The emergency physician should be adept at the interpretation of computed tomography of the head, particularly for life-threatening processes where awaiting a radiologist interpretation may unnecessarily delay care.
As with the approach detailed previously for imaging of the abdomen and pelvis, a similar structured method for interpretation of head imaging exists and follows the mnemonic “Blood Can Be Very Bad”.
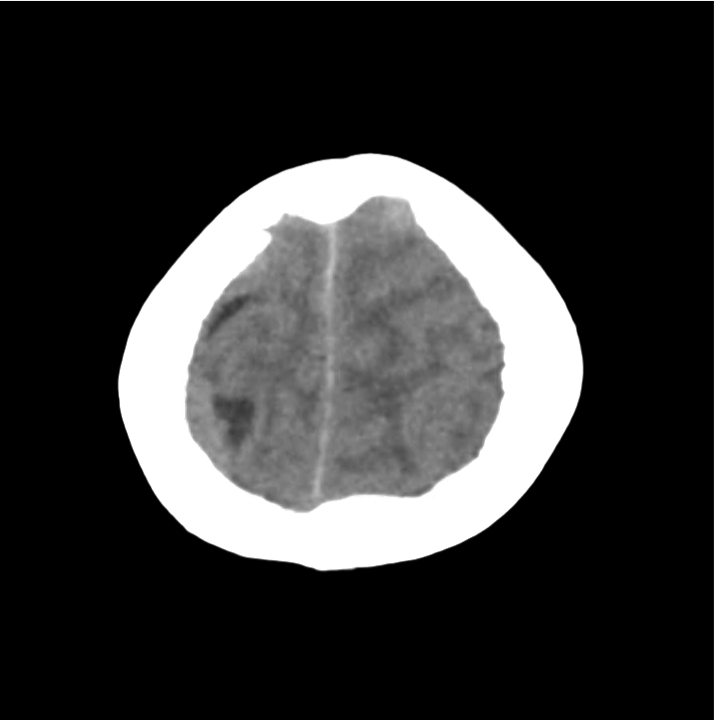
Normal Neuroanatomy
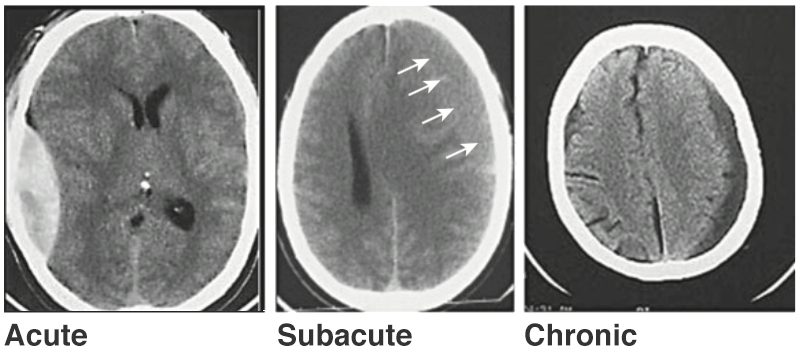
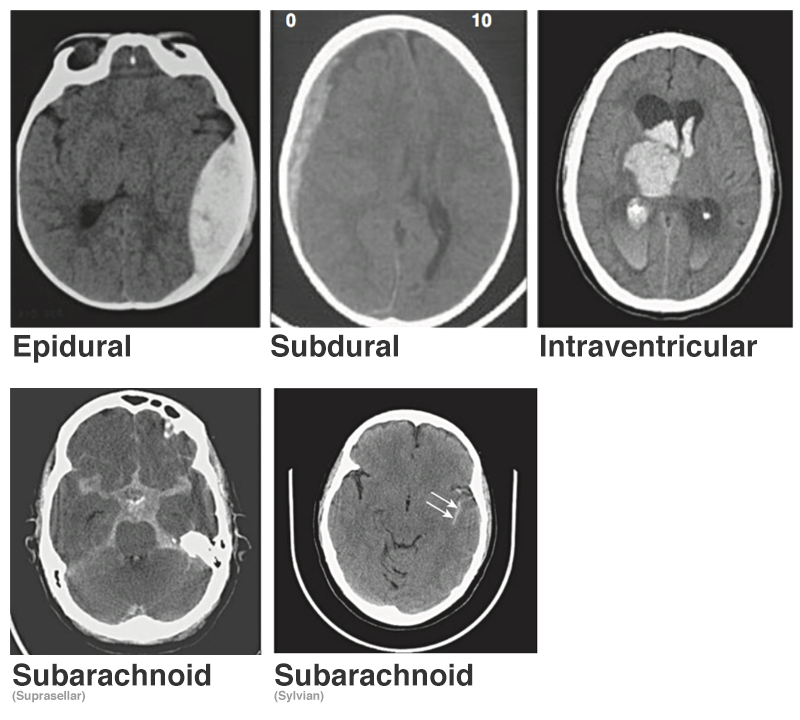
Blood: Blood
- Density
- Acute: hyperdense (50-100HU)
- 1-2wks: isodense with brain
- 2-3wks: hypodense with brain
Types/Locations
- Intraparenchymal Hemorrhage/Contusions
- Sudden deceleration of the head causes the brain to impact on bony prominences (e.g., temporal, frontal, occipital poles).
- Non-traumatic hemorrhagic lesions seen more frequently in elderly and located in basal ganglia.
- Intraventricular Hemorrhage
- White density in otherwise black ventricular spaces, can lead to obstructive hydrocephalus and elevated ICP.
- Associated with worse prognosis in trauma.
- Subarachnoid Hemorrhage
- Hemorrhage into subarachnoid space usually filled with CSF (cistern, brain convexity).
- Extracranial Hemorrhage
- Presence of significant extracranial blood or soft-tissue swelling should point examiner to evaluation of underlying brain parenchyma, opposing brain parenchyma (for contrecoup injuries) and underlying bone for identification of fractures.
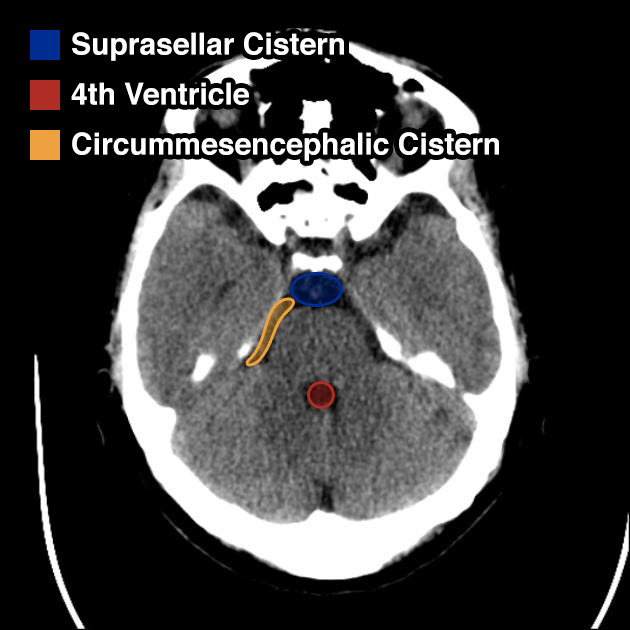
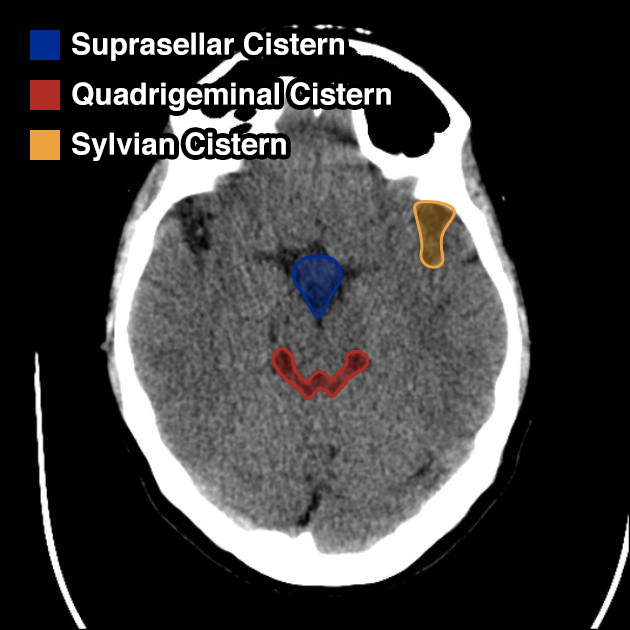
Can: Cisterns
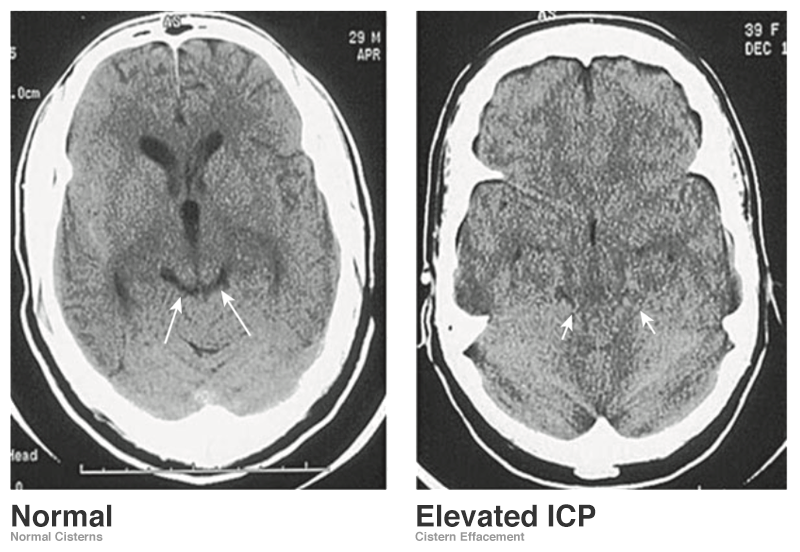
Evaluating the cisterns is important for the identification of increased intracranial pressures (assessed by effacement of spaces) and presence of subarachnoid blood.
- Circummesencephalic: CSF ring around midbrain and most sensitive marker for elevated ICP
