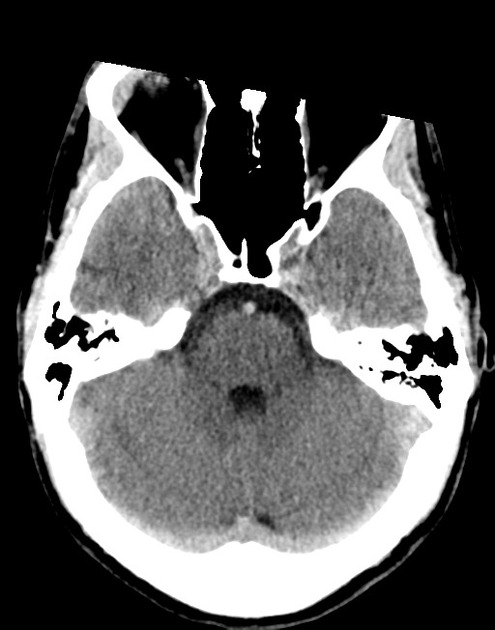
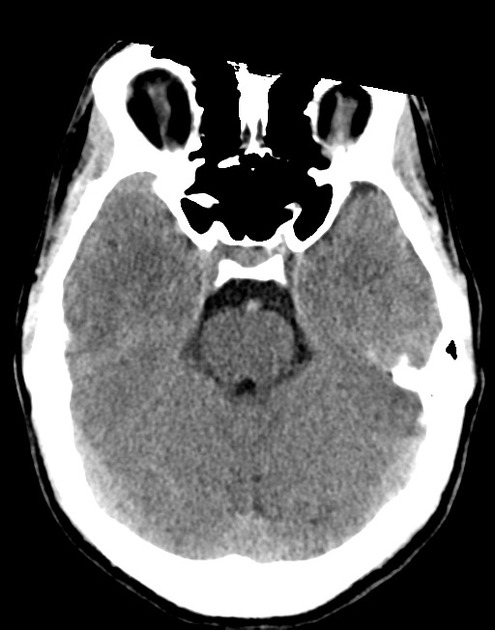
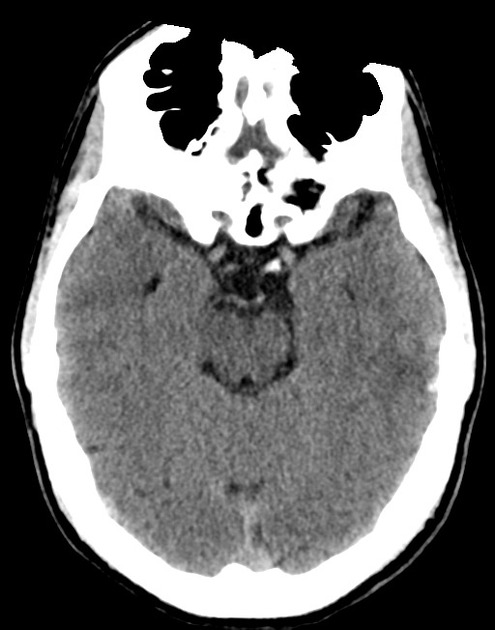
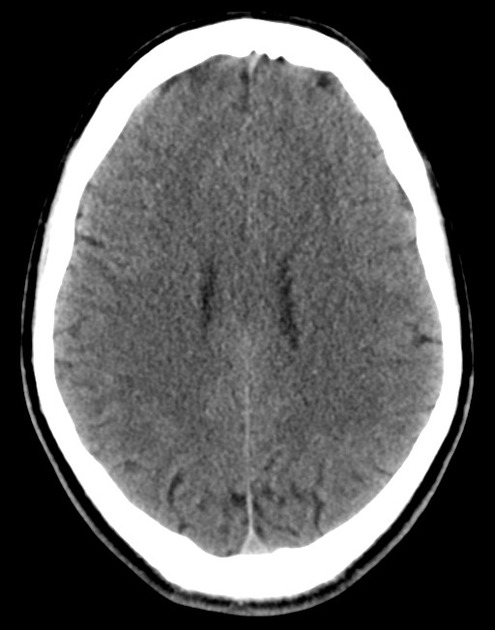
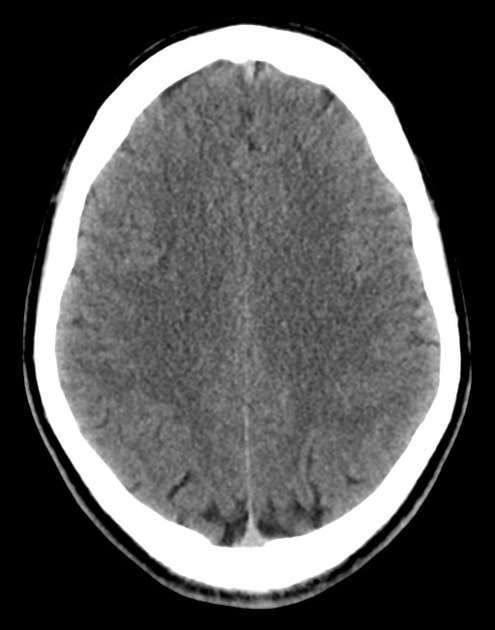
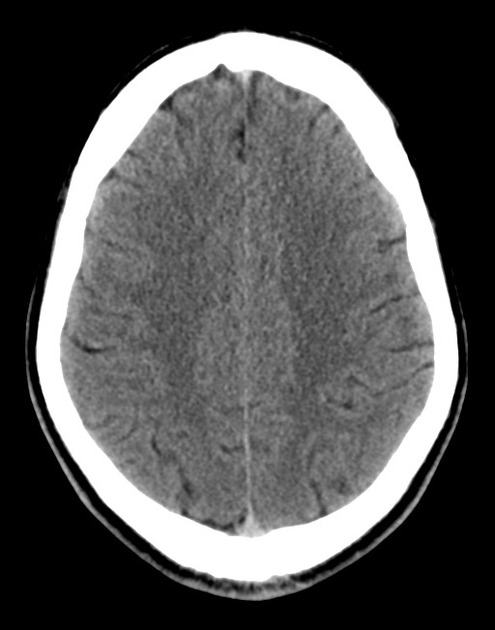
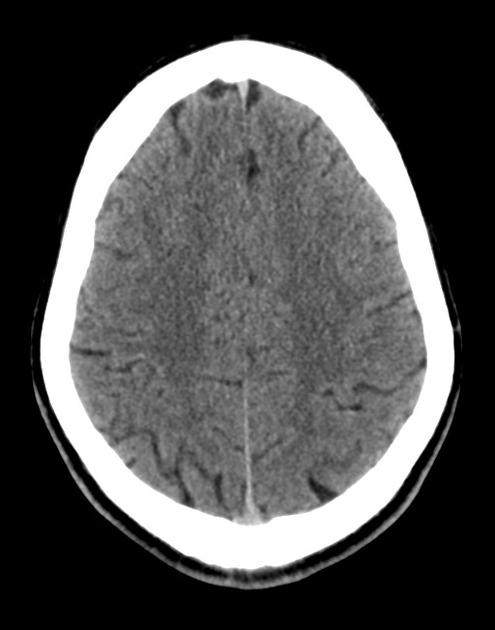
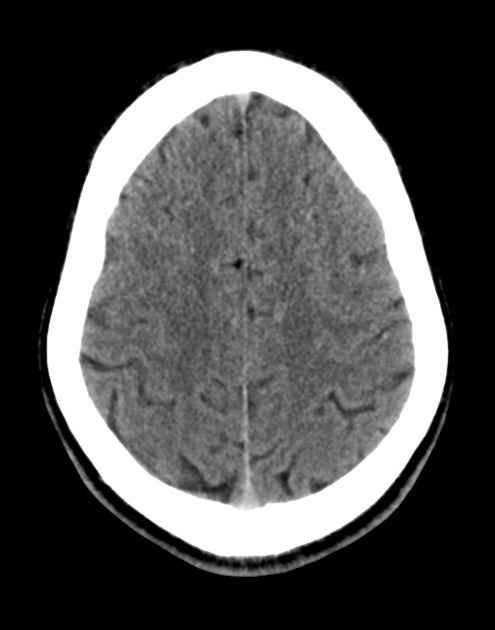
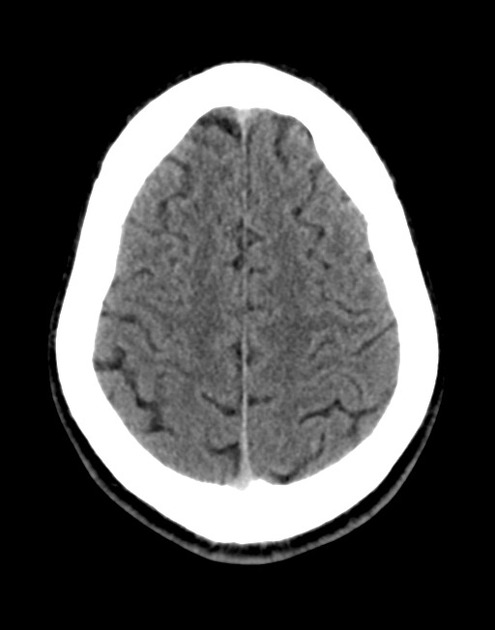
