 HPI:
HPI:
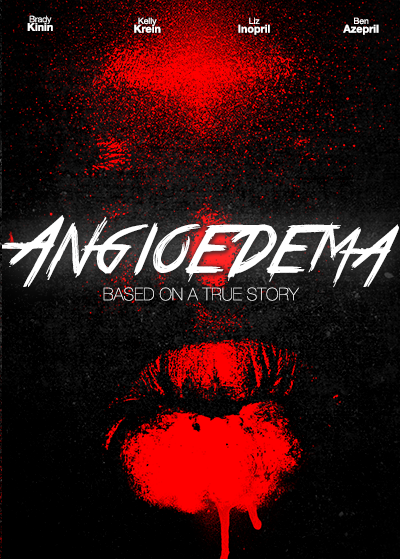
63-year old African American male with a history of HTN presenting with lip swelling x1 day. The patient states he was well until this morning when he noticed progressive swelling of his lips. The swelling is not associated with any difficulty speaking, swallowing or breathing and is not painful.
He denies new rashes or itching, and has no history of such swelling. He also denies any exposure to known allergens, recent insect bites or travel. He has been taking lisinopril for his blood pressure regularly for the past several months and denies any prior adverse effects (cough, rash).
PMH:
- Parkinson Disease
- HTN
PSH:
None
FH:
No family history of angioedema
SHx:
- No t/e/d use
- Lives at home with caretaker
Meds:
- Lisinopril 20mg p.o. daily
- Carbidopa/levodopa 50mg p.o. t.i.d.
Allergies:
NKDA
Physical Exam:
| VS: | T 37.8 HR 84 RR 14 BP 146/98 O2 99% RA |
| Gen: | Well-appearing, no respiratory distress, speaking comfortably |
| HEENT: | PERRL, significant external upper/lower lips swelling extending to lateral cheeks, non-tender, no fluctuance or overlying skin changes. No visible tongue swelling, floor of mouth swelling/tenderness, uvular/palatal deviation. |
| CV: | RRR, no M/R/G |
| Lungs: | CTAB, no crackles/wheezing, good air movement b/l |
| Abd: | +BS, soft, NT/ND, no rebound/guarding |
| Ext: | Warm, well-perfused, 2+ peripheral pulses |
| Skin: | No visible skin lesions/rashes |
| Neuro: | AAOx4, CN II-XII intact |
Assessment/Plan:
63M with acute onset, progressive facial swelling. Currently restricted to external lips, with no evidence of airway compromise. Likely ACE inhibitor-induced angioedema given patient is on lisinopril and has no history of hereditary angioedema. Doubt anaphylaxis given no allergies, suspicious exposures or history of pruritus. Doubt infection given afebrile and painless swelling without e/o erythema.
Pathophysiology of ACE inhibitor-induced angioedema1
Angioedema is a vascular reaction associated with tissue (subcutaneous, submucosal) edema resulting from increased activity of vasoactive substances. The vasoactive substances in ACE inhibitor-induced angioedema are bradykinin and substance P. In the presence of ACE inhibition, these enzymes are inactivated through alternative pathways which, if disturbed, lead to angioedema.