- Suprasellar: Star-shaped space above the sella
- Quadrigeminal: W-shaped space at the top of the midbrain
- Sylvian: Bilateral space between temporal/frontal lobes
Be: Brain
Evaluate the brain parenchyma, including an assessment of symmetry of the gyri/sulci pattern, midline shift, and a clear gray-white differentiation.
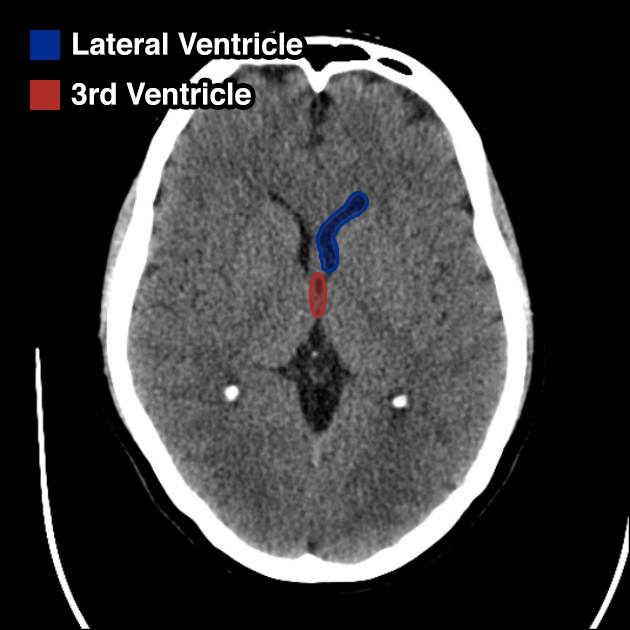
Very: Ventricles
Evaluate the ventricles for dilation or compression. Compare the ventricle size to the size of cisterns, large ventricles with normal/compressed cisterns and sulcal spaces suggests obstruction.
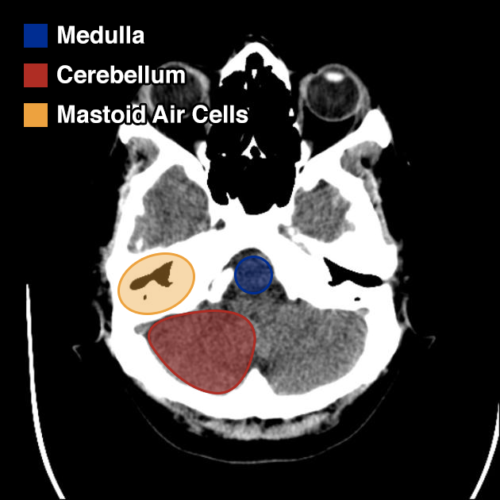
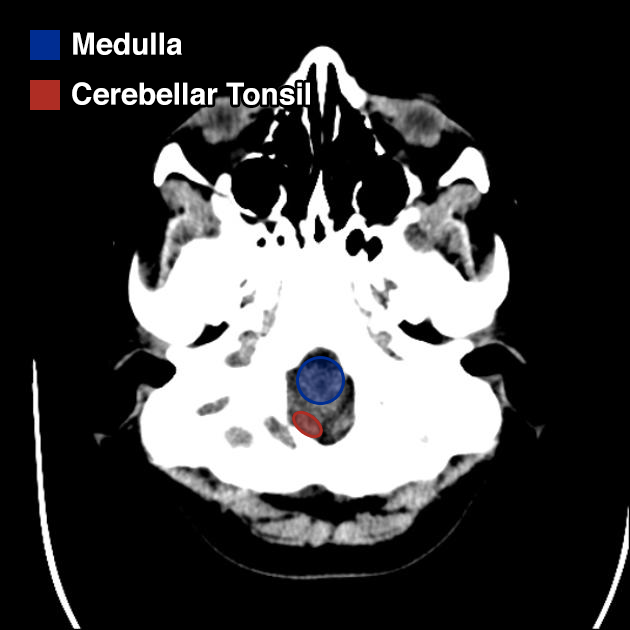
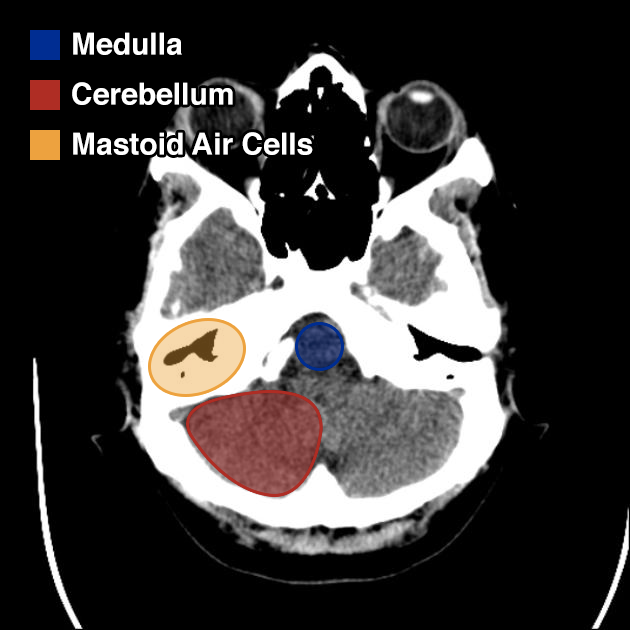
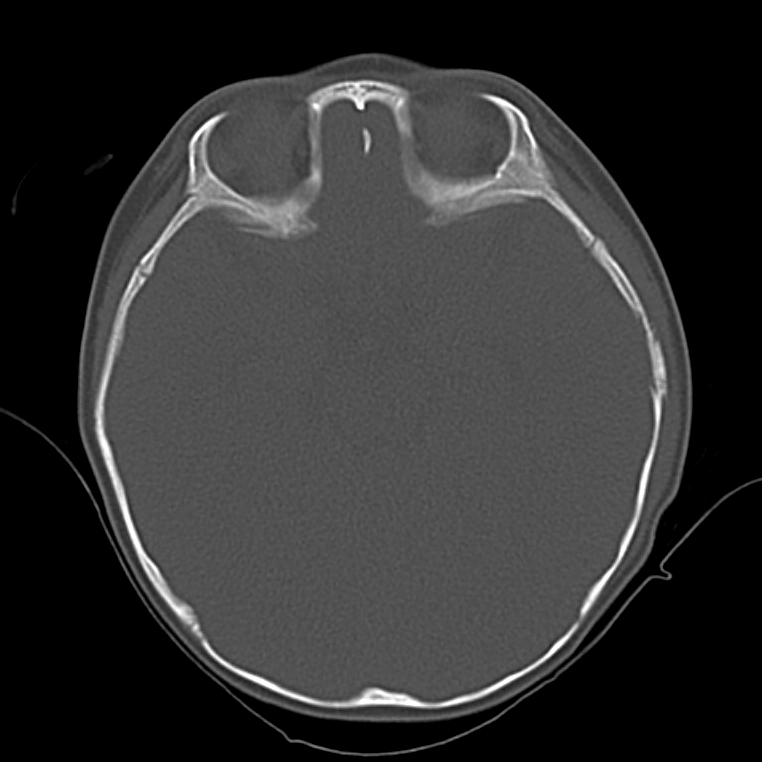
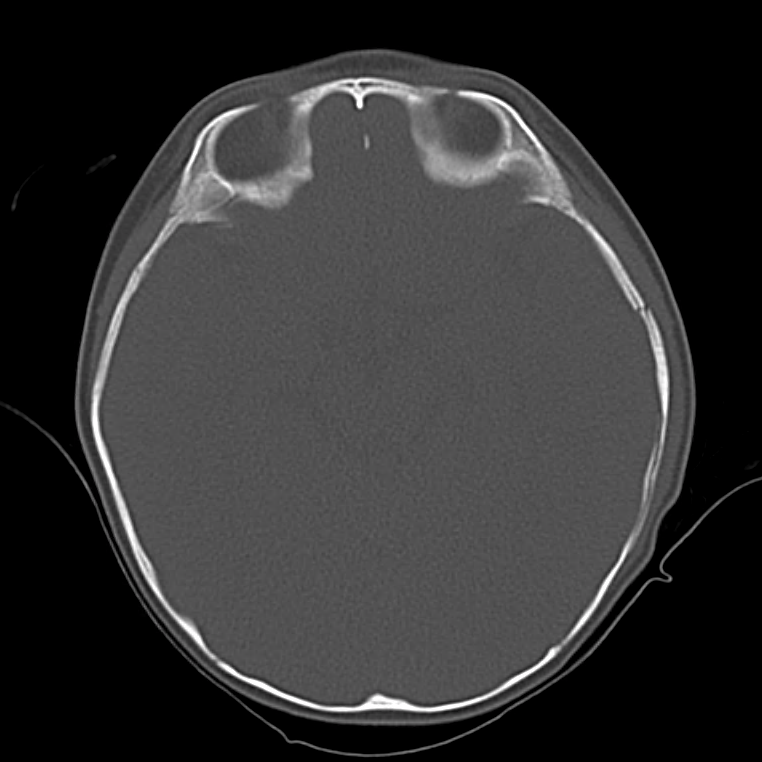
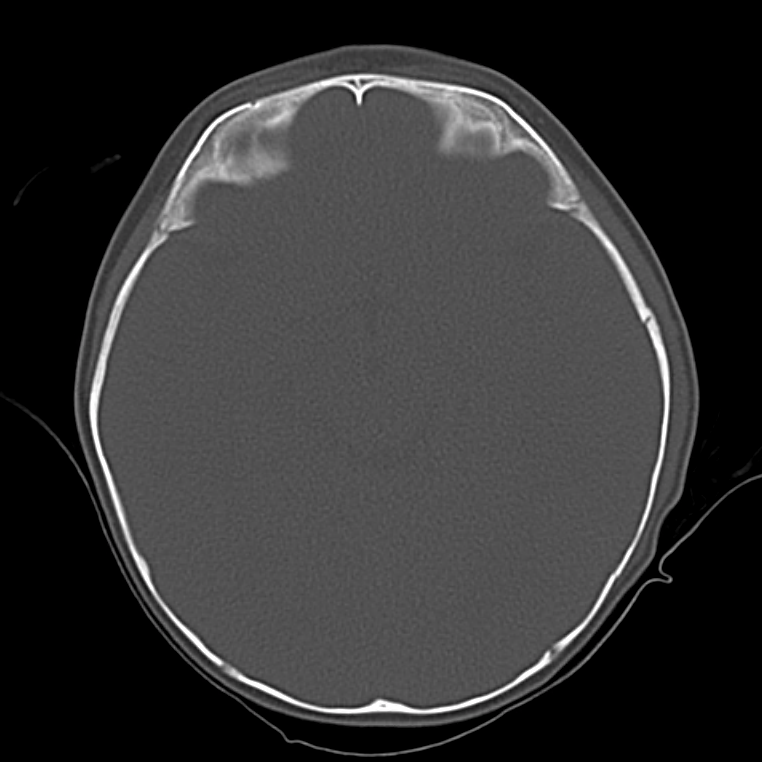
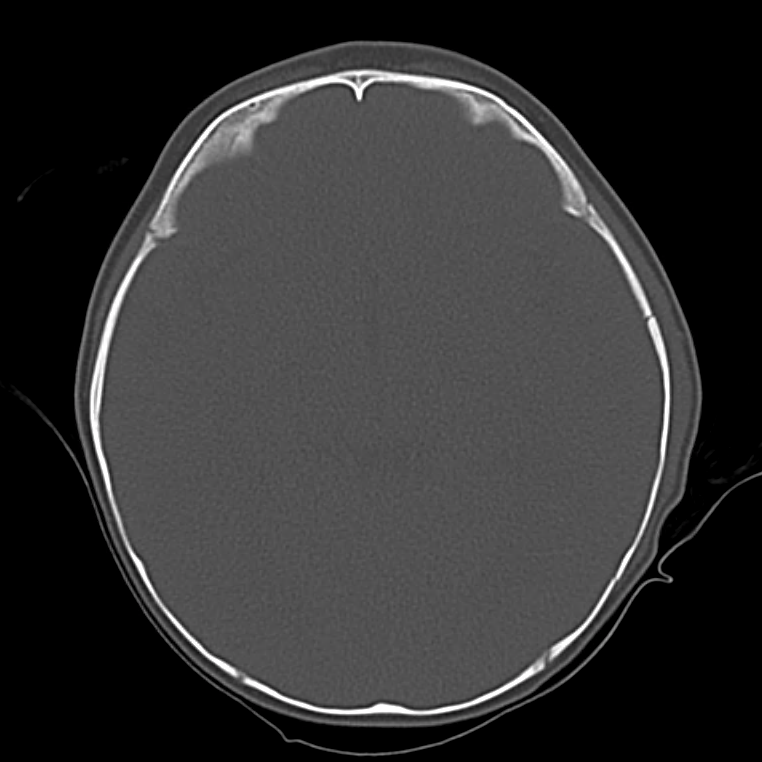
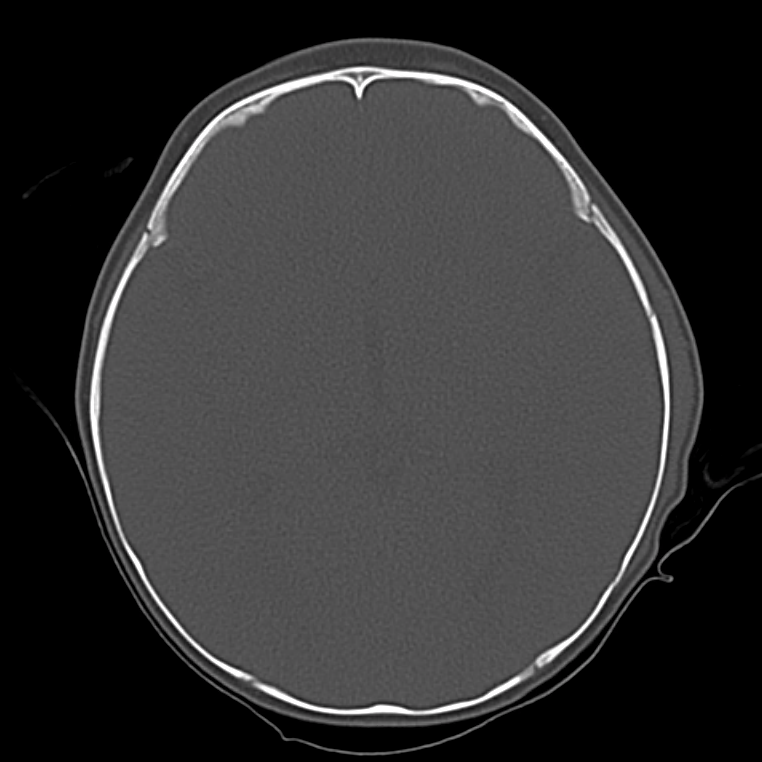
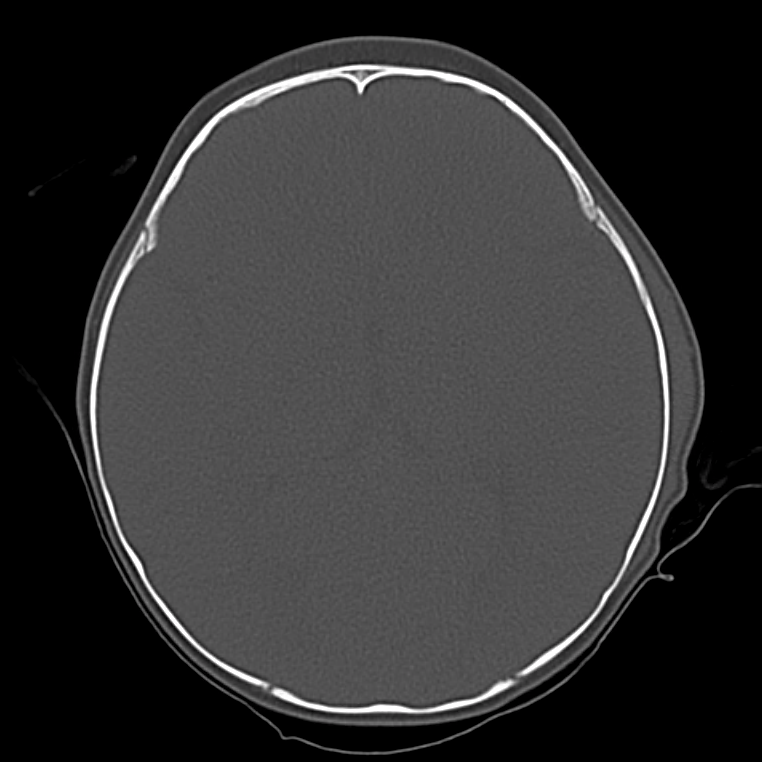
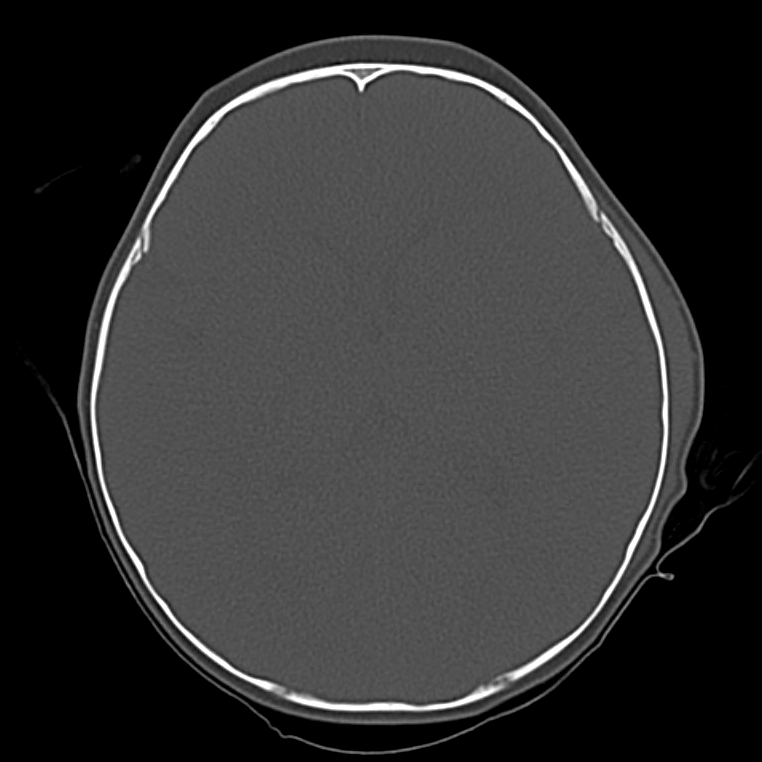
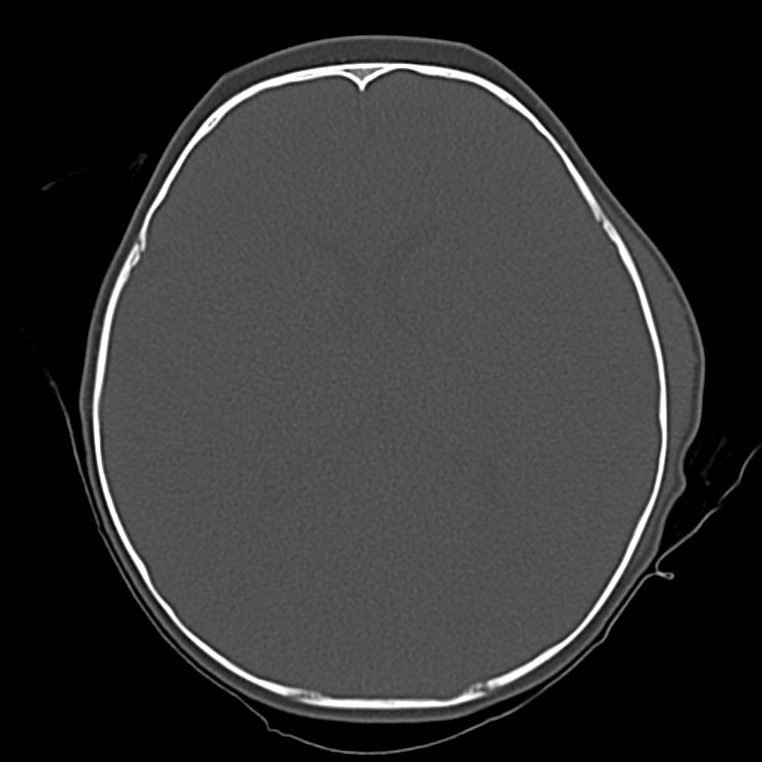
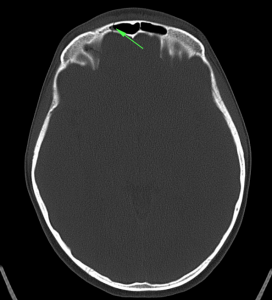
Bad: Bone
Switch to bone windows to evaluate for fracture. The identification of small, linear, non-depressed skull fractures may be difficult to identify as they are often confused with sutures – surrogates include pneumocephalus, and abnormal aeration of mastoid air cells and sinuses. The Presence of fractures increases the suspicion for intracranial injury, search adjacent and opposing parenchyma and extra-axial spaces.
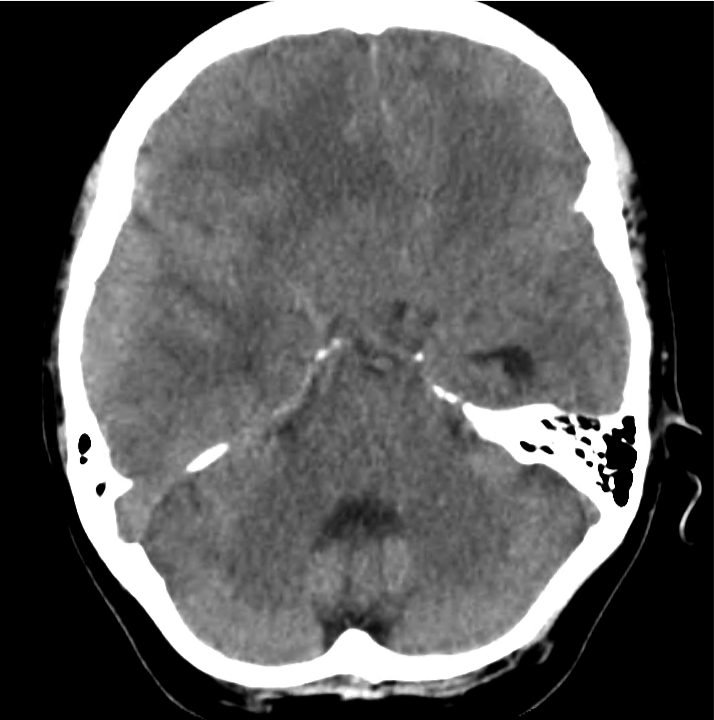
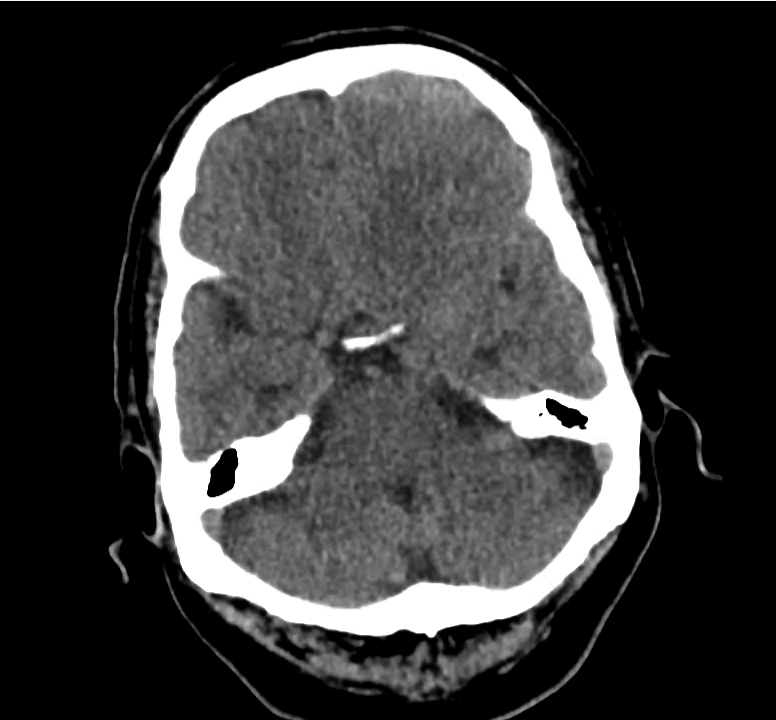
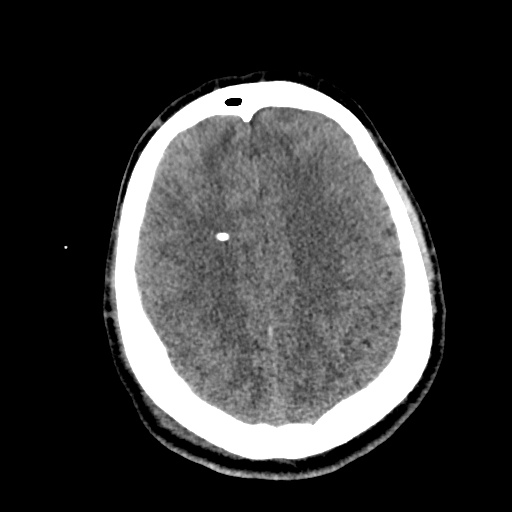
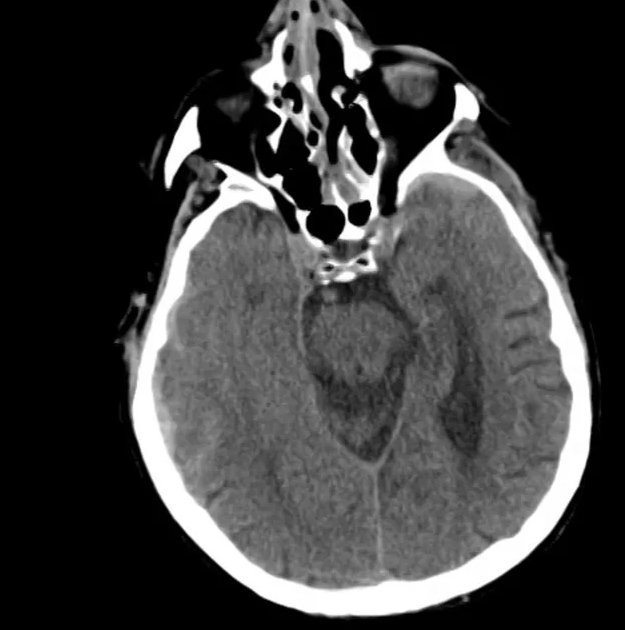
Example #1
CT Head Interpretation
- Ill-defined lesion in right parietal white matter with a large amount of surrounding vasogenic edema with midline shift and right uncal herniation.
- Acute on subacute right extra-axial subdural hematoma.
- Effacement of basilar cisterns.
