Brief HPI:
A 28 year-old female with a history of IV drug use presents to the emergency department with back pain and fever. During evaluation for spinal epidural abscess, she develops vomiting and diarrhea. Examination reveals diaphoresis, mydriasis and hyperactive bowel sounds – she states that her last heroin use was 18-hours ago.
The patient was interested in guidance with cessation of opioid dependence and was evaluated by a recovery support specialist in the emergency department and provided with an appointment for outpatient follow-up. She was treated with buprenorphine-naloxone 8mg sublingual and her symptoms resolved. Her diagnostic evaluation was normal and she was discharged with a prescription for buprenorphine-naloxone 16mg daily until follow-up.
An Algorithm for the Management of Opioid Withdrawal1-4
Symptoms
- Dysphoria
- Rhinorrhea
- Myalgias, arthralgias
- Nausea, vomiting, diarrhea
- Abdominal cramps
Buprenorphine Considerations
Buprenorphine is a high-affinity, opioid partial agonist. The administration of buprenorphine may displace lower-affinity opioids.5 When used for the treatment of acute opioid withdrawal, special care must be taken to ensure that sufficient time has elapsed since last use (evidenced by the presence of moderate withdrawal symptoms) as the immediate displacement of existing opioids can precipitate severe withdrawal. In addition to provoking the maximum severity of the symptoms for which treatment was sought, this can generate mistrust in an otherwise effective medication and the healthcare system more broadly. The combination of buprenorphine with naloxone is intended to deter parenteral abuse – oral/sublingual naloxone is poorly bioavailable.
The initiation of medication-assisted treatment for opioid dependence from the emergency department should be dependent on the availability of outpatient follow-up and addiction treatment programs.6
Supportive Care4,6-7
| Symptom | Agent | Dose |
|---|---|---|
| Nausea, Vomiting | Promethazine | 25mg IM |
| Diarrhea | Loperamide | 4mg PO |
| Octreotide | 50mcg SQ | |
| Muscle cramps | Baclofen | 5mg PO |
| Anxiety, Dysphoria | Lorazepam | 1-2mg IV |
