 ID:
ID:
14 year-old female, previously healthy, brought in by ambulance s/p auto vs. pedestrian.
HPI:
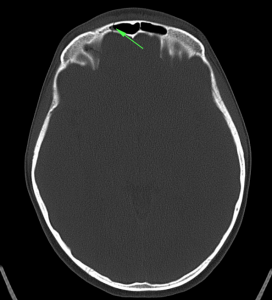
Incident unwitnessed, paramedics report no LOC with GCS 15 at scene. GCS 10 upon arrival to ED, with 2min GTC seizure. Patient intubated for airway protection and CT head showed non-displaced frontal bone fracture and small frontal SAH. Patient self-extubated, returned to baseline mental status and was transferred to PICU.
PE:
- VS: 128/76mmHg, 120bpm, 22 R/min, 100% RA, 37.6°C
- General: Alert and responsive young female with multiple bandages on extremities
- HEENT: Right frontal hematoma, no bony defect palpated, multiple facial abrasions, no otorrhea, no rhinorrhea, TM clear b/l, no other ecchymosis.
- CV: RRR, normal S1/S2, no M/R/G
- Lungs: CTAB
- Abdomen: +BS, soft, NT/ND, no rebound/guarding, no flank ecchymoses
- Neuro: AAOx3, CN II-XII intact, sensation/motor/reflexes symmetric and intact.
- Extremities: Well-perfused with good pulses, no focal bony tenderness, no joint effusions, multiple abrasions on extensor surfaces of all four extremities.
Assessment & Plan:
14yo female, previously healthy, s/p auto vs. peds followed by GTC seizure and CT head showing small SAH and non-displaced frontal bone skull fracture. No evidence of basilar skull fracture on examination or imaging. Seizure likely 2/2 irritation from SAH. Patient was followed closely in PICU with q1h neuro checks with low threshold for repeat CT if change in mental status or more seizures occurred. The patient was eventually transferred to the general ward and was discharged with neurology follow-up and Keppra for seizure prophylaxis for 6mo.