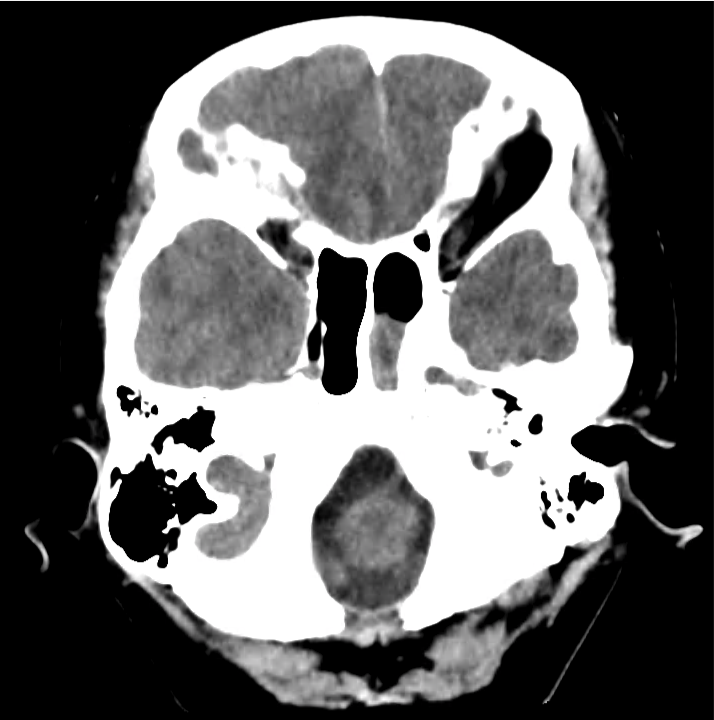
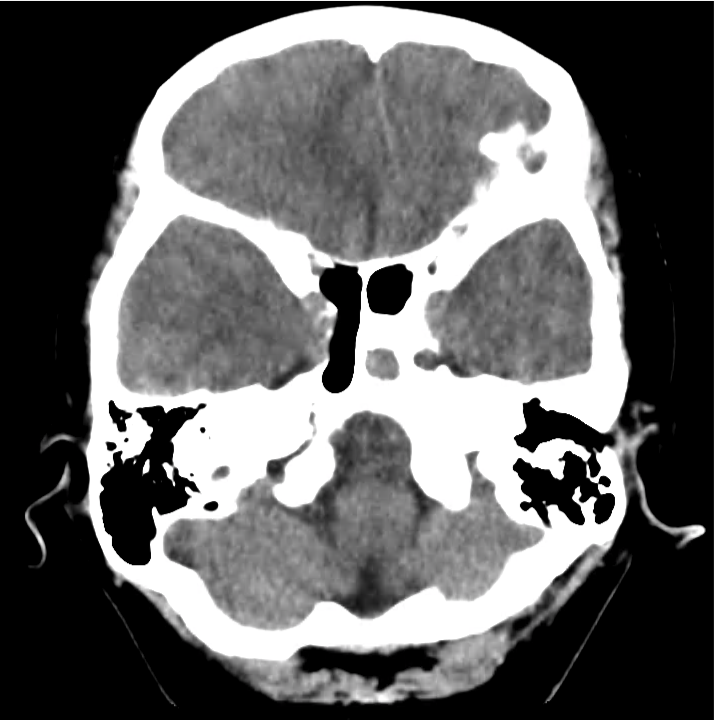
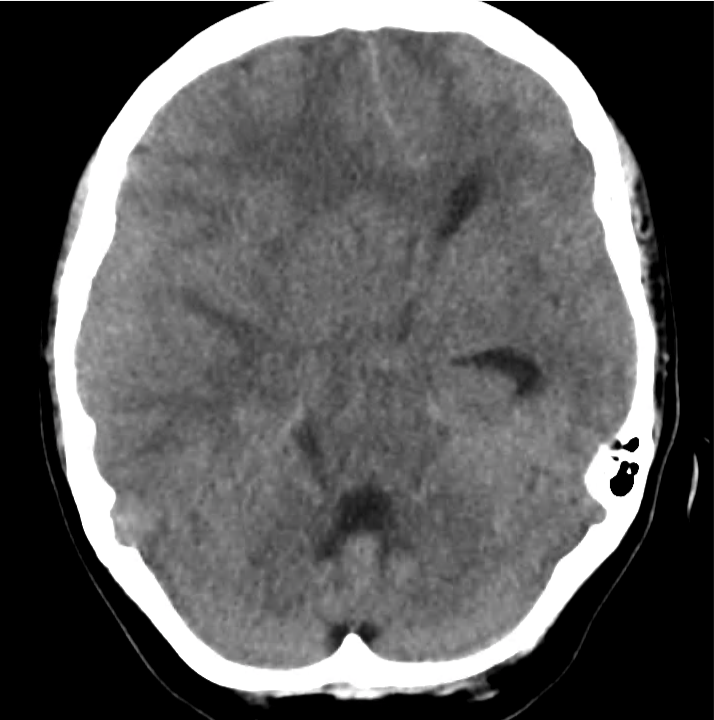
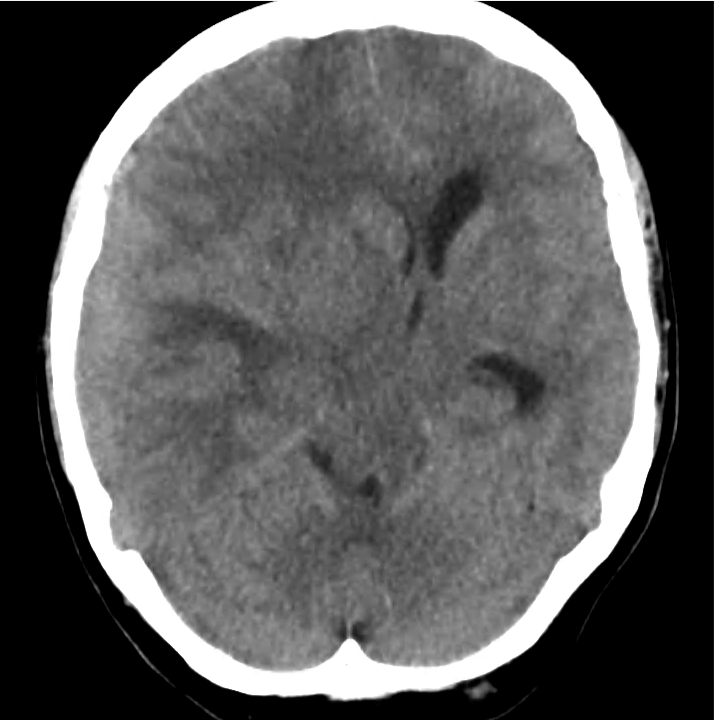
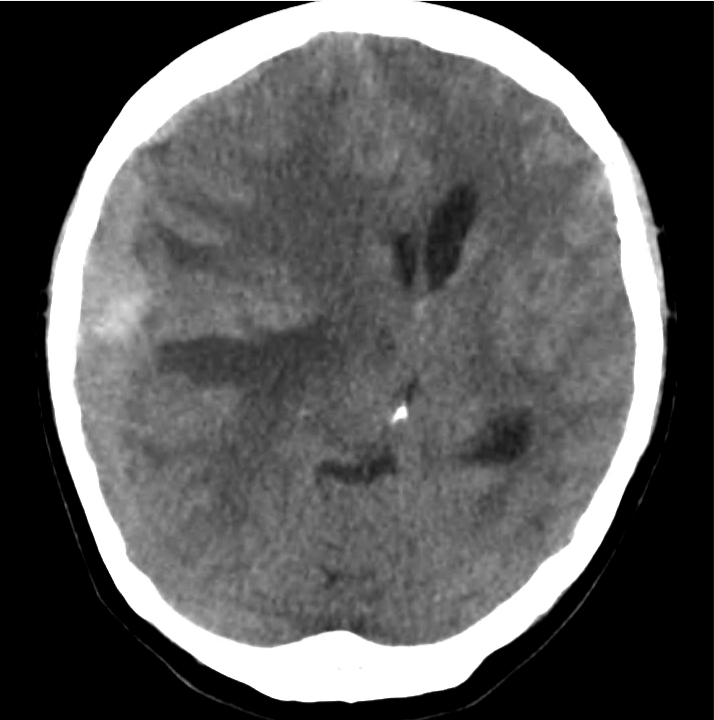
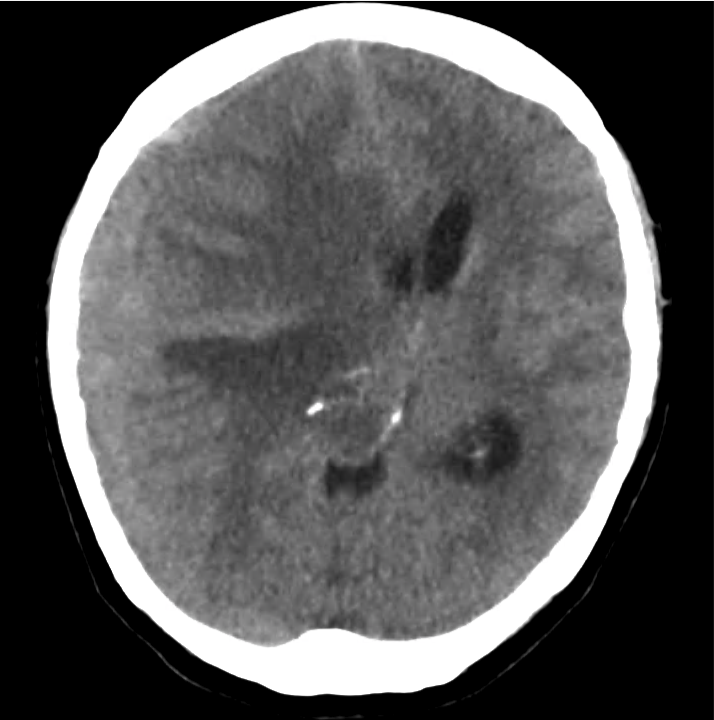
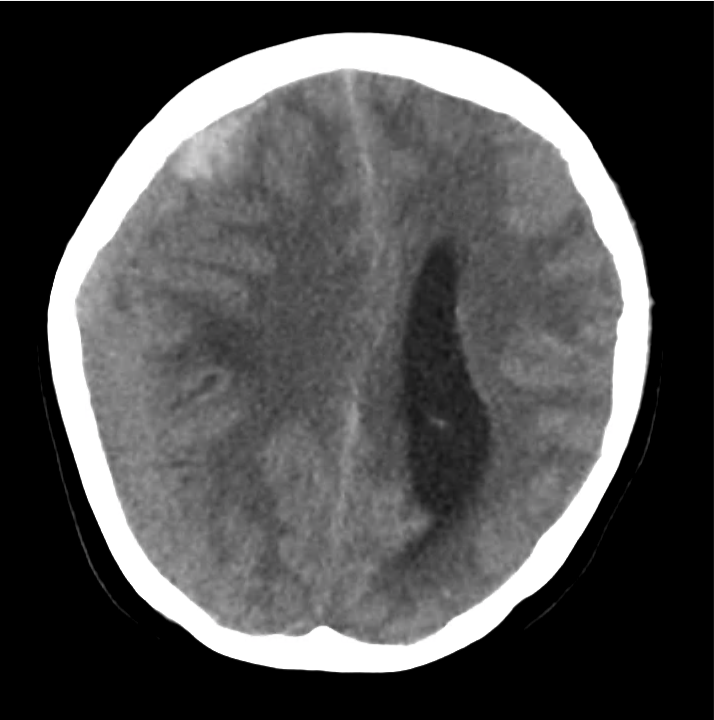
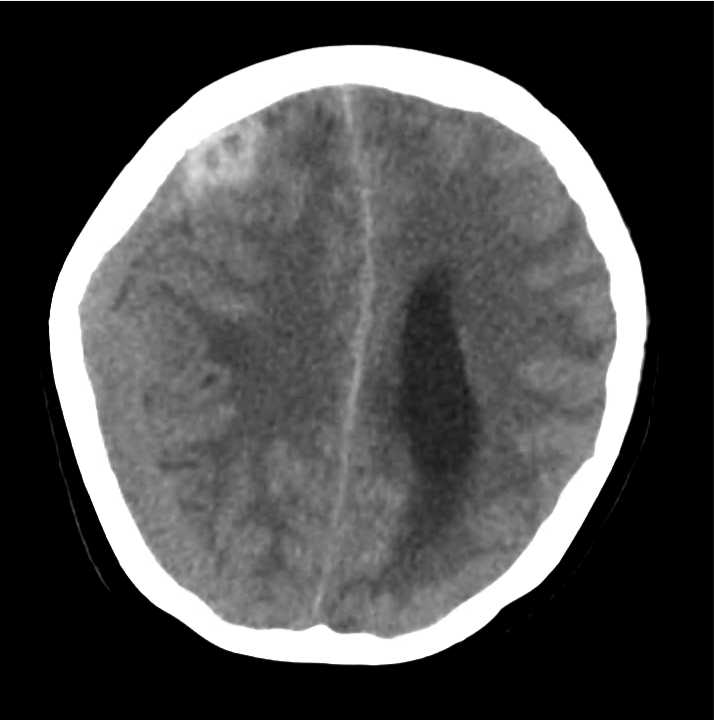
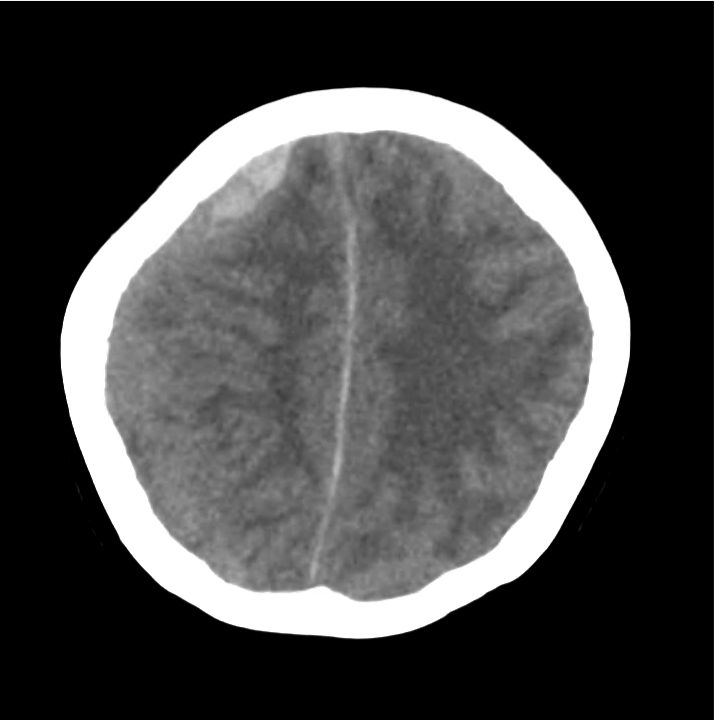
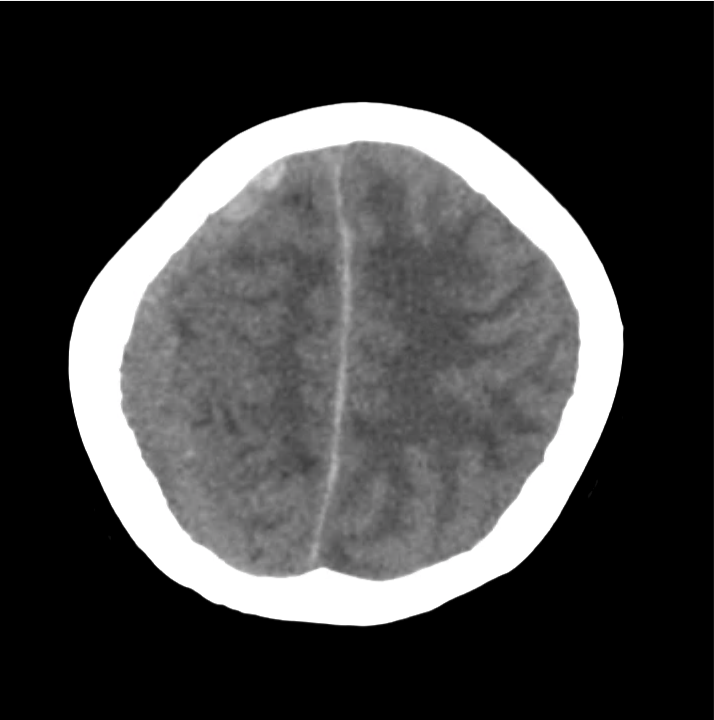
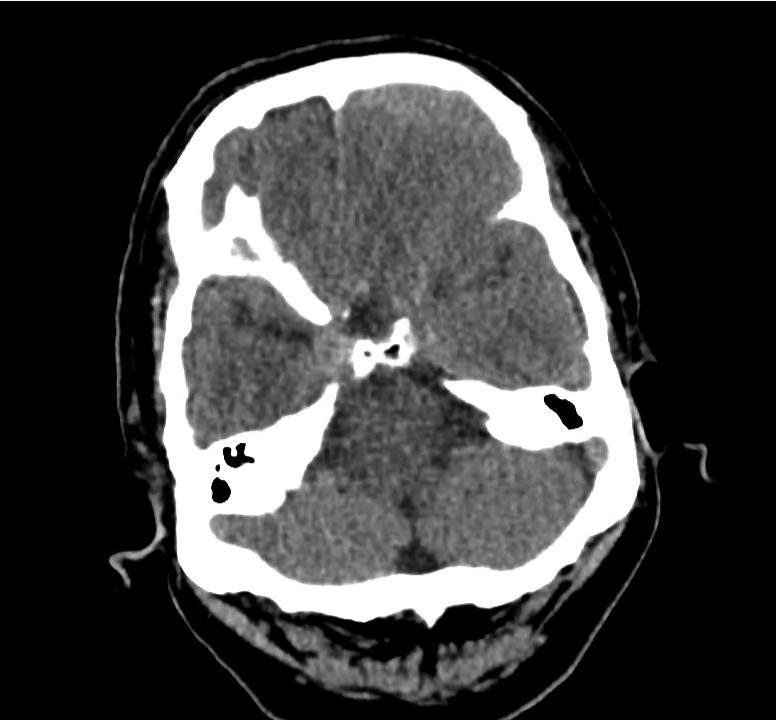
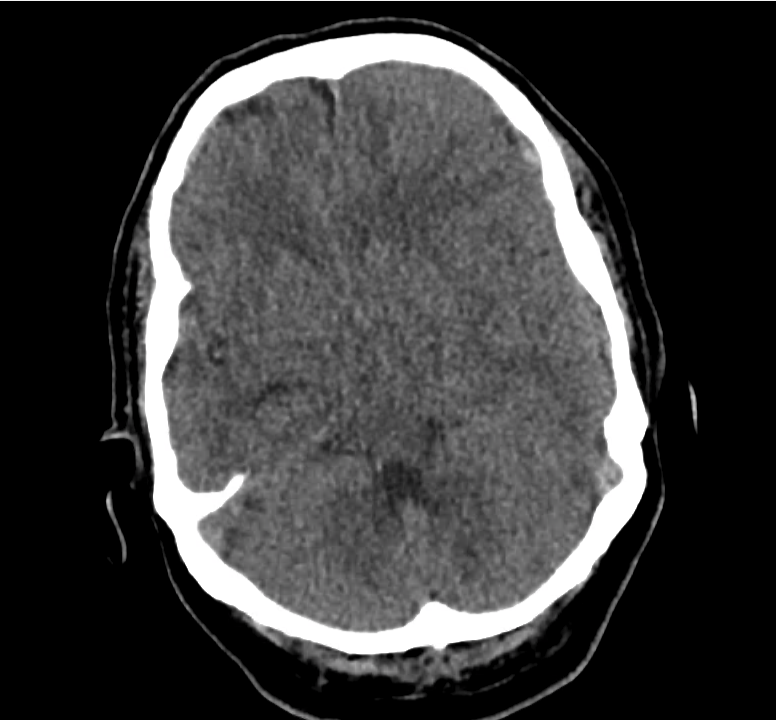
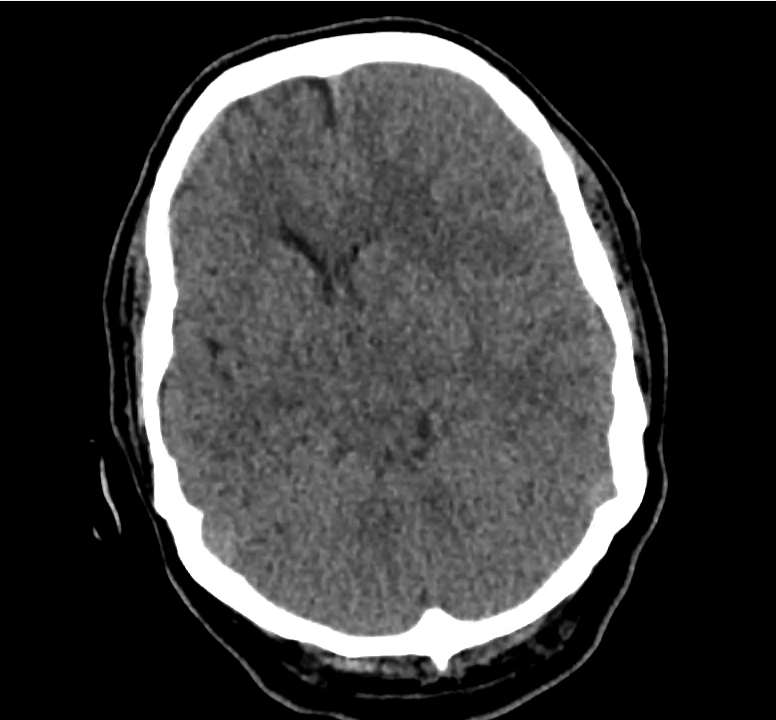
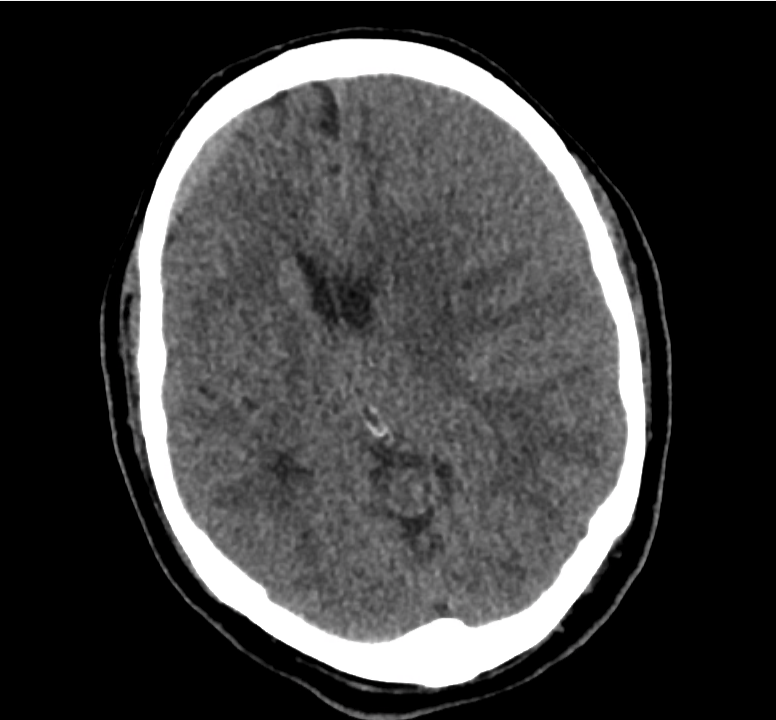
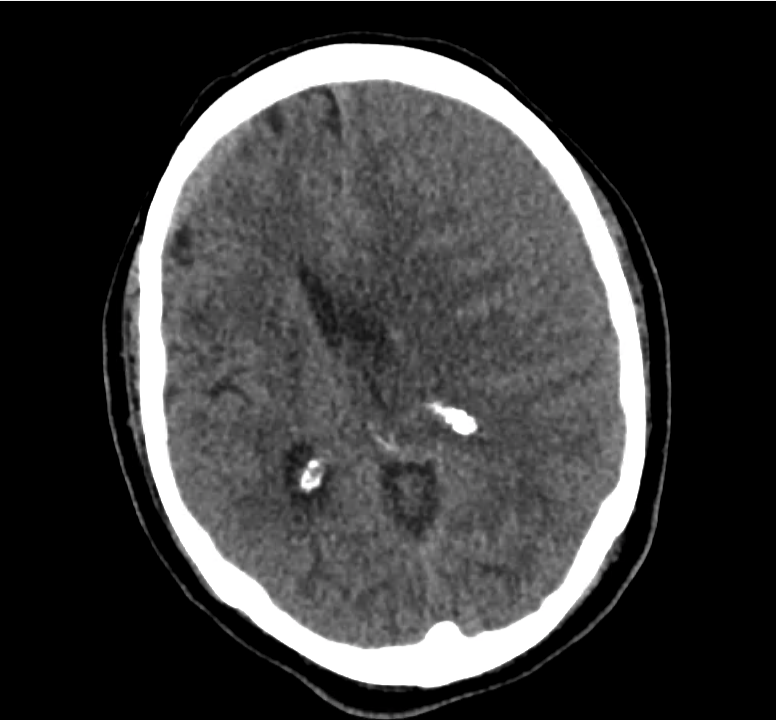