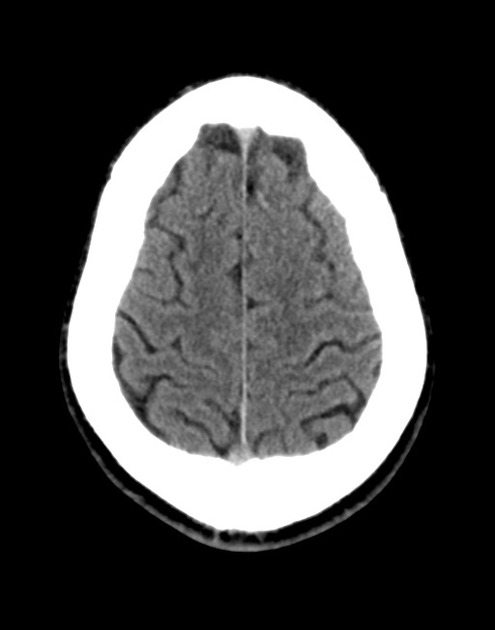
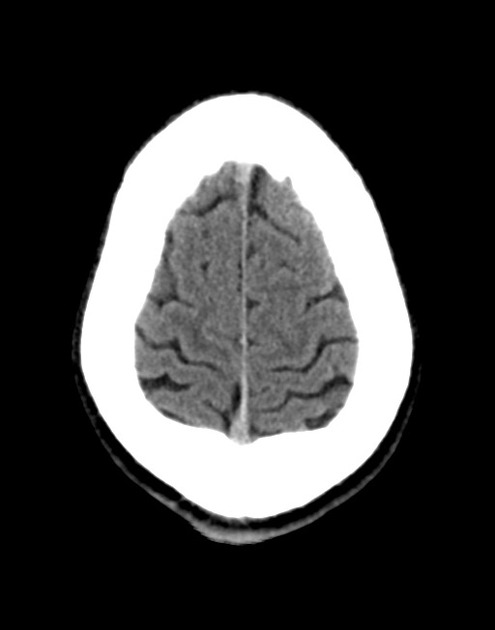
A 48 year-old male with hypertension and hyperlipidemia presents with headache. Notes onset of symptoms 8 hours prior to presentation, reaching maximal severity within seconds. Headache improved with over-the-counter analgesics. On examination, there are no neurological deficits, neck is supple. A CT head non-contrast is obtained:
CT Head:
No acute intracranial process. Case courtesy of Assoc Prof Craig Hacking, Radiopaedia.org, rID: 37118
ED Course:
A lumbar puncture is performed, CSF sampling reveals xanthochromia – neurosurgery is consulted and the patient is admitted for angiography and possible intervention.
