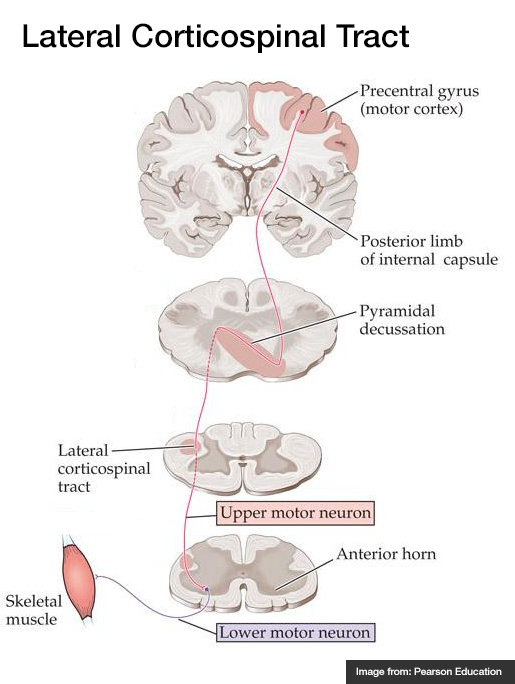
A systematic approach to motor weakness progresses along an anatomic tract from the cerebral cortex to individual sarcomeres. Impulses are generated in the primary motor cortex mapped to the homunculus, then aggregate as they descend through the internal capsule. Fibers decussate in the medulla and descend in the contralateral lateral corticospinal tract. These upper motor neurons (UMN) synapse with the lower motor neuron (LMN) in the anterior horn of the spinal cord. The lower motor neuron is bundled with neighboring fibers into a peripheral nerve and activates the target muscle fibers at the neuromuscular junction.
Algorithm for the Evaluation of Weakness

Upper Versus Lower Motor Neuron Findings
| Finding | Upper | Lower |
| Reflexes | | |
| Atrophy | | |
| Weakness | | |
| Fasciculation | | |
| Tone | | |
Summary
Recalling these findings can be simplified by understanding the underlying process. Denervation near the target muscle fibers (lower motor neuron disease) results in dampening of the efferent limb of spinal reflexes, resulting in hyporeflexia. The absence of nourishing stimulation leads to muscle atrophy and disorganized interpretation of proximal activity produces fasciculation.
Comparison Between Myopathy, Neuropathy and Neuromuscular Junction Processes
| Finding |
Myopathy |
Neuropathy |
Neuromuscular Junction |
| Example |
Polymyositis |
Guillain-Barre Syndrome |
Myasthenia Gravis |
| Distribution |
Proximal > Distal |
Distal > Proximal |
Diffuse, Bulbar |
| Reflexes |
|
|
Normal |
| Sensory |
|
|
|
| Fatigue |
|
|
|
| CK |
|
Normal |
Normal |
Motor Strength Grading
| Grade | Description |
| 5 | Normal |
| 4 | Reduced, moves against resistance |
| 3 | Moves against gravity |
| 2 | Moves only with elimination of gravity |
| 1 | Fasciculation only |
| 0 | None |
Reflex Grading
| Grade | Description |
| 4 | Increased amplitude, spread to adjacent, clonus |
| 3 | Increased |
| 2 | Normal |
| 1 | Decreased |
| 0 | None |
References
- Ganti L, Rastogi V. Acute Generalized Weakness. Emerg Med Clin North Am. 2016;34(4):795-809. doi:10.1016/j.emc.2016.06.006.
- Asimos AW. Weakness: A Systematic Approach To Acute, Non-traumatic, Neurologic And Neuromuscular Causes. Emergency Medicine Practice. 2002;4(12):1-28.
- Morchi R. Weakness. In: Rosen’s Emergency Medicine. Elsevier Inc.; 2014:2521.