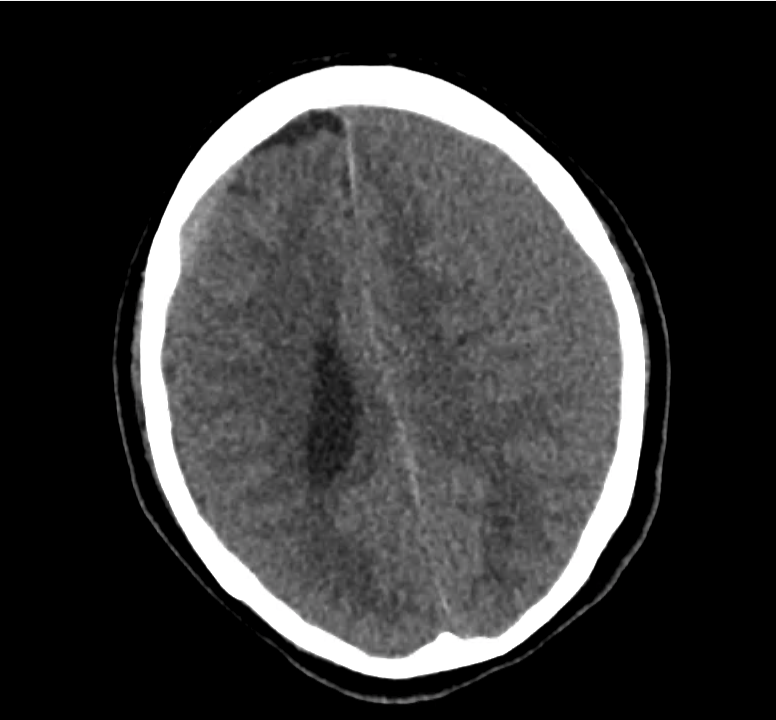
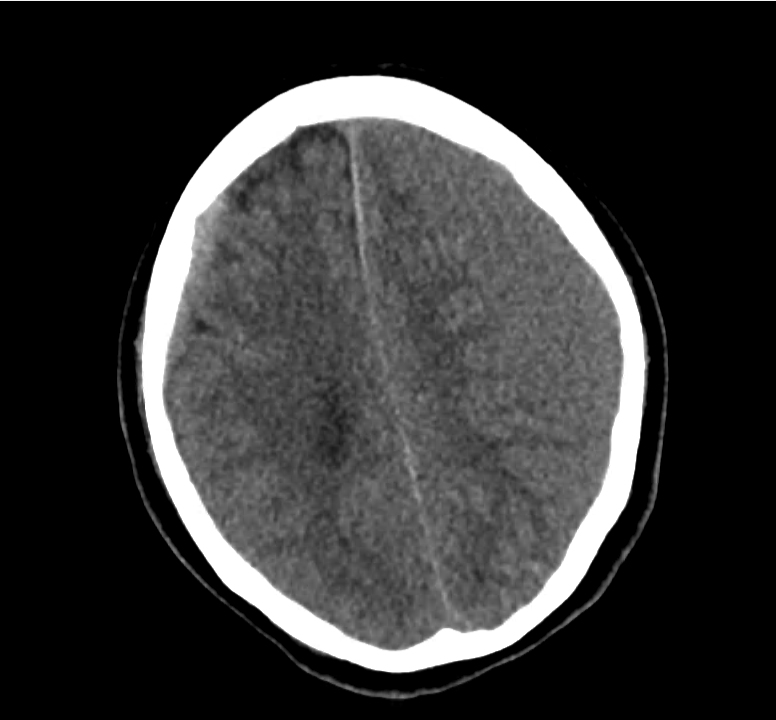
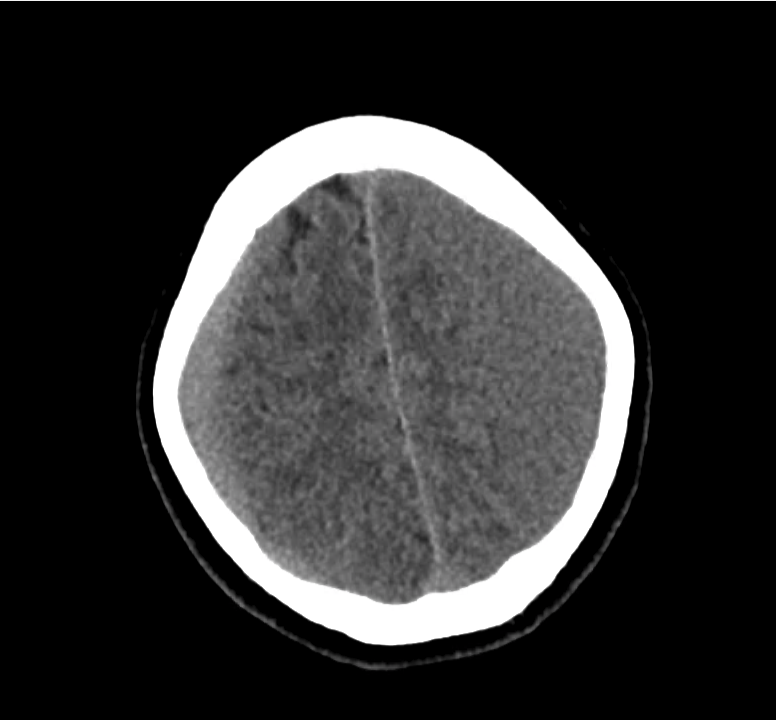
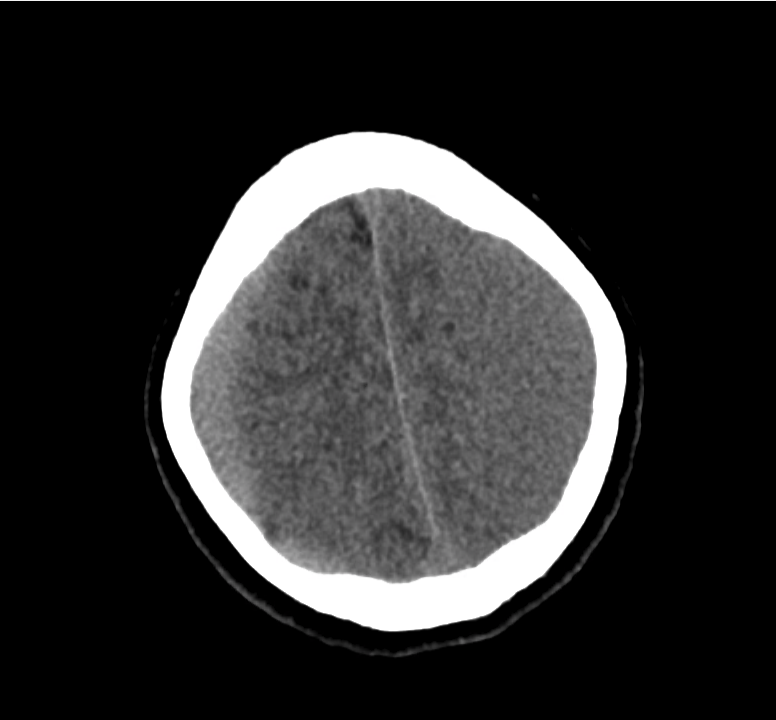
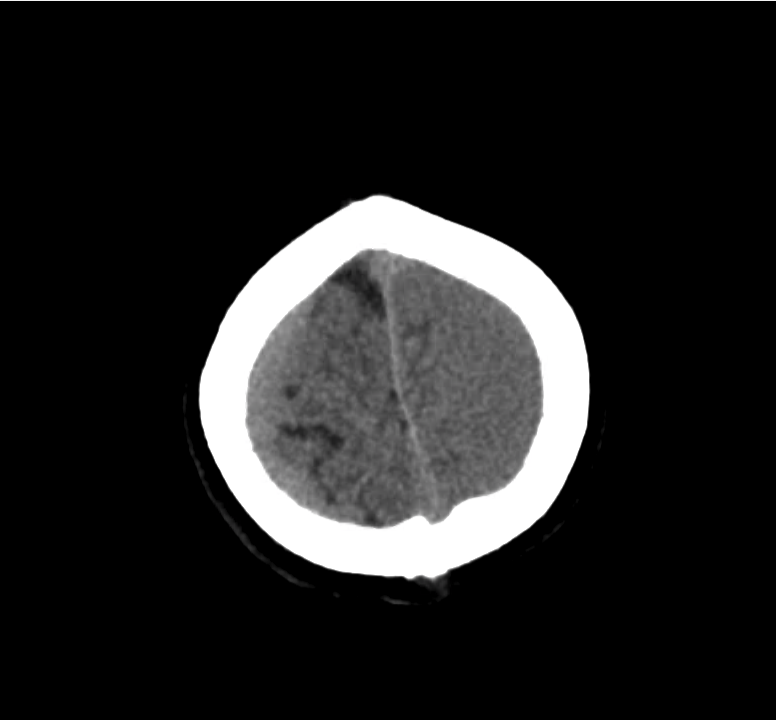
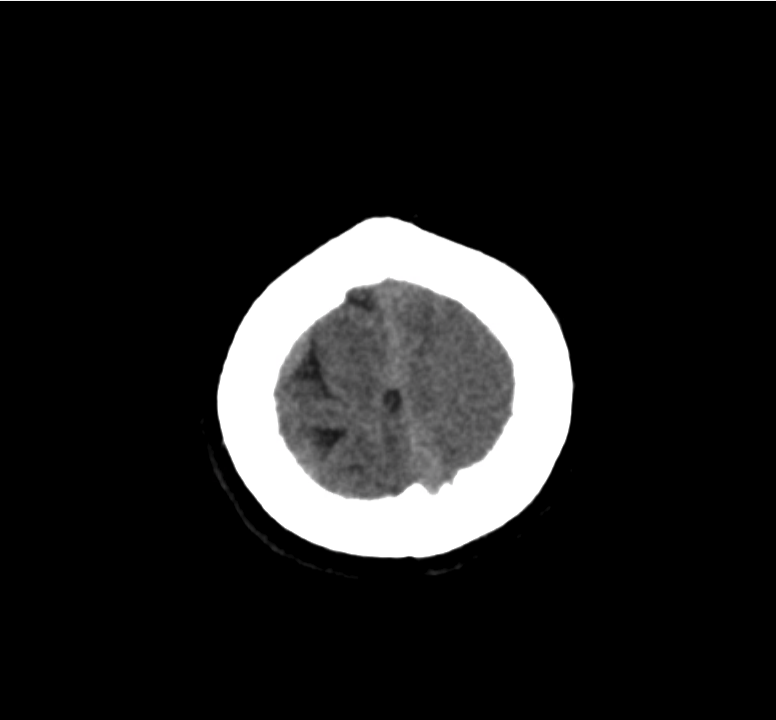
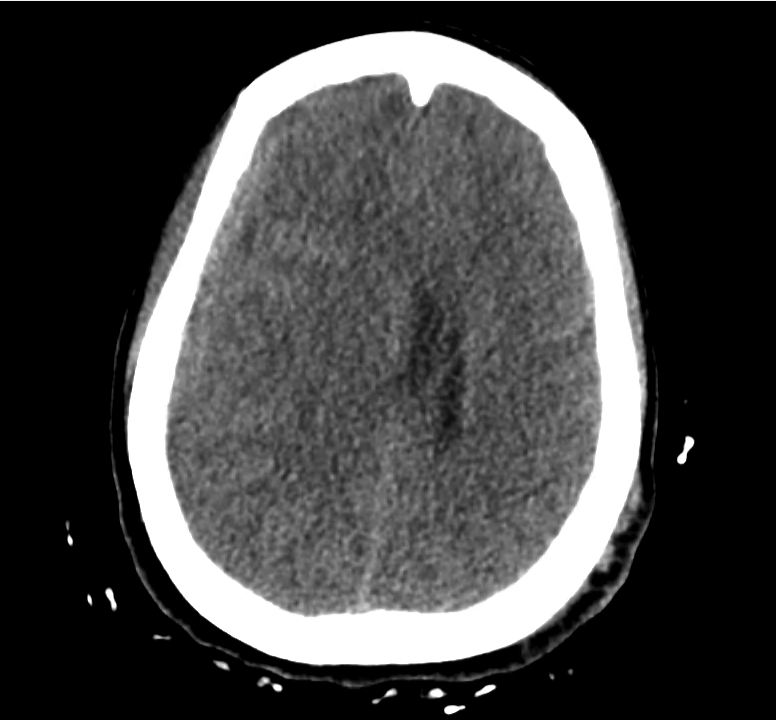
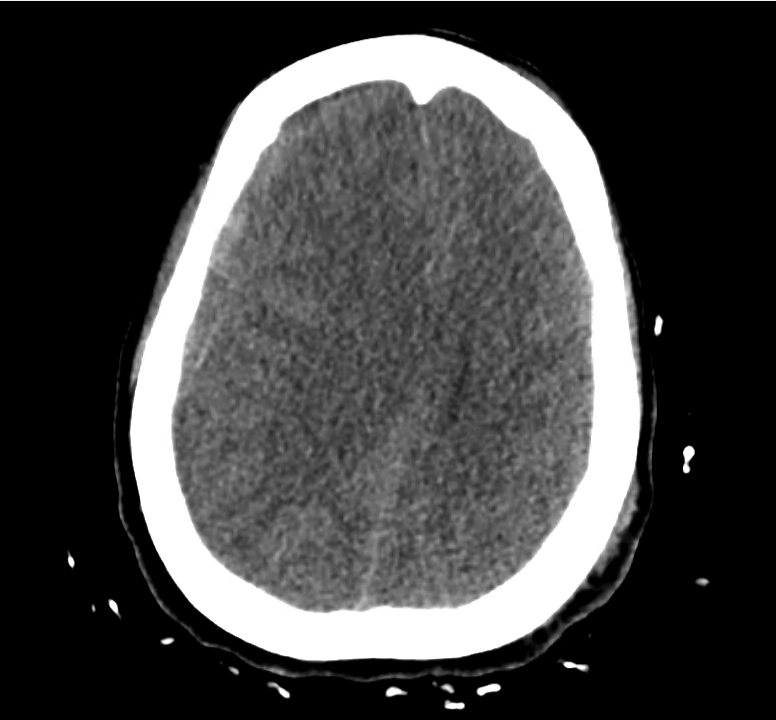
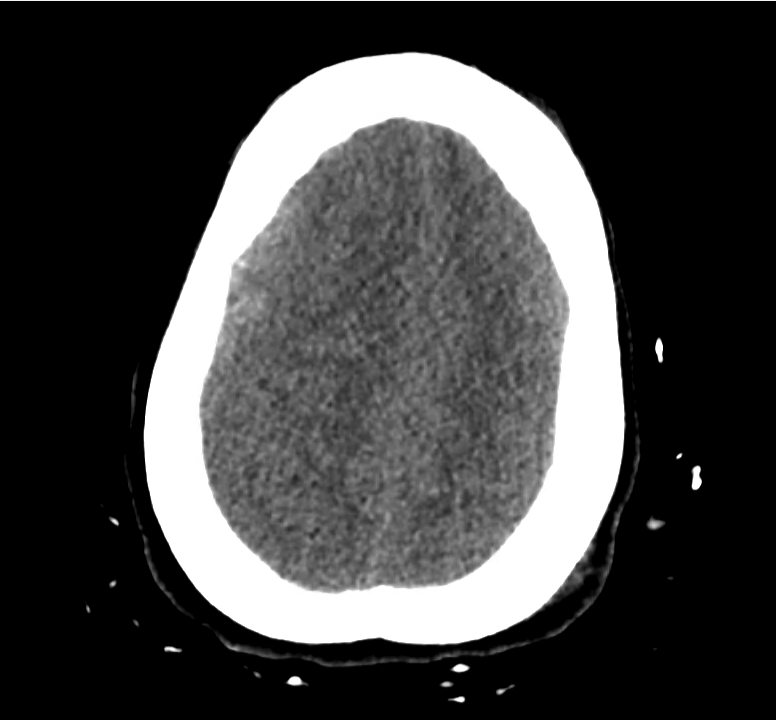
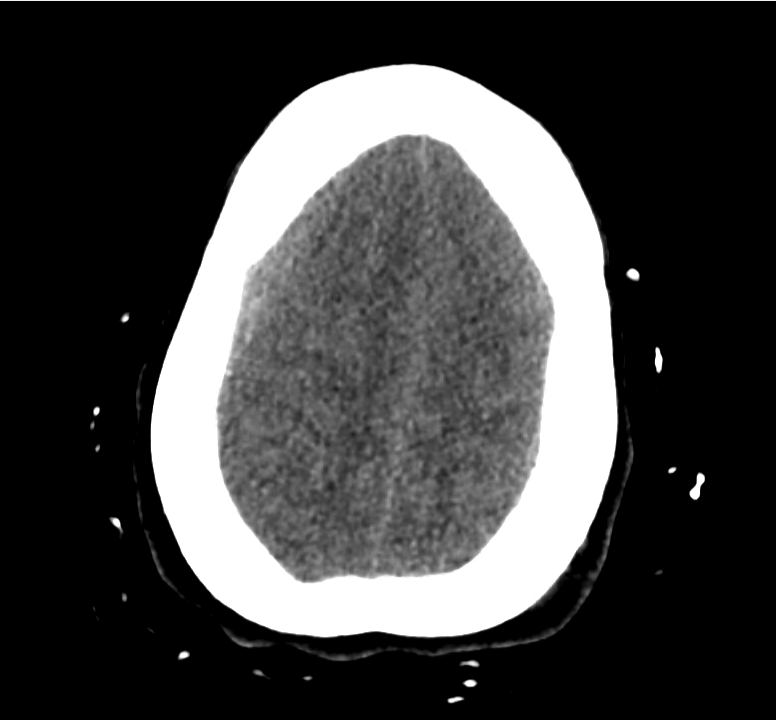
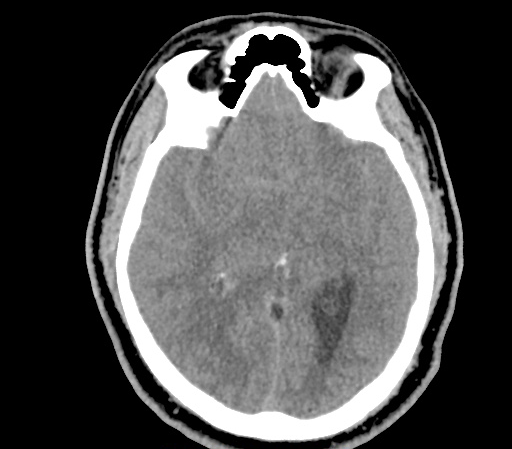
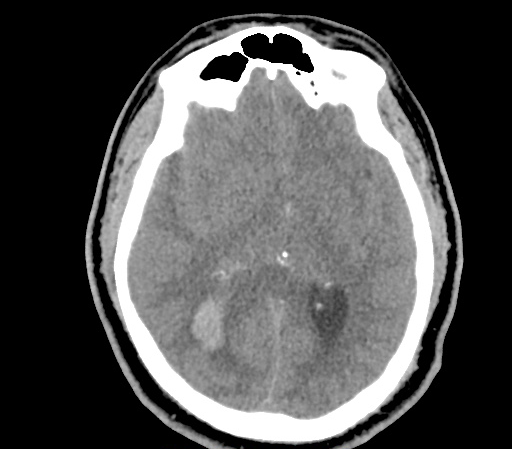
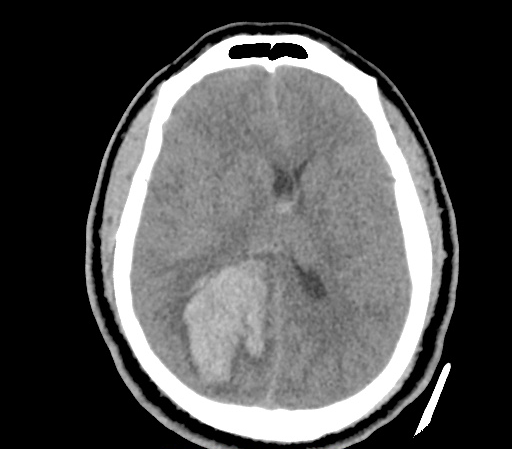
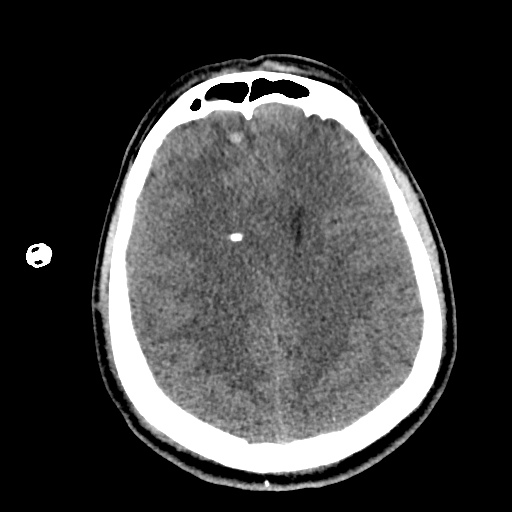
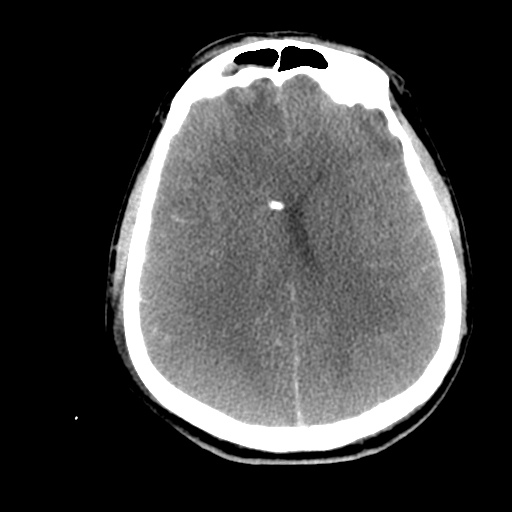