An Algorithm for the Evaluation of Headache
High-Risk Historical Features
- Sudden onset (seconds/minutes), patient recalls activity at onset
- Worst in life or change in character from established headache
- Fever, neck pain/stiffness
- Altered mental status
- Malignancy
- Coagulopathy: iatrogenic, hepatopathy, dialysis
- Immunocompromised
- Rare: CO exposure, jaw claudication, PCKD
Location of Pain
- Unilateral: migraine
- Periorbital: glaucoma, CVT, optic neuritis, cluster
- Facial/maxillary: trigeminal neuralgia, sinusitis
- Temporal: GCA
- Occipital: cerebellar stroke
- Nuchal: meningitis
Characteristics of Primary Headaches
| Type | Location | Duration | Quality | Associated symptoms | Comment |
|---|---|---|---|---|---|
| Migraine | Unilateral | Hours to days | Throbbing | Photophobia, phonophobia | Atypical migraines with neurological findings (basilar, ophthalmoplegic, ophthalmic, hemiplegic) |
| Tension | Bilateral | Minutes to days | Constricting | None | |
| Cluster | Unilateral, periorbital | Minutes to hours | Throbbing | Conjunctival injection, lacrimation, rhinorrhea, miosis, eyelid edema | Males 90%, triggered by EtOH. |
Physical Examination Findings
- Vital Signs
- Fever: present in 95% of patients with meningitis
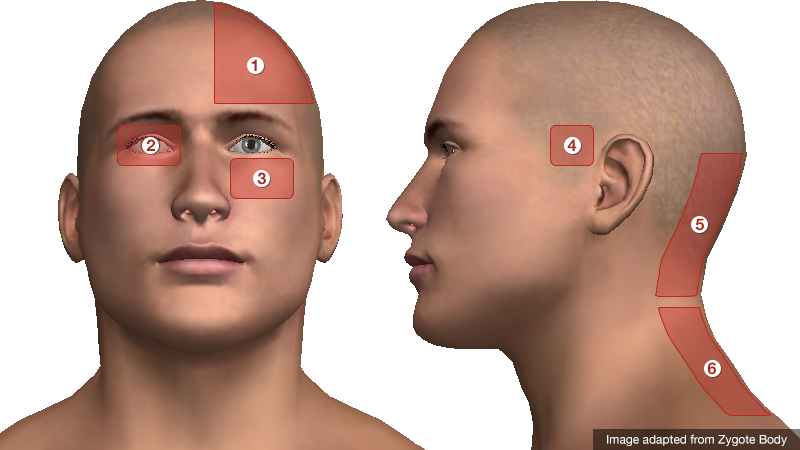
- Head
- Trauma: signs of basilar skull fracture
- Temporal artery tenderness/induration: GCA
- Pericranial muscle tenderness: tension headache
- Trigger point, Tinnel sign: occipital neuralgia
- Eyes
- Pupillary defects: aneurysm with CN III compression
- Papilledema, absence of spontaneous venous pulsations: elevated intracranial pressure
- EOM abnormalities: ICH, mass lesion, neuropathy (DM, Lyme)
- Horner syndrome (ptosis, miosis, anhidrosis): carotid dissection
- Visual field defect: stroke, atypical migraine
- Conjunctival injection: glaucoma (fixed, mid-size pupil, elevated intraocular pressure), cluster headache
- Mouth
- Thrush: immunocompromise
- Sinuses
- Tenderness to palpation, abnormal transillumination: sinusitis
- Neck
- Resistance to supine neck flexion: meningitis
- Kernig: supine position, hip flexed, knee flexed, resistance to knee extension
- Brudzinski: supine position, neck flexion results in knee flexion
- Jolt accentuation: patient rotates head side-to-side, 2-3 times/sec exacerbates headache
References:
- Russi, C. (2013). Headache. In Rosen’s Emergency Medicine – Concepts and Clinical Practice (8th ed., Vol. 1, pp. 170-175). Elsevier Health Sciences.
- Godwin SA, Villa J. “Acute headache in the ED: Evidence-Based Evaluation and Treatment Options.” Emerg Med Pract 2001; 3(6): 1-32.
- Edlow, J. A., Panagos, P. D., Godwin, S. A., Thomas, T. L., & Decker, W. W. (2008). Clinical Policy: Critical Issues in the Evaluation and Management of Adult Patients Presenting to the Emergency Department With Acute Headache. Annals of emergency medicine, 52(4), 407–436. doi:10.1016/j.annemergmed.2008.07.001
- WikEM: Headache