HPI:
25M with a history of mild asthma transferred from an outside hospital after 10 days in the intensive care unit for continued management of ARDS.
The patient was well until one week prior to admission when he developed intermittent subjective fevers and general malaise associated with a non-productive cough and nausea/vomiting. He presented to the emergency department of an outside hospital with difficulty breathing and was noted to have respiratory distress and was subsequently admitted. Initial CT at the outside hospital revealed pneumomediastinum but no evidence of pulmonary embolism. Results from the outside hospital reveal a wide array of bacterial/fungal cultures and viral serologies including bronchoscopy but no obvious infectious source. The patient was treated with broad spectrum antibiotics for several days but his condition worsened requiring intubation, mechanical ventilation and transfer to the ICU. Further imaging was suggestive of ARDS, and the patient was transferred for additional management.
The patient was well until one week prior to admission when he reported development of malaise and fatigue. On the day of hospitalization, the patient presented to primary care doctor with complaint of cough and shortness of breath and was found to be in respiratory distress and was admitted. The patient received IV antibiotics (cefepime, vancomycin) and was intubated when respiratory distress worsened. Found to have evidence of ARDS on CXR.
PMH:
- Mild asthma, not requiring medication
- MRSA skin abscess
PSH:
- None
FH:
- Non-contributory.
SHx:
- Lives with family and works at a local supermarket. Rare alcohol use and no prior tobacco or drug use.
- No recent travel or sick contacts.
Meds:
- ciprofloxacin 400mg i.v. q12h
- linezolid 600mg i.v. q12h
- meropenem 1g i.v. q8h
- heparin 5000units s.q. q8h
- cisatracurium 1.48mcg/kg/min
- fentanyl 125mcg/hr
- midazolam 10mg/hr
- propofol 20mcg/kg/min
Allergies:
NKDA
Physical Exam:
| VS: | T | 97.8 | HR | 120 | RR | 35 | BP | 123/68 | O2 | 96% |
| Vent: | PRVC, VT 320, RR 35, PEEP 6, FiO2 95% | |||||||||
| Gen: | Young male, thin-appearing, intubated and sedated and not responding to verbal commands | |||||||||
| HEENT: | PERRL, unable to assess EOM, ET tube in place | |||||||||
| CV: | RRR, normal S1/S2, no murmurs | |||||||||
| Lungs: | Coarse breath sounds bilaterally | |||||||||
| Abd: | Normoactive bowel sounds, soft, non-distended, no hepatosplenomegaly | |||||||||
| Ext: | No clubbing, cyanosis, edema | |||||||||
| Neuro: | Unable to assess | |||||||||
Labs/Studies:
- CBC: 25.06/7.0/21.3/426
- BMP: 132/3.3/88/32/18/1.1/103
- ABG: 7.30/97/76/18
- Blood/sputum/urine cultures: Negative
- Aspergillus, crypto, cocci: Negative
- EBV, HIV, influenza, RSV: Negative
Imaging
CT Chest: Evidence of pneumomediastinum and pneumopericardium. Bilateral pulmonary infiltrates, but no pulmonary embolism.
Assessment/Plan:
25M with ARDS transferred from outside hospital for further management.
# ARDS: Severe (P/F ratio <100). Etiology unclear, thorough infectious workup without obvious source. Consider autoimmune or allergic cause.