| Diazepam | 2-10mg PO, IM, IV | |
| Pain, Myalgia | Acetaminophen | 650mg – 1,000mg PO |
| Ibuprofen | 600mg PO |
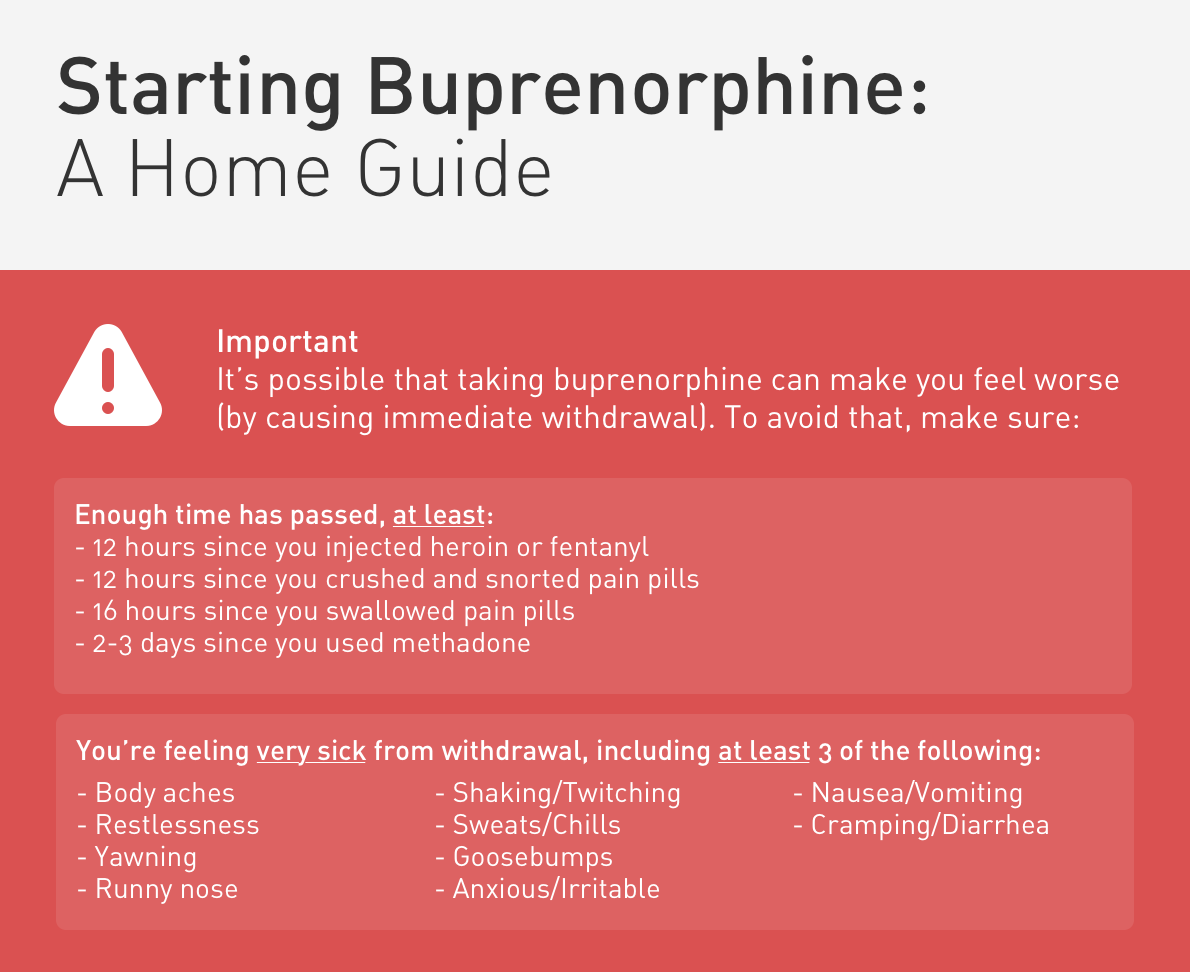
Unobserved Induction Guide8
The following guide is adapted from the Yale Department of Emergency Medicine ED-Initiated Buprenorphine Program and is available free for use.
References
- Strayer R, Hawk K, Hayes B, Herring A et al. Management of Opiate Misuse Disorder in the Emergency Department: A White Paper Prepared for the American Academy of Emergency Medicine. American Academy of Emergency Medicine.
- ED-Initiated Buprenorphine. Retrieved July 17, 2020, from https://medicine.yale.edu/edbup/Algorithm_338052_5_v2.pdf
- Su, M., Lopez, J., Crossa, A., Hoffman, R. (2018). Low dose intramuscular methadone for acute mild to moderate opioid withdrawal syndrome The American Journal of Emergency Medicine 36(11), 1951-1956. https://dx.doi.org/10.1016/j.ajem.2018.02.019
- Stolbach A, Hoffman R. Opioid withdrawal in the emergency setting. Post TW, ed. UpToDate. Waltham, MA: UpToDate Inc.
- Boas, R., Villiger, J. (1985). Clinical actions of fentanyl and buprenorphine. The significance of receptor binding. British journal of anaesthesia 57(2), 192-6. https://dx.doi.org/10.1093/bja/57.2.192
- D’Onofrio, G., Chawarski, M., O’Connor, P., Pantalon, M., Busch, S., Owens, P., Hawk, K., Bernstein, S., Fiellin, D. (2017). Emergency Department-Initiated Buprenorphine for Opioid Dependence with Continuation in Primary Care: Outcomes During and After Intervention Journal of General Internal Medicine 32(6), 660-666. https://dx.doi.org/10.1007/s11606-017-3993-2
- Gowing, L., Farrell, M., Ali, R., White, J. (2016). Alpha2‐adrenergic agonists for the management of opioid withdrawal Cochrane Database of Systematic Reviews https://dx.doi.org/10.1002/14651858.cd002024.pub5
- Home Initiated Buprenorphine. Retrieved July 17, 2020, from https://medicine.yale.edu/edbup/quickstart/Home_Buprenorphine_Initiation_338574_42801_v1.pdf
- Wesson DR, Ling W. The Clinical Opiate Withdrawal Scale (COWS). J Psychoactive Drugs. 2003;35(2):253-259. doi:10.1080/02791072.2003.10400007