Epidemiology of ACE inhibitor-induced angioedema
Angioedema occurs in 0.1-0.7% of patients taking ACE inhibitors, and 60% of cases occur within the first week of starting an ACE inhibitor (though it can occur as much as years later).2,3 ACE inhibitors are implicated as the cause of 20-40% of all ED visits for angioedema.4
Risk Factors2,5,6
- Female
- Age > 65yo
- African American
- Prior angioedema
- Smoking
- ACE inhibitor-associated cough
Clinical Features of ACE inhibitor-induced angioedema
Affected Sites:
- Mucous membranes of the head and neck
- Face
- Tongue
- Lips
- Pharynx
- Larynx
- GI tract
- Diffuse abdominal pain
- Nausea/vomiting/diarrhea
Signs/Symptoms at initial presentation:4
- SOB (89%)
- Lip swelling (70%)
- Tongue swelling (52%)
- Voice change/hoarseness (29%)
- Stridor (11%)
Key Clinical Features:
- Onset in minutes with resolution in 24-72 hours
- Absence of itching/urticaria7
Staging and Disposition:8
| Stage | Affected Site | Outpatient (%) | Floor (%) | ICU (%) | Intervention (%) |
|---|---|---|---|---|---|
| I | Face, lip | 48 | 52 | 0 | 0 |
| II | Soft palate | 60 | 40 | 0 | 0 |
| III | Tongue | 26 | 7 | 67 | 7 |
| IV | Larynx | 0 | 0 | 100 | 24 |
Management of ACE inhibitor-induced angioedema
- Proven benefit
- Airway management
- Withdrawal of ACE inhibitor
- Unclear benefit
- Epinephrine 0.3mg IM q15min
- Diphenhydramine 50mg IV
- Famotidine 20mg IV
- Solumedrol 125mg IV
- Future treatment options
- FFP: contains ACE9
- Icatibant: bradykinin B2 receptor antagonist10,11
References:
- Vleeming, W., van Amsterdam, J. G., Stricker, B. H. C., & de Wildt, D. J. (1998). ACE inhibitor-induced angioedema. Drug Safety, 18(3), 171–188. doi:10.2165/00002018-199818030-00003
- Grant, N. N., Deeb, Z. E., & Chia, S. H. (2007). Clinical experience with angiotensin-converting enzyme inhibitor-induced angioedema. Otolaryngology – head and neck surgery, 137(6), 931–935. doi:10.1016/j.otohns.2007.08.012
- Slater, E. E., Merrill, D. D., Guess, H. A., Roylance, P. J., Cooper, W. D., Inman, W. H., & Ewan, P. W. (1988). Clinical profile of angioedema associated with angiotensin converting-enzyme inhibition. JAMA : the journal of the American Medical Association, 260(7), 967–970.
- Banerji, A., Clark, S., Blanda, M., LoVecchio, F., Snyder, B., & Camargo, C. A. (2008). Multicenter study of patients with angiotensin-converting enzyme inhibitor-induced angioedema who present to the emergency department. Annals of allergy, asthma & immunology, 100(4), 327–332. doi:10.1016/S1081-1206(10)60594-7
- Gibbs, C. R., Lip, G. Y., & Beevers, D. G. (1999). Angioedema due to ACE inhibitors: increased risk in patients of African origin. British journal of clinical pharmacology, 48(6), 861–865.
- Morimoto, T., Gandhi, T. K., Fiskio, J. M., Seger, A. C., So, J. W., Cook, E. F., Fukui, T., et al. (2004). An evaluation of risk factors for adverse drug events associated with angiotensin-converting enzyme inhibitors. Journal of evaluation in clinical practice, 10(4), 499–509. doi:10.1111/j.1365-2753.2003.00484.x
- Kanani, A., Schellenberg, R., & Warrington, R. (2011). Urticaria and angioedema. Allergy, Asthma & Clinical Immunology, 7(Suppl 1), S9. doi:10.1186/1710-1492-7-S1-S9
- Ishoo, E., Shah, U. K., Grillone, G. A., Stram, J. R., & Fuleihan, N. S. (1999). Predicting airway risk in angioedema: staging system based on presentation. Otolaryngology – head and neck surgery, 121(3), 263–268.
- Hassen, G. W., Kalantari, H., Parraga, M., Chirurgi, R., Meletiche, C., Chan, C., Ciarlo, J., et al. (2013). Fresh frozen plasma for progressive and refractory angiotensin-converting enzyme inhibitor-induced angioedema. The Journal of emergency medicine, 44(4), 764–772. doi:10.1016/j.jemermed.2012.07.055
- Bas, M., Greve, J., Stelter, K., Bier, H., Stark, T., Hoffmann, T. K., & Kojda, G. (2010). Therapeutic Efficacy of Icatibant in Angioedema Induced by Angiotensin-Converting Enzyme Inhibitors: A Case Series. Annals of emergency medicine, 56(3), 278–282. doi:10.1016/j.annemergmed.2010.03.032
- MD, M. G., & MD, M. A. (2012). Icatibant: a novel approach to the treatment of angioedema related to the use of angiotensin-converting enzyme inhibitors. American Journal of Emergency Medicine, 30(8), 1664.e1–1664.e2. doi:10.1016/j.ajem.2011.09.014