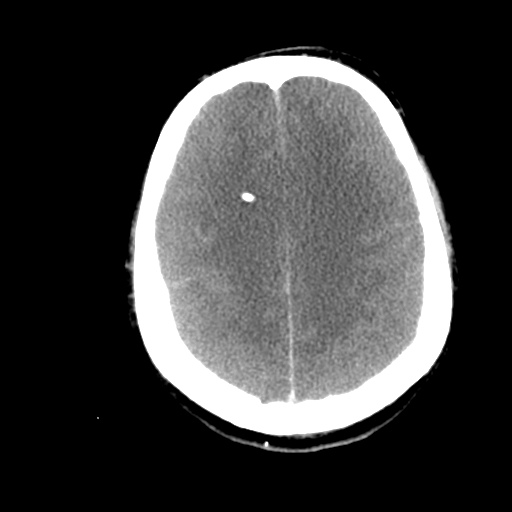
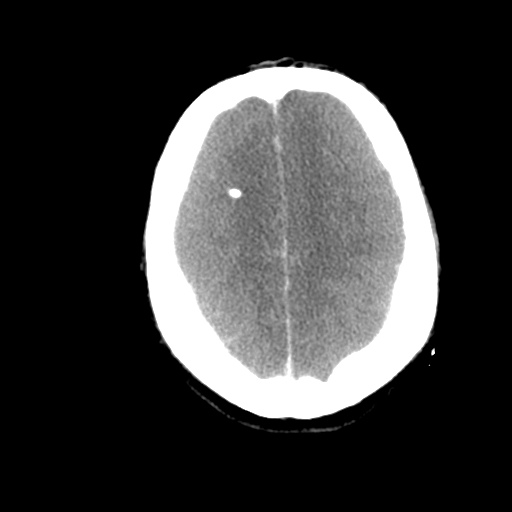
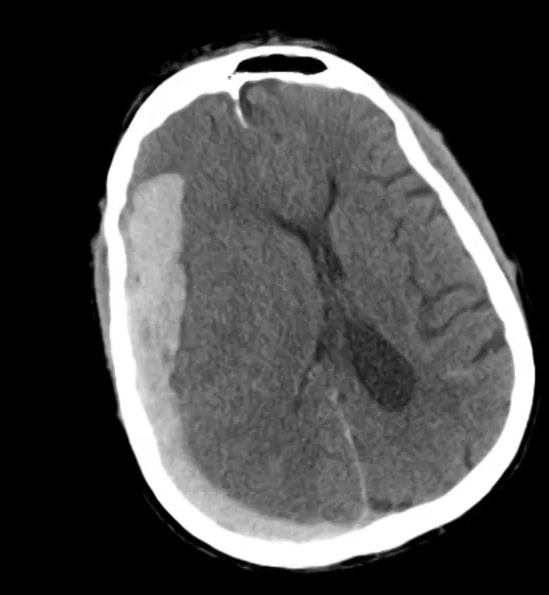
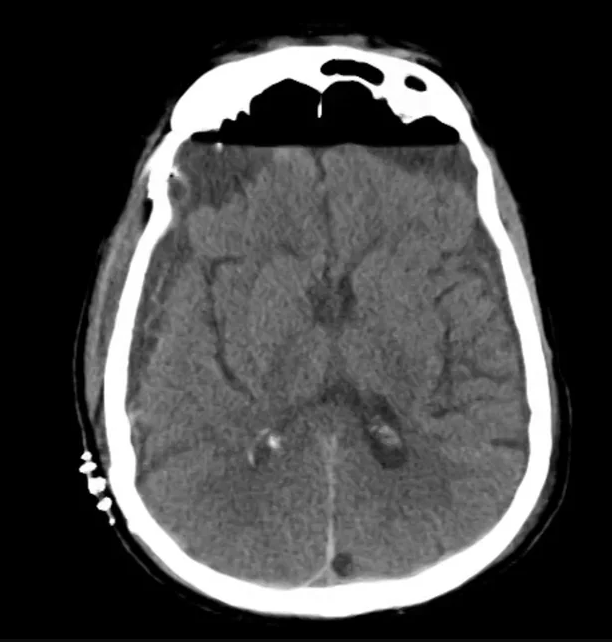
Example #2
CT Head Interpretation
- Bilateral subacute subdural hematomas, left larger than right and associated with rightward midline shift.
- Left lateral ventricle is partially effaced.
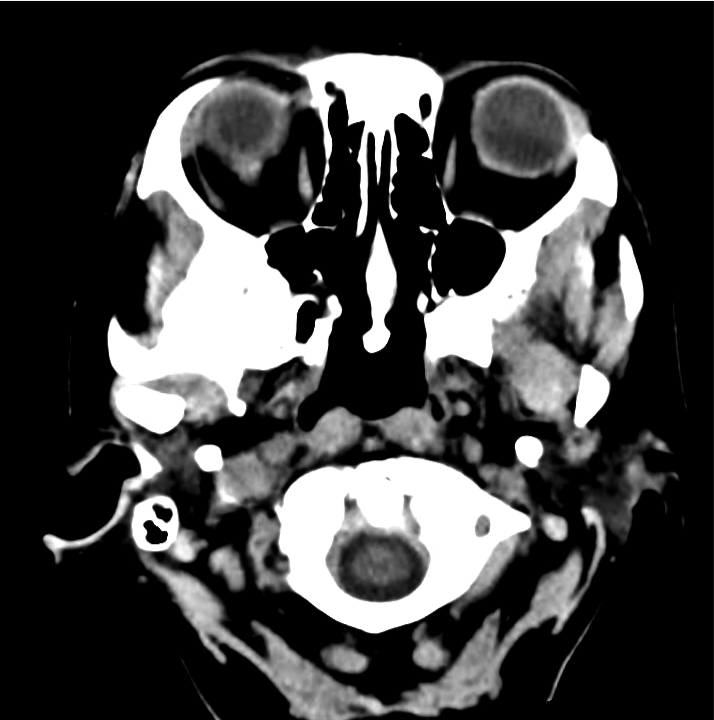
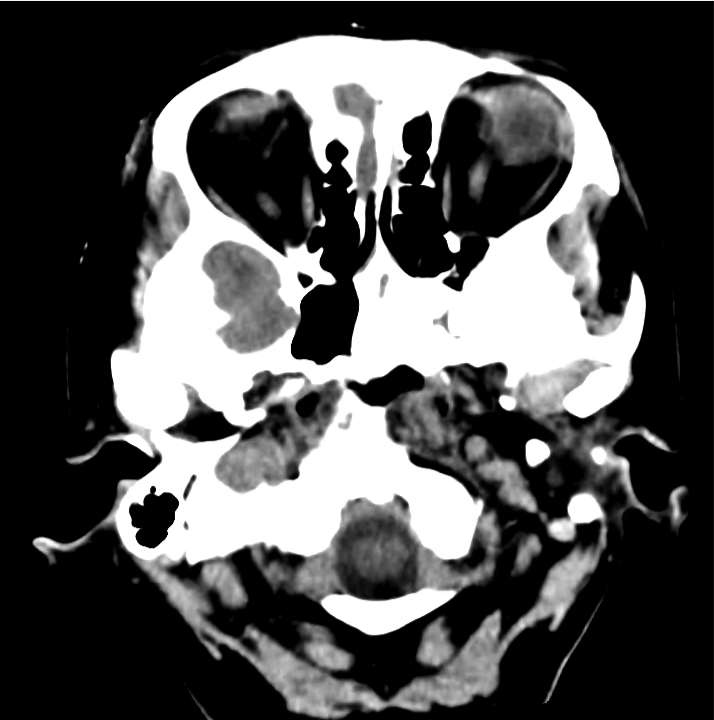
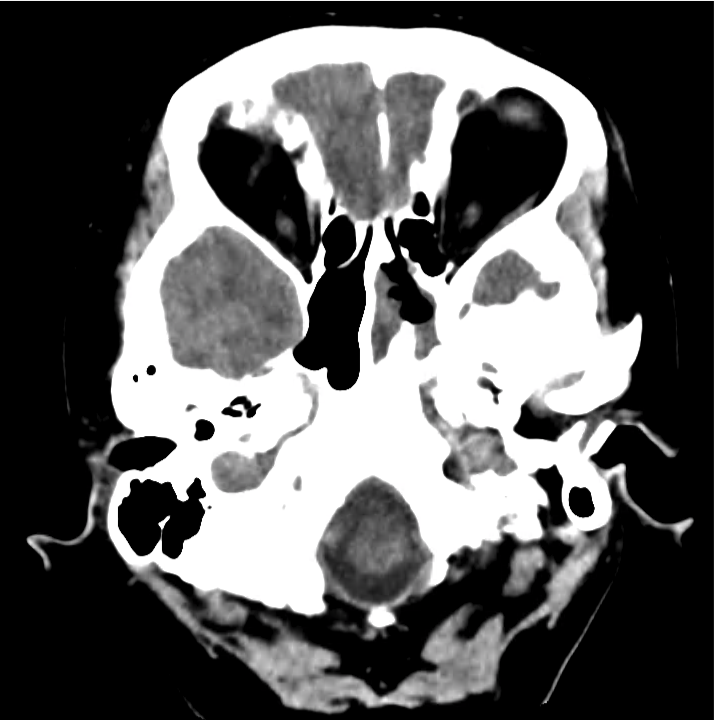
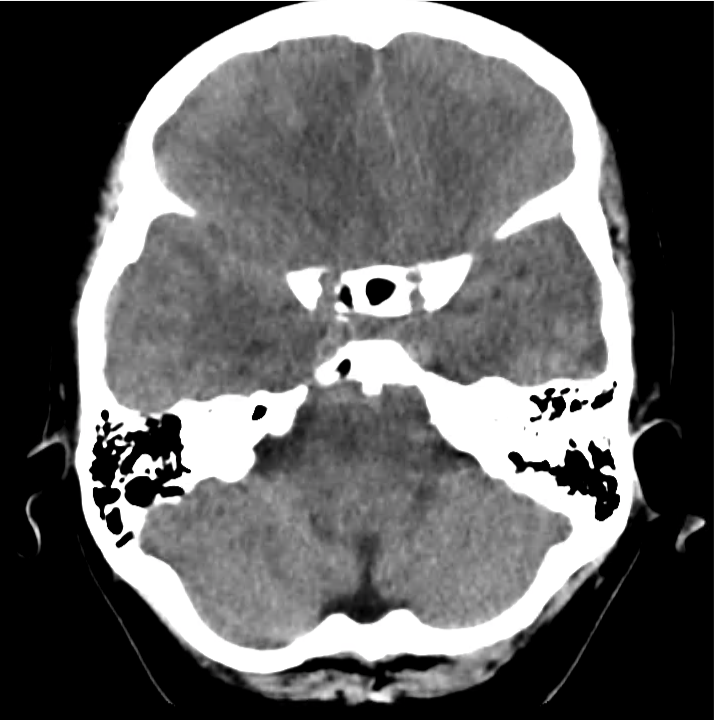
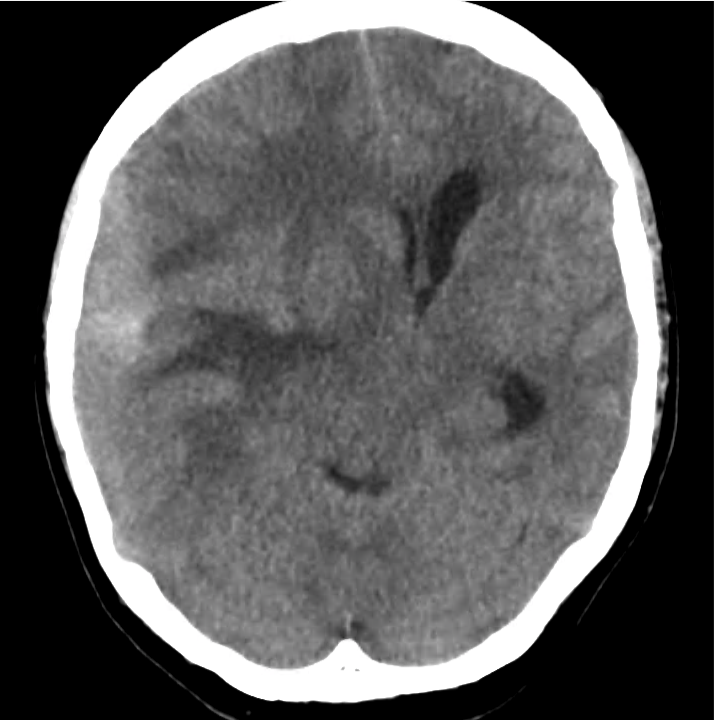
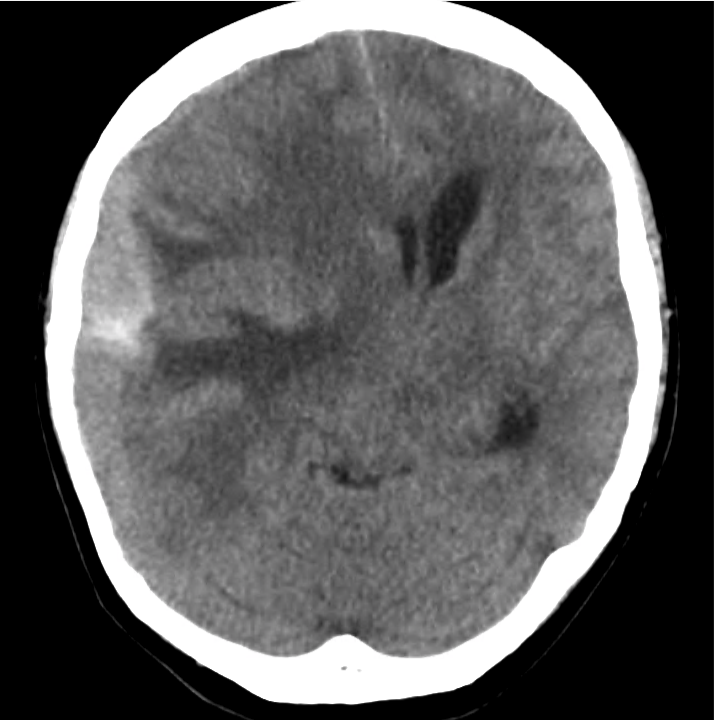
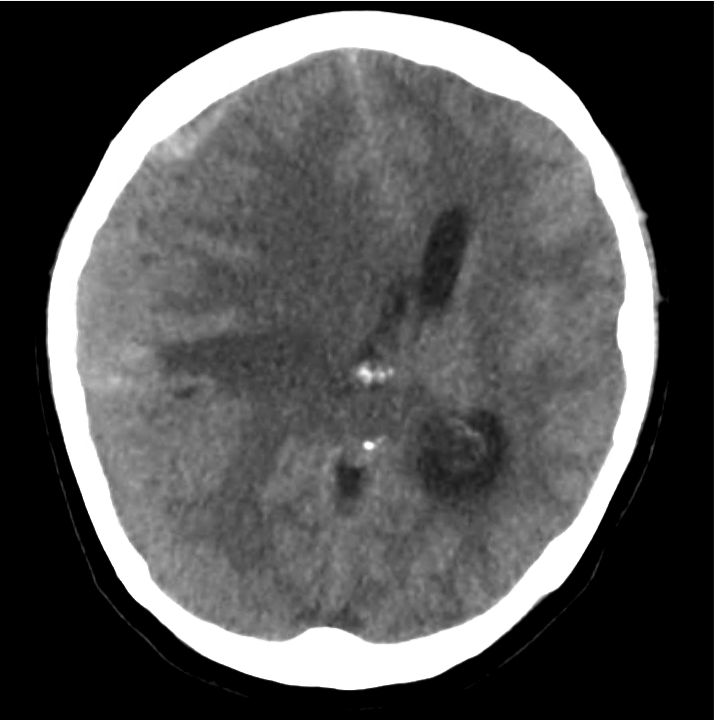