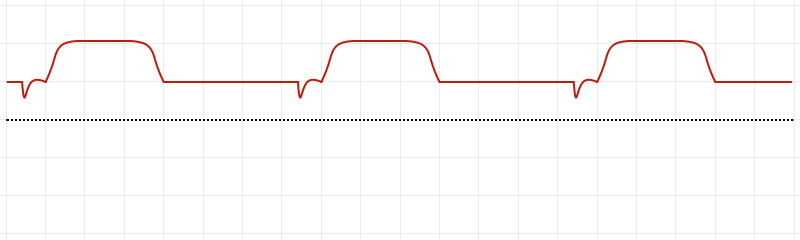
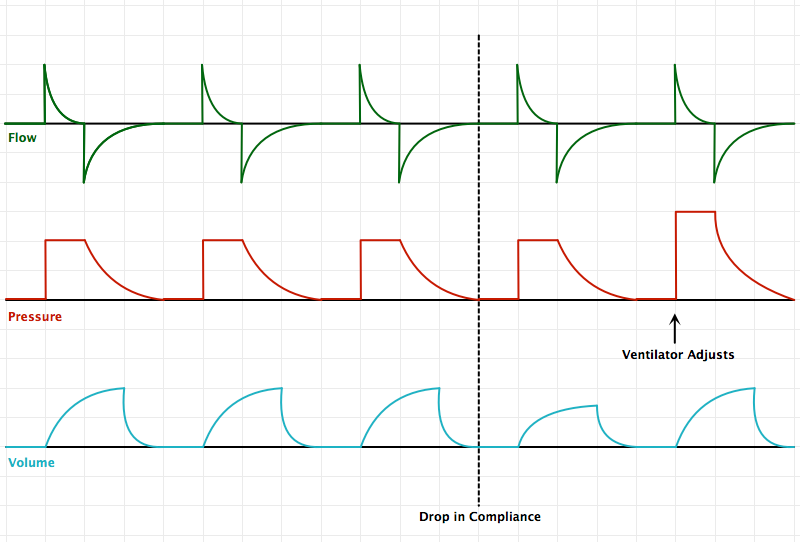
- Ventilator: PRVC lung-protective ventilation
- Consider NMB for dyssynchrony despite sedation
- Monitor strict I/O, maintain net negative fluid balance.
# Sepsis: Leukocytosis, tachycardia. Continue broad-spectrum antibiotics and monitor cultures.
# Acidosis: Largely respiratory, place dialysis catheter if acute need arises.
# Pneumomediastinum: Possible Boerhaave syndrome given reports of nausea/vomiting.
Pathophysiology of Acute Respiratory Distress Syndrome (ARDS):1
ARDS represents a stereotyped response to multiple insults. It is characterized by damaged capillary endothelium and alveolar epithelium resulting in increased permeability and the accumulation of fluid in the alveolar space. This causes diffuse alveolar damage and triggers the release of various cytokines (TNF, IL-1, IL-6) which recruit and activate neutrophils causing oxidative cell damage.
Definition of ARDS (Berlin):2,3
| Timing | Acute in onset (<1 week) |
| Chest imaging | Bilateral opacities |
| Origin of pulmonary edema | Not explained by heart failure or fluid overload (assessed with echocardiography) |
| Oxygenation (PaO2/FiO2) |
|
Causes of ARDS:2,4
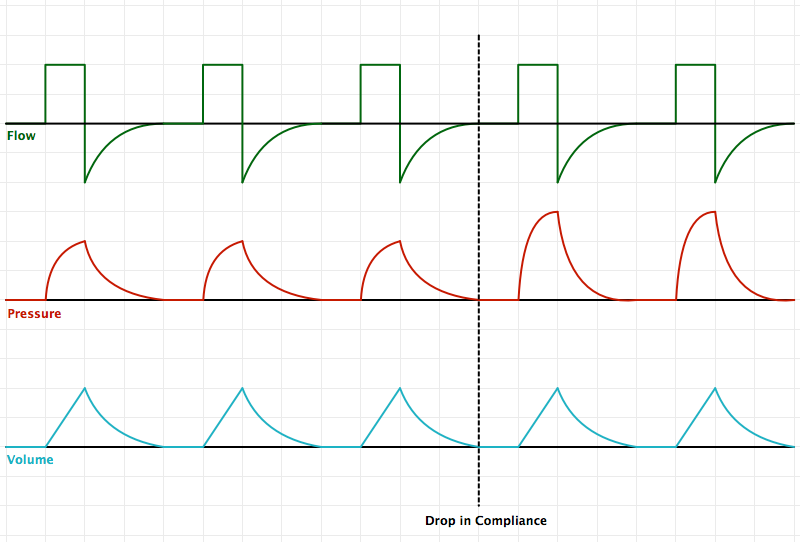
