HPI:
HPI:
23M w/no known medical history presenting with abdominal “ball” x10d. Patient denies pain, and is tolerating regular diet w/o N/V. Reports lifting weights.
PMH/PSH/FHx/SHx:
None, non-contributory, no t/e/d.
Meds:
Acetaminophen, NKDA
PE:
- VS: T N/A HR 86 RR 18 BP 116/64 O2 N/A
- Gen: Well-appearing young male, no acute distress
- HEENT: PERRL, MMM no lesions
- CV: RRR, normal S1/S2, no murmurs
- Lungs: CTAB, no crackles/wheezes
- Abd: +BS, soft, NT/ND, 3cm bulge in right inguinal region with valsalva, above inguinal ligament, ~7cm lateral to symphysis, non-tender, reduces spontaneously after valsalva GU: uncircumcised penis, testes descended b/l, normal size, non-tender, no herniation through inguinal canal palpated with valsalva
- Ext: Warm, well-perfused, 2+ peripheral pulses
- Neuro: Alert and oriented, appropriate
Assessment/Plan:
23M ċ inguinal hernia, currently asymptomatic with no evidence of incarceration/strangulation. Recommend follow-up at city hospital for evaluation and possible surgical repair. Advised to refrain from strenuous activity, heavy lifting.
Physical Examination Techniques: 1
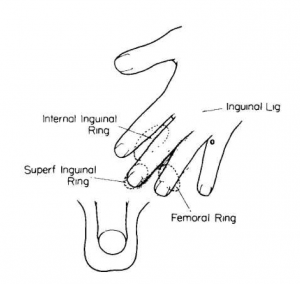
- Observation: Best performed with patient standing and physician seated on a stool facing the patient
- Palpation: place hand over patient’s groin (see figure), with two fingers each superior and inferior to the inguinal ligament. Have the patient cough and feel for a palpable bulge or impulse.
- GU: With a finger in the inguinal canal, bulges felt against the side of the examining finger are direct hernias, while those felt at the tip of the finger are indirect.
Types of Abdominal Wall Hernias: 2
| Name | Location | Etiology/Epidemiology |
| 1. Umbilical | Linea alba through weakened umbilical ring.Paraumbilical hernias through linea alba in the region of the umbilicus. | Congenital or acquired due to increased intra-abdominal pressure (obesity, pregnancy, ascites, PD) |
| 2. Epigastric | Linea alba between umbilicus and xiphoid process | Congenital weakness of linea alba (lack of decussating fibers) |
| 3. Spigelian | Semilunar line: along the lateral borders of rectus abdominus. Herniation typically occurs caudally (below arcuate line) due to absence of posterior rectus sheath. | |
| 4. Incisional | Site of prior incision | Poor fascial healing possibly due to: infection (increased risk in wound dehiscence), obesity, smoking, immunosuppression excess wound tension, CT disorders. |
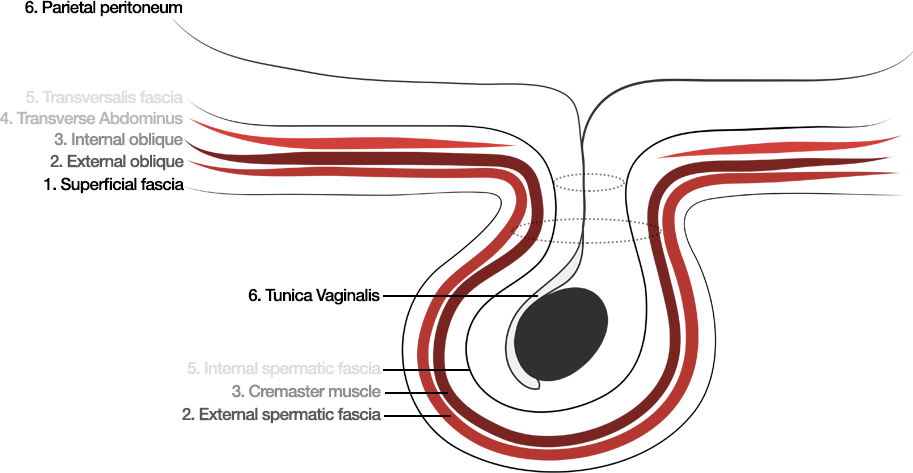
| 5. Inguinal | Indirect: internal (deep) inguinal ring, lateral to inferior epigastric vessels.Direct: external (superficial) inguinal ring, medial to inferior epigastric vessels. | Indirect > direct. |
| 6. Femoral | Inferior to the inguinal ligament, through empty space medial to femoral sheath. | F > M, increased likelihood of incarceration/strangulation (40%) |