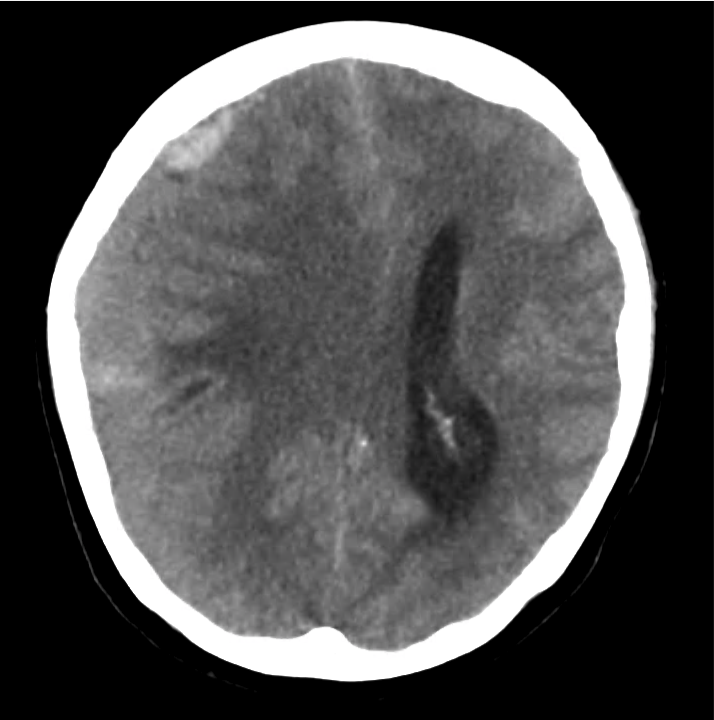
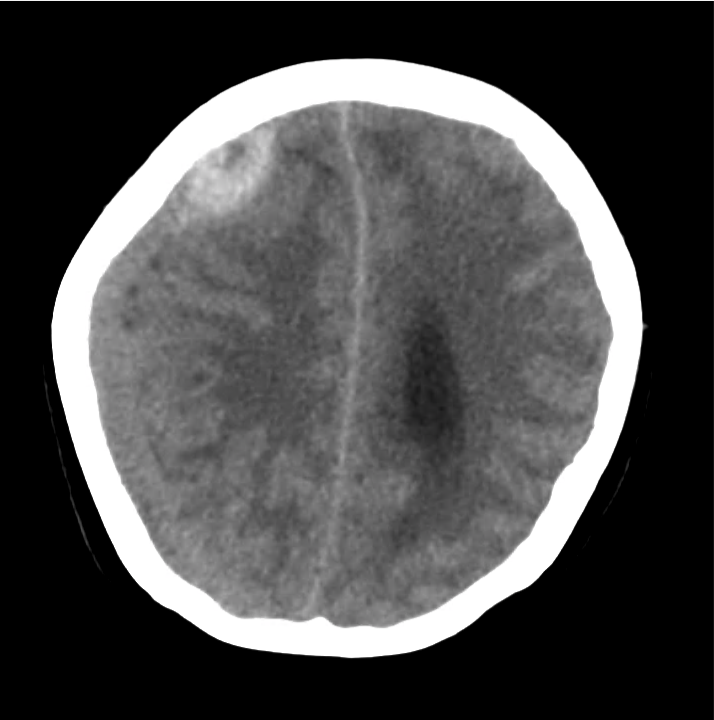
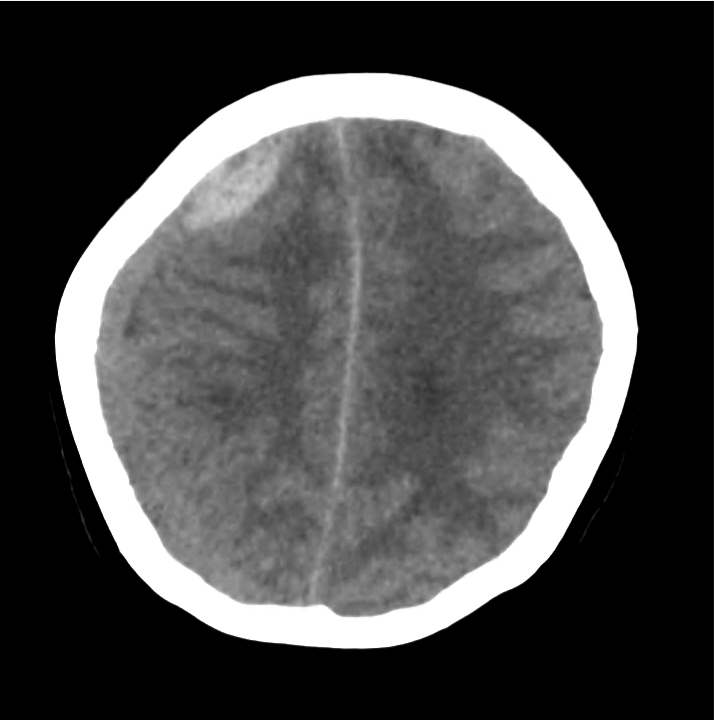
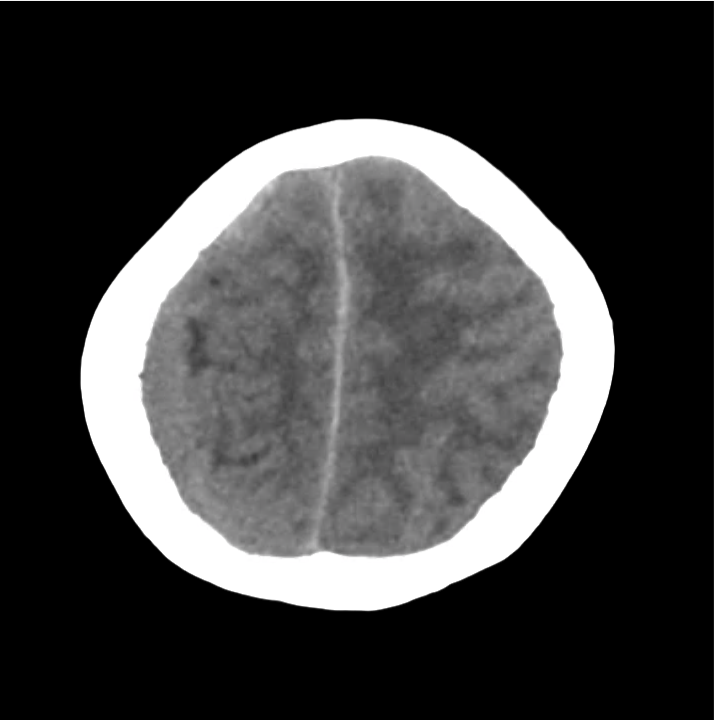
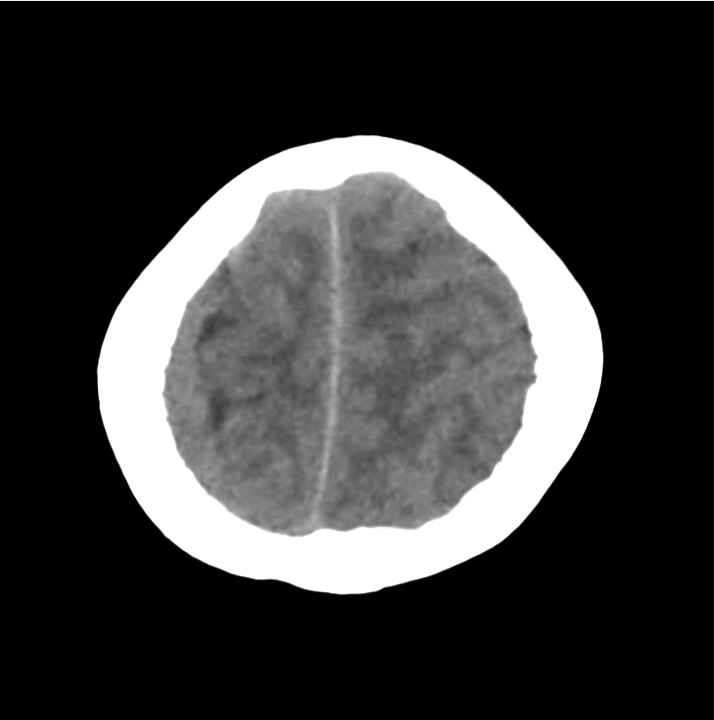
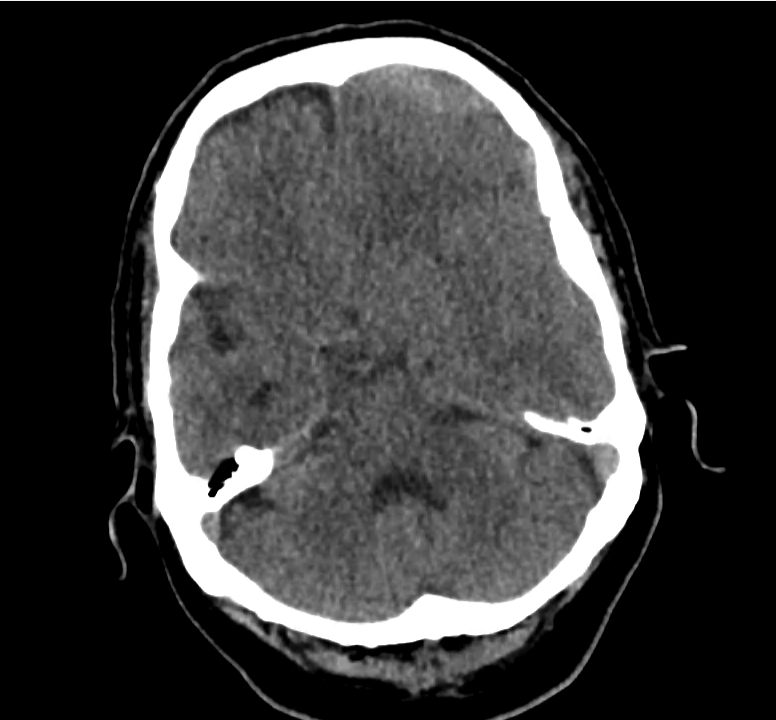
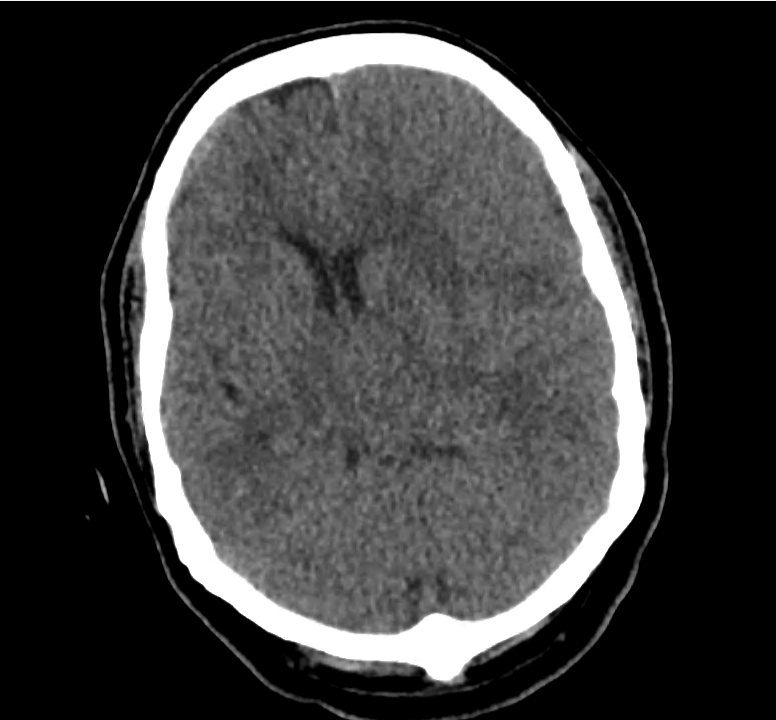
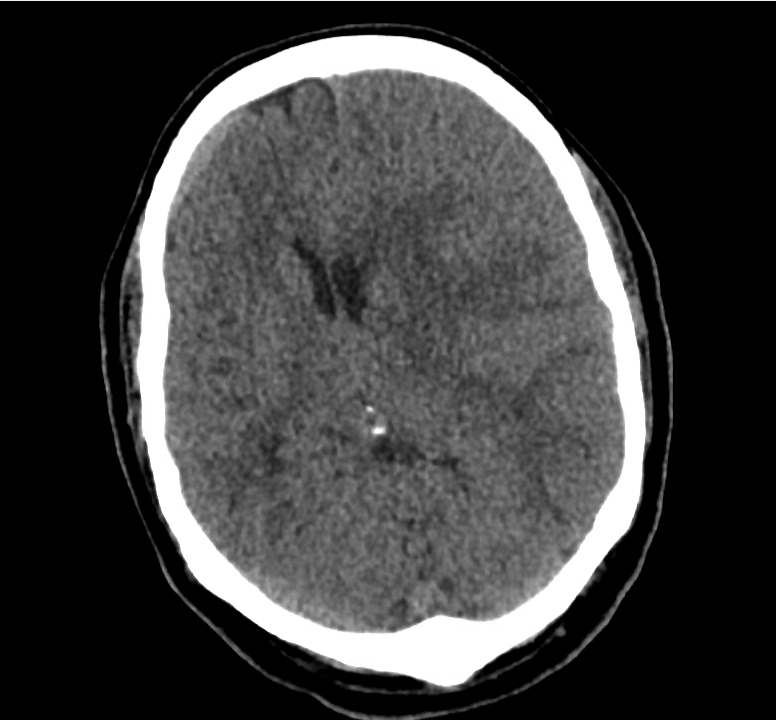
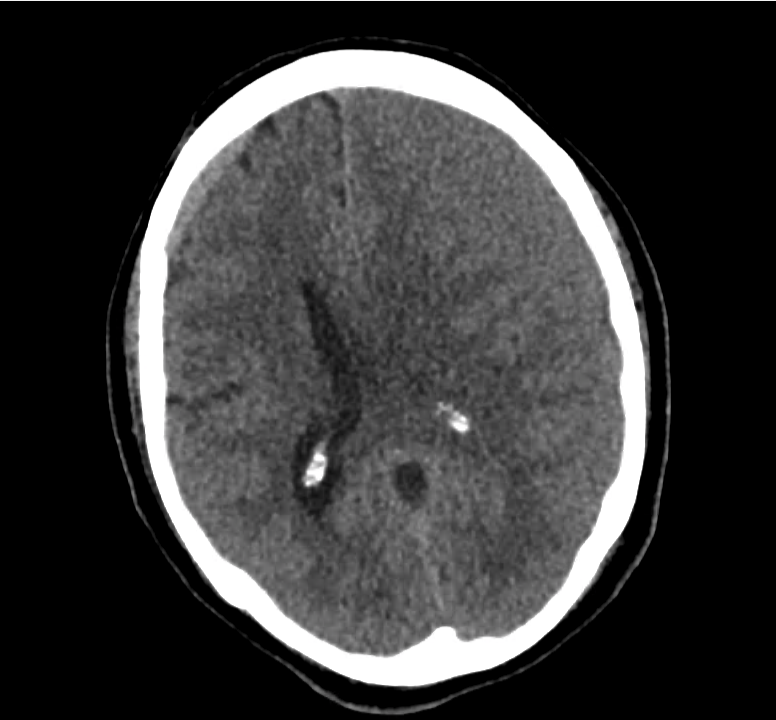
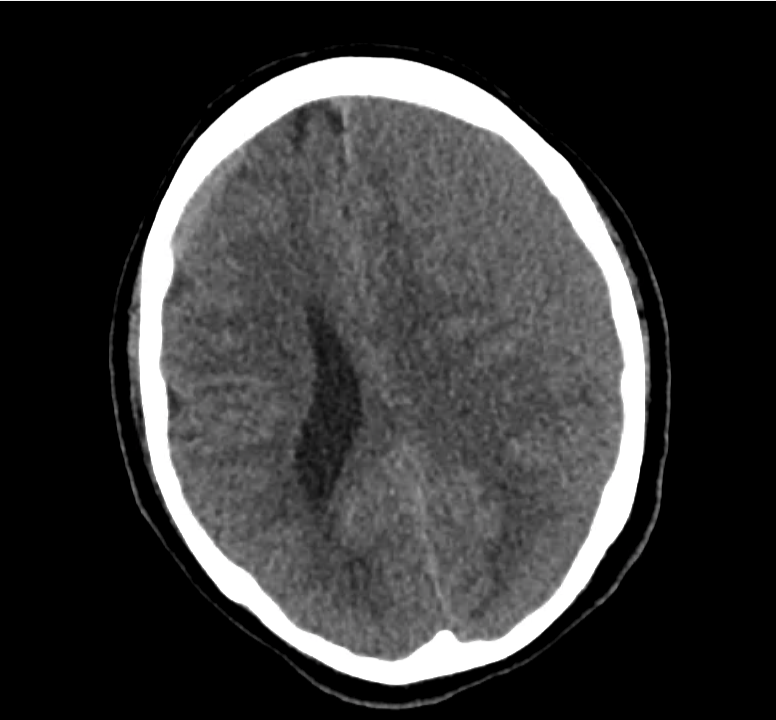
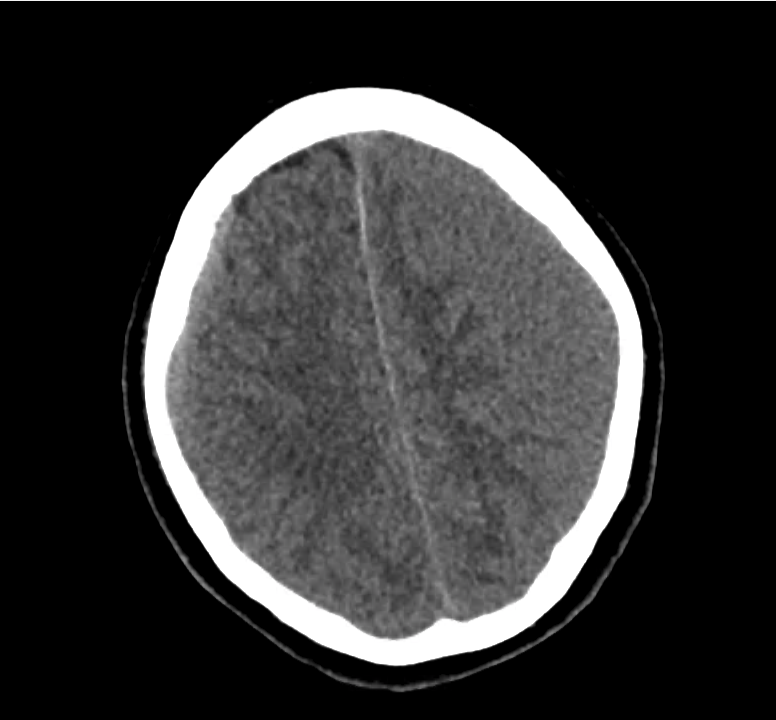
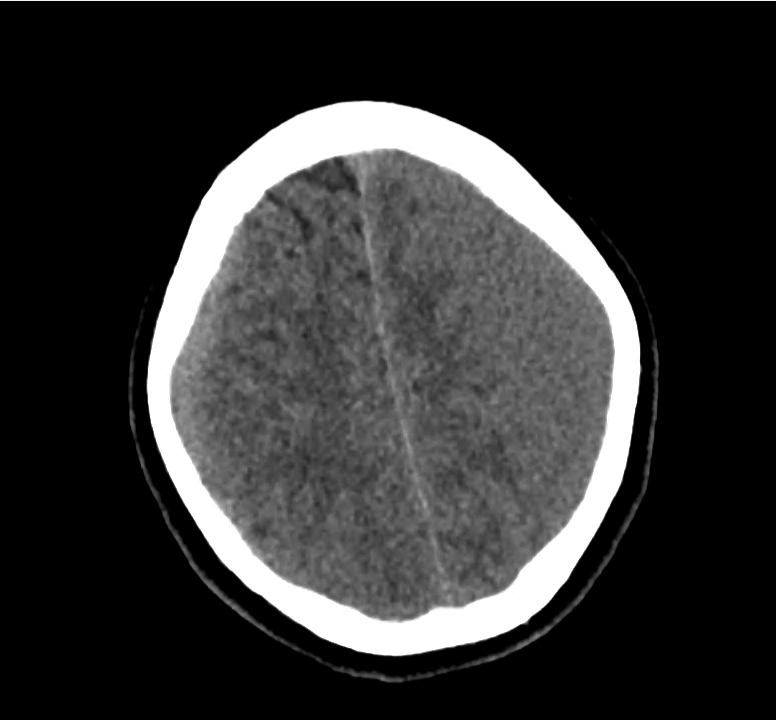
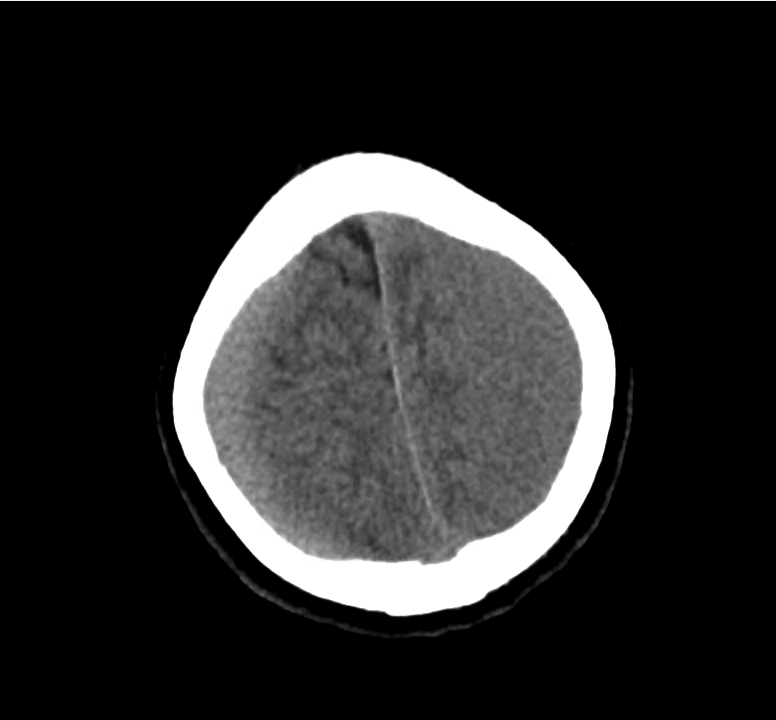
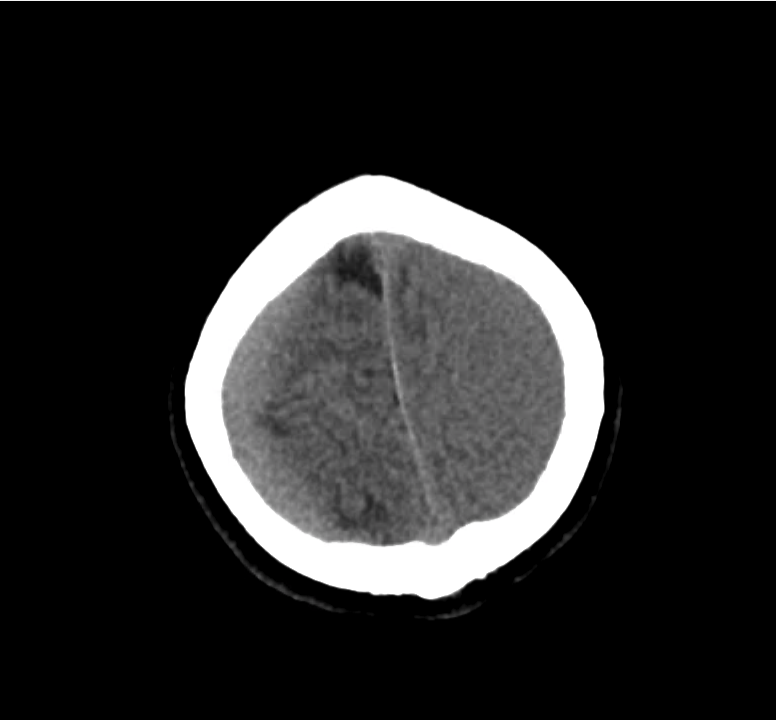
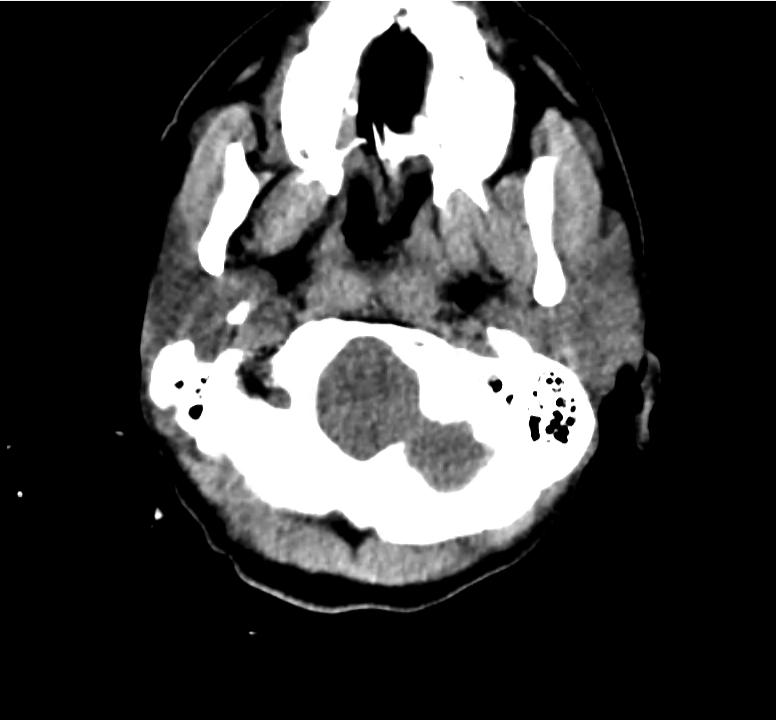
