 ID:
ID:
17 year-old female presenting to the pediatric ED with sore throat for 2 days.
HPI:
The patient reports steadily worsening sore throat over the past 2 days, associated with a sensation of swelling. The pain is described as sharp, 4/10 in severity, located on the left side of her throat, and worsened with swallowing. She denies inability to swallow or difficulty breathing, she also denies fever, cough, new skin rashes or genital lesions.
She has no PMH/PSH, takes no medications, denies t/e/d use and is not currently sexually active.
PE:
- VS: 111/65mmHg, 80bpm, 97.8°, 16/min, 100% RA
- Gen: Well-appearing, NAD
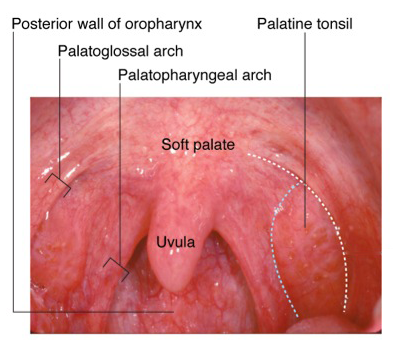
- HEENT: PERRL, no conjunctival injection, TM clear b/l, minimal pharyngeal erythema on left with 6mm white circular lesion on left tonsil, no tonsillar enlargement, no uvular deviation, no cervical LAD, neck supple no masses, normal neck ROM
- CV: RRR, no M/R/G, Lungs: CTAB
- Abdomen: +BS, soft, NT/ND
- Ext: Warm, well-perfused, normal peripheral pulses
Assessment & Plan:
17yo female with no significant PMH with acute pharyngitis for 2 days. The most likely cause of the patient’s symptoms is viral pharyngitis, potentially herpangina (given the appearance of the tonsillar lesion). A more serious viral/bacterial pharyngitis is less likely given the absence of fever or significant erythema/exudate. There was no uvular deviation to suggest peritonsillar abscess and no evidence of airway obstruction to suggest other acute processes (epiglottitis, retropharyngeal abscess). The plan is to recommend supportive care and ibuprofen for symptomatic relief. The patient will be discharged home in good condition with precautions to return if symptoms worsen or she begins to have difficulty swallowing/breathing.
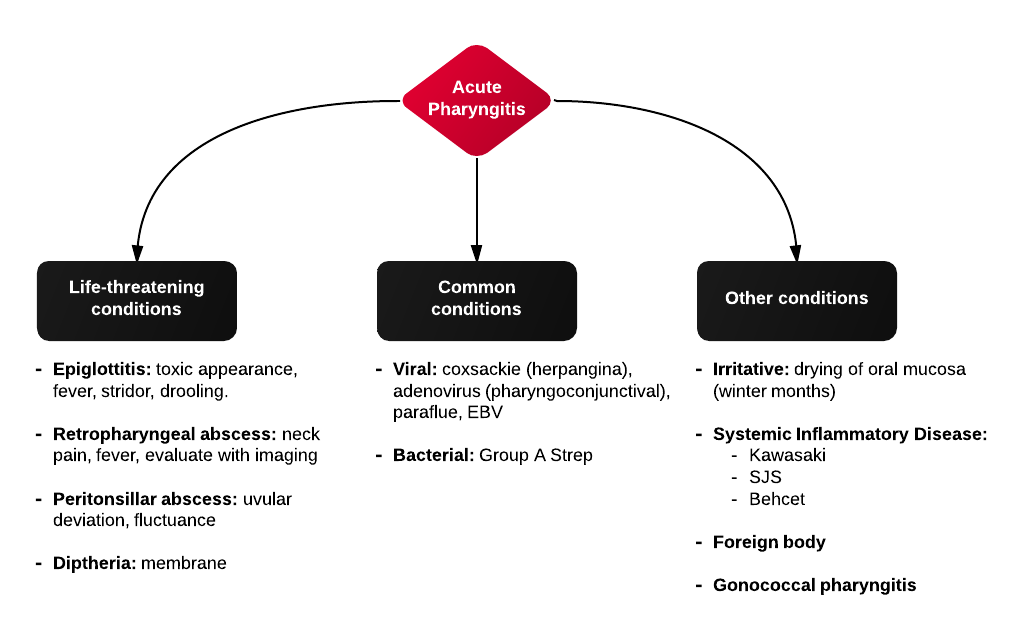
Differential Diagnosis of Acute Pharyngitis:
Evaluation (history):
- Respiratory distress: epiglottitis, retropharyngeal abscess, peritonsillar abscess, EBV (obstruction in or near pharynx)
- Fatigue: infectious mononucleuosis
- Abrupt onset: epiglottitis
Evaluation (physical examination):
- Vesicles anterior: herpetic stomatitis, SJS, Behcet
- Vesicles posterior: herpangina (± involvement of extremities)
- Asymmetry: peritonsillar abscess
- Stridor, drooling, respiratory distress: airway obstruction
- Generalized inflammation: Kawasaki