| 7. Lumbar 3 | Arise in two anatomical triangles:Superior lumbar triangle – lateral border internal oblique, medial border erector spinae, superior border 12thrib.Inferior lumbar triangle – lateral border external oblique, medial border latissimus dorsi, inferior border iliac crest. (See figure) | Associated with surgery (incisional), typically urologic. |
| 8. Obturator | Protrusion of peritoneal sac through obturator foramen. | Rare, occur primarily in elderly women (high predisposition for incarceration). |
Locations of Abdominal Wall Hernias:
Layers of the Anterior Abdominal Wall:
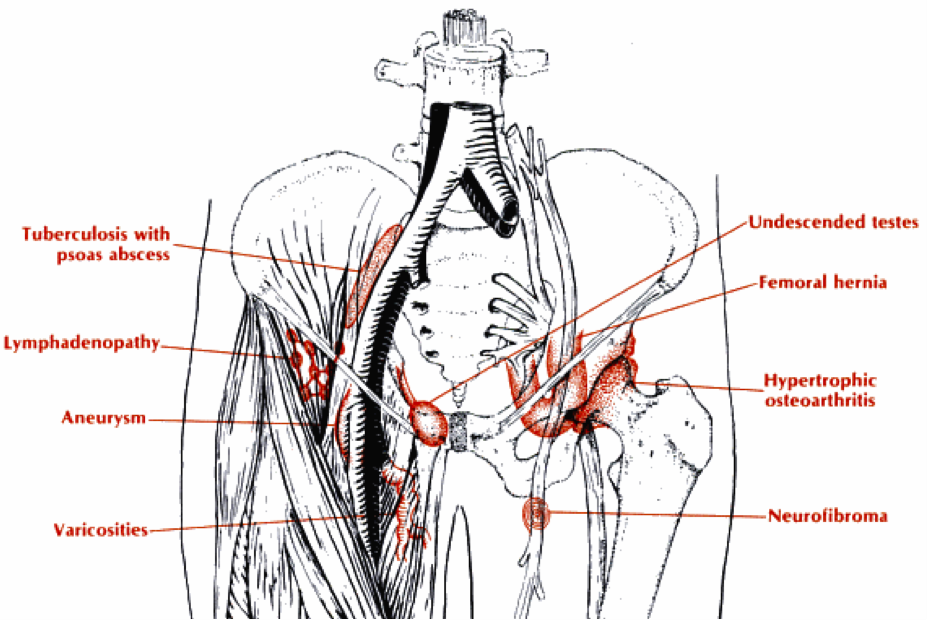
Differential diagnosis for groin masses: 4
| Category | Inguinal 5 | Scrotal 6 | Vulvar 7 | Perineal 8 |
| Vascular | Varicocele extension | Varicocele | Vulvar varicocity Hemangioma | |
| Infectious, Inflammatory | Lymphadenopathy Abscess Inflammatory joint process (hip, related bursae) Thrombophlebitis | Epididymitis Epididymo-orchitis | Condyloma Molluscum Bartholin’s cyst | |
| Neoplastic | Benign (lipoma) Lymph node metastatsis | Testicular malignancy | Malignant skin lesions | Soft-tissue malignancy Anal SCC Rectal GIST Metastasis (commonly anorectal, prostatic) |
| Congenital, Anatomic | Hernia Testis (undescended, retracted) | Epididymal cyst Spermatocele Hydrocele | Embryological remnants (mucocele) | |
| Traumatic | Hematoma Aneurysm (complication of catheterization) | Hematoma | Hematoma |
Locations of Groin Masses: 9
References:
- Amerson JR. Inguinal Canal and Hernia Examination. In: Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition. Boston: Butterworths; 1990. Chapter 96. Available from: http://www.ncbi.nlm.nih.gov/books/NBK423/
- Aguirre, D. A., Casola, G., & Sirlin, C. (2004). Abdominal Wall Hernias: MDCT Findings. American Journal of Roentgenology, 183(3), 681–690. doi:10.2214/ajr.183.3.1830681
- Guillem, P., Czarnecki, E., Duval, G., Bounoua, F., & Fontaine, C. (2002). Lumbar hernia: anatomical route assessed by computed tomography. Surgical and radiologic anatomy : SRA, 24(1), 53–56.
- Roberts, J. R., & Hedges, J. R. (2010). Clinical procedures in emergency medicine. (5th ed., Vol. section 7, p. Ch. 44). W B Saunders Co. Retrieved from http://www.mdconsult.com/books/page.do?eid=4-u1.0-B978-1-4160-3623-4.00044-4
- Shadbolt, C. L., Heinze, S. B., & Dietrich, R. B. (2001). Imaging of groin masses: inguinal anatomy and pathologic conditions revisited. Radiographics : a review publication of the Radiological Society of North America, Inc, 21 Spec No, S261–71.
- Eyre, RC. Evaluation of nonacute scrotal pathology in adult men. In: UpToDate, Rose, BD (Ed), UpToDate, Waltham, MA, 2013.
- Foster, D. C. (2002). Vulvar disease. Obstetrics and gynecology, 100(1), 145–163.
- Tappouni, R. F., Sarwani, N. I., Tice, J. G., & Chamarthi, S. (2011). Imaging of unusual perineal masses. American Journal of Roentgenology, 196(4), W412–20. doi:10.2214/AJR.10.4728
- Collins, R. (2008). Differential diagnosis in primary care. Philadelphia: Lippincott Williams & Wilkins.