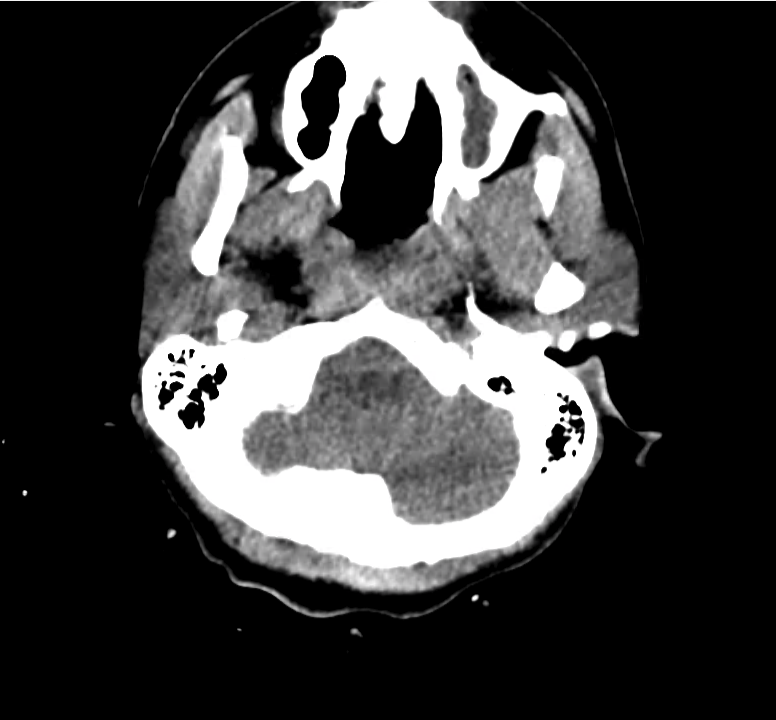
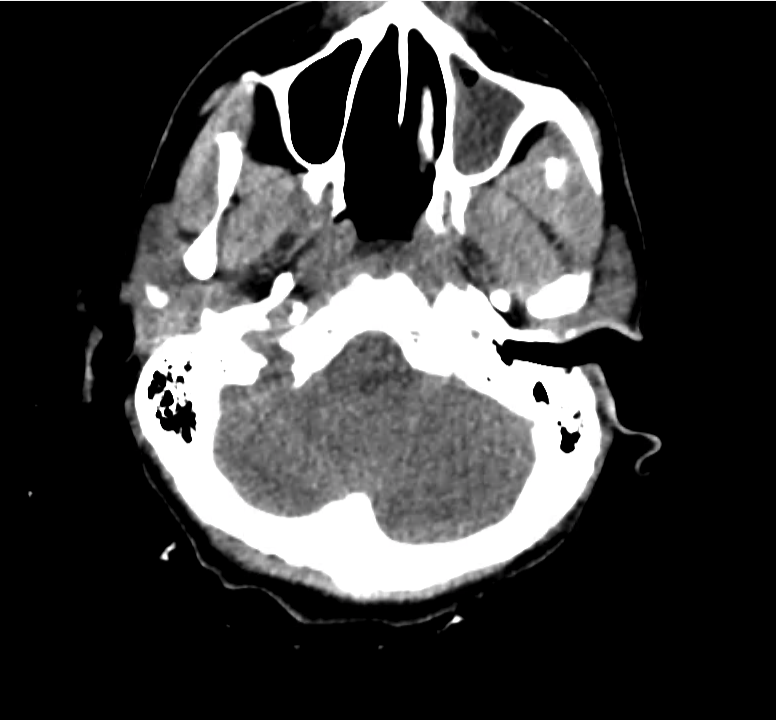
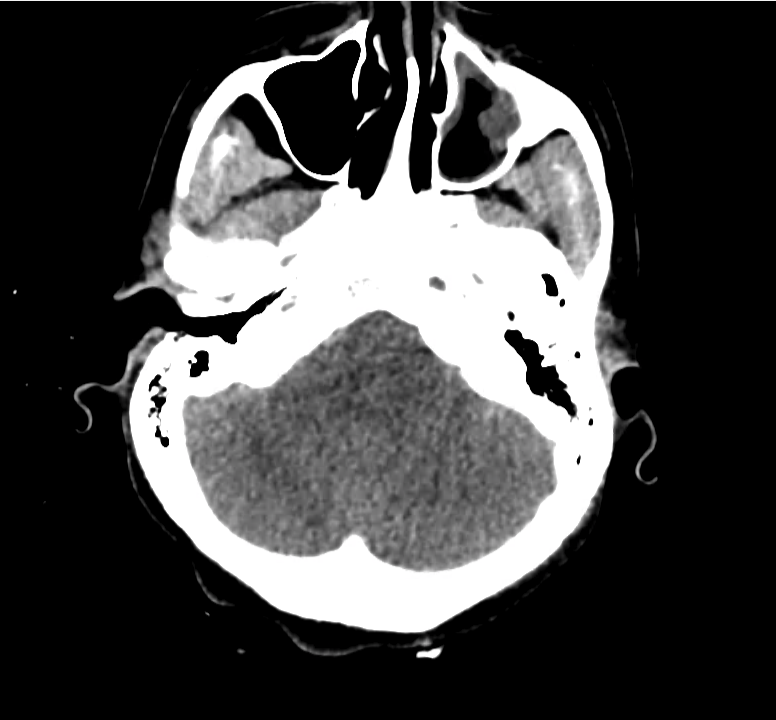
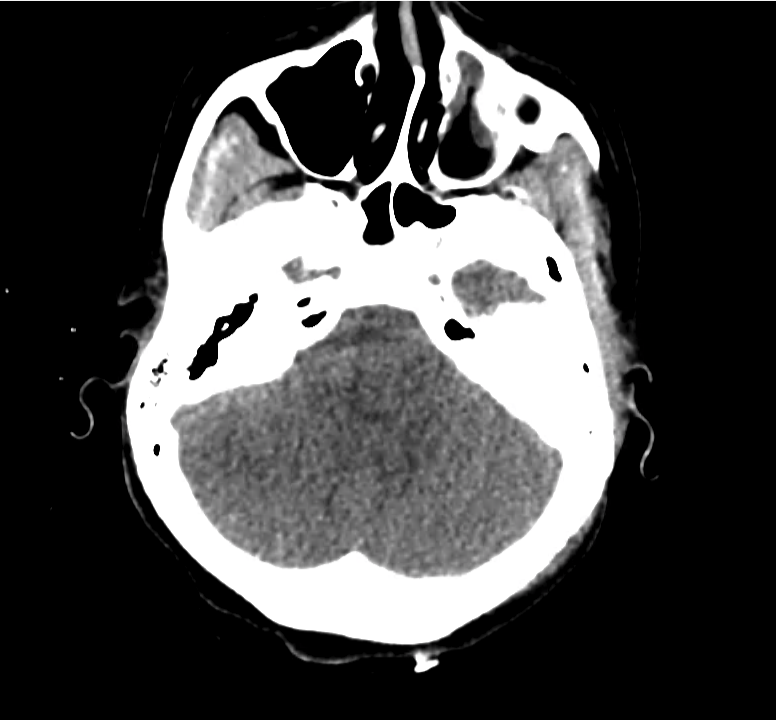
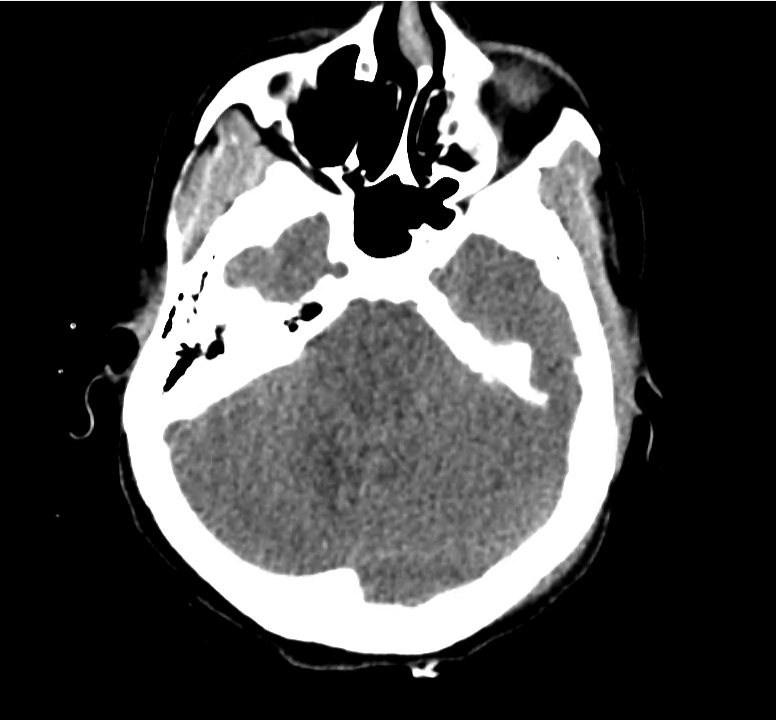
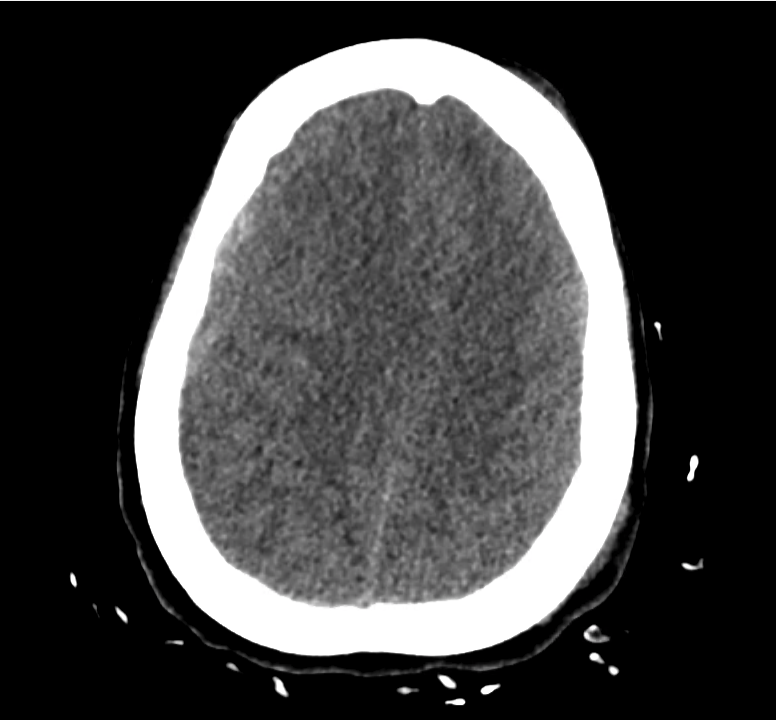
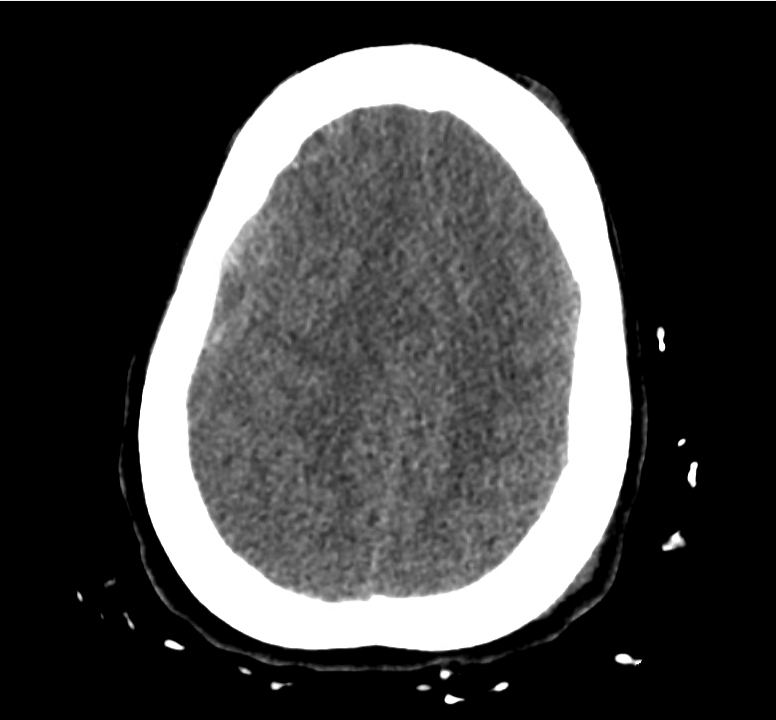
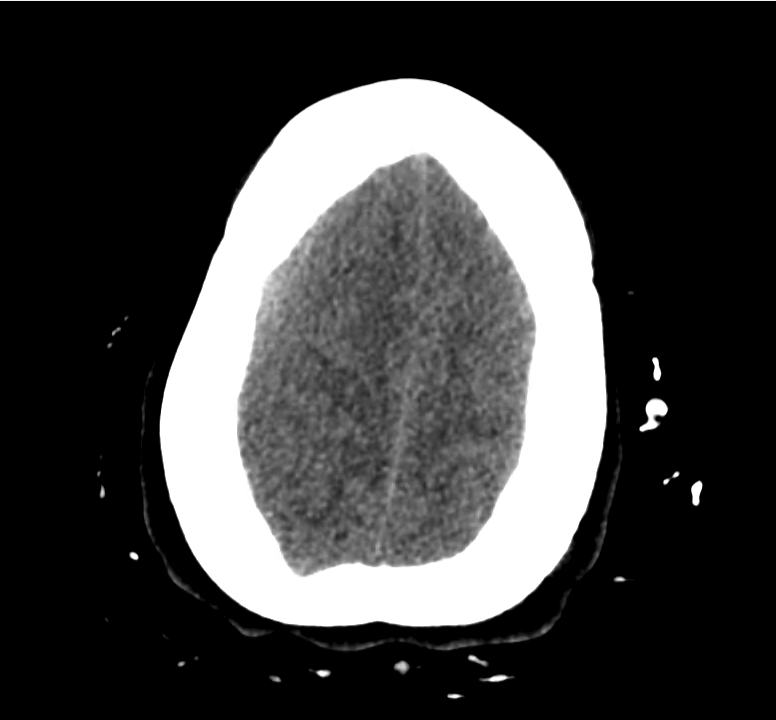
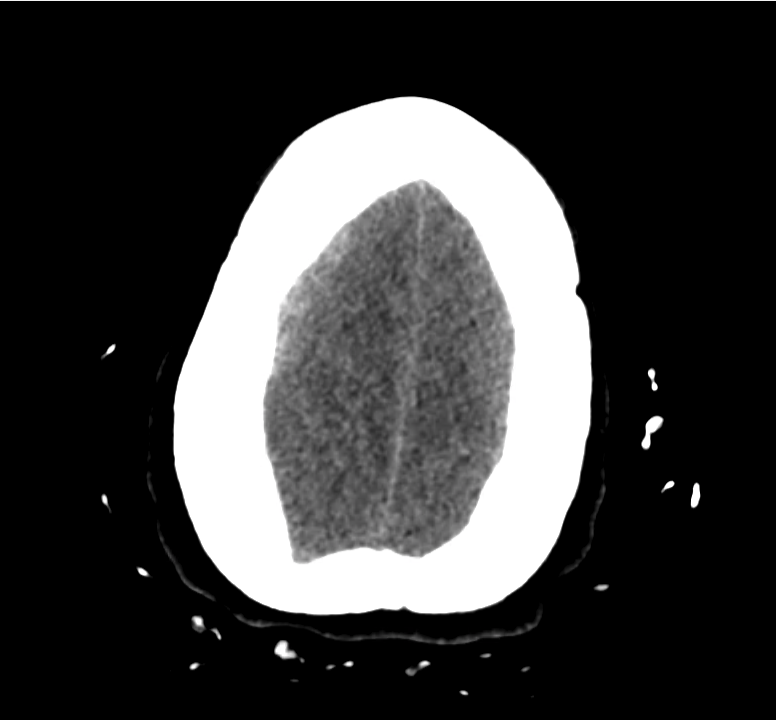
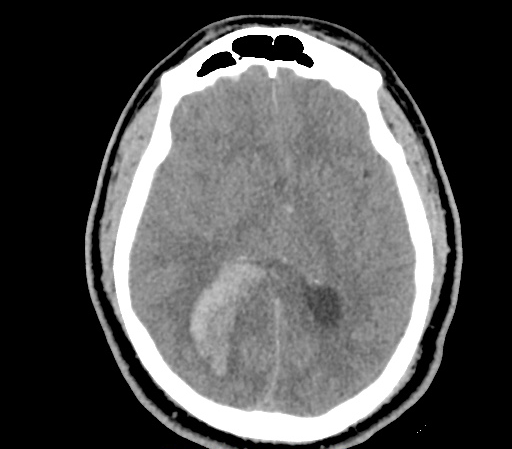
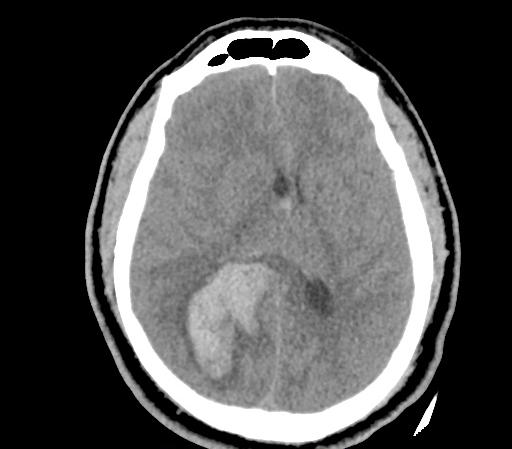
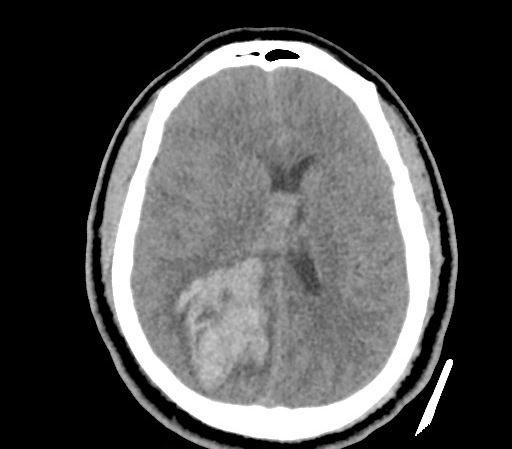
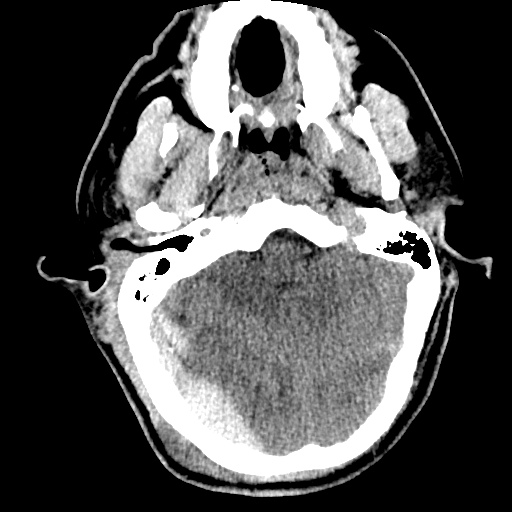
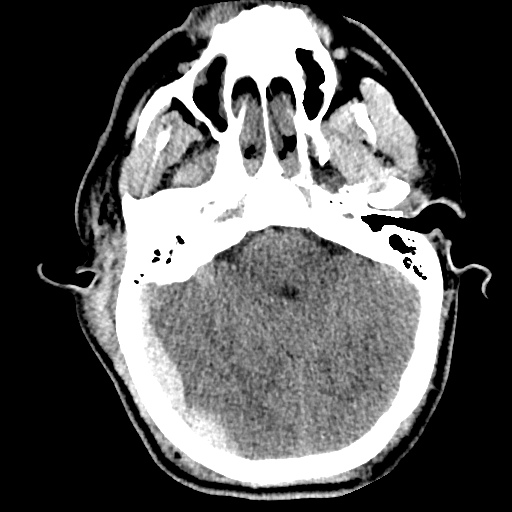
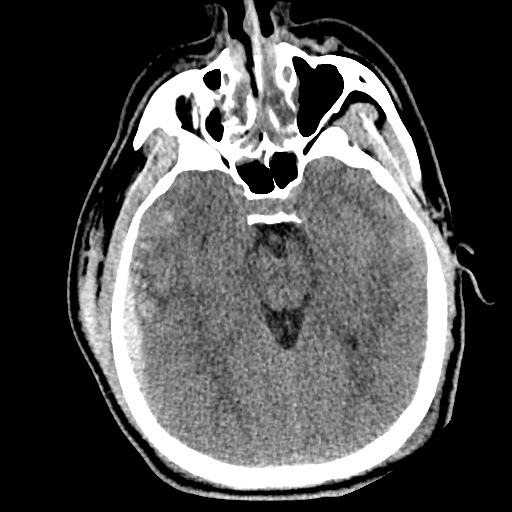
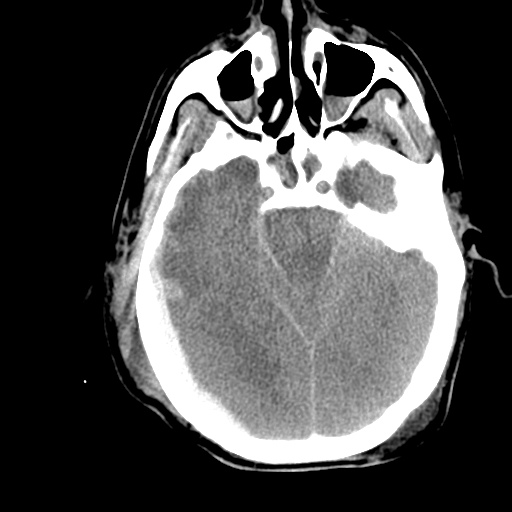
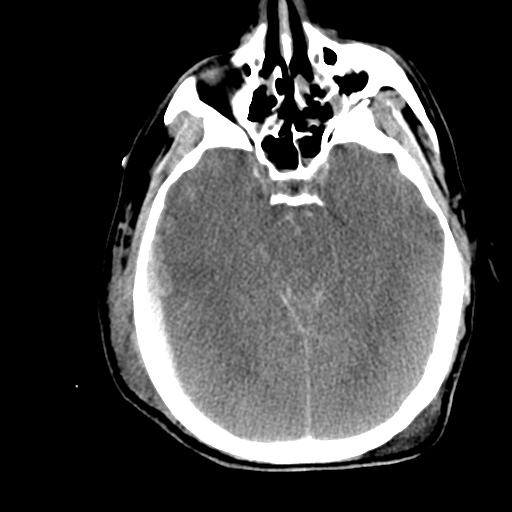
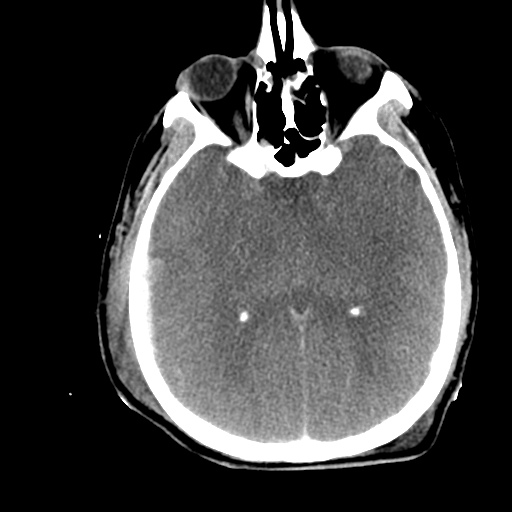
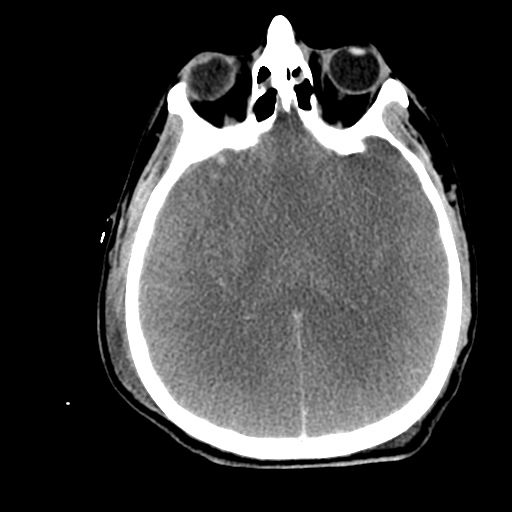
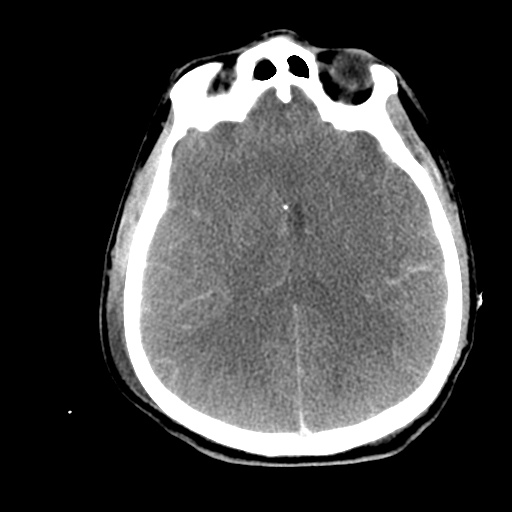
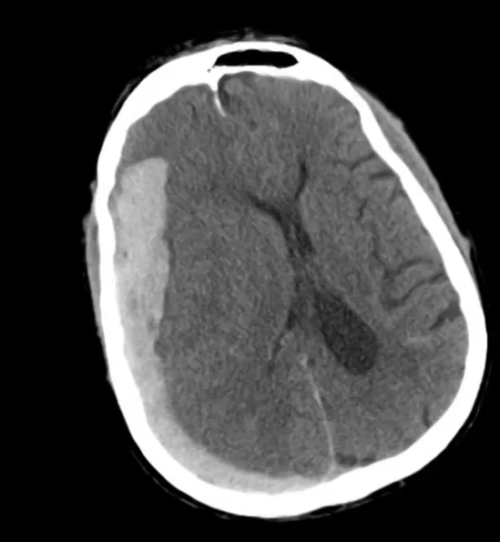
Example #3
CT Head Interpretation
Subdural hematoma with significant herniation
References
- Perron A. How to read a head CT scan. Emergency Medicine. 2008.
- Arhami Dolatabadi A, Baratloo A, Rouhipour A, et al. Interpretation of Computed Tomography of the Head: Emergency Physicians versus Radiologists. Trauma Mon. 2013;18(2):86–89. doi:10.5812/traumamon.12023.































 ID:
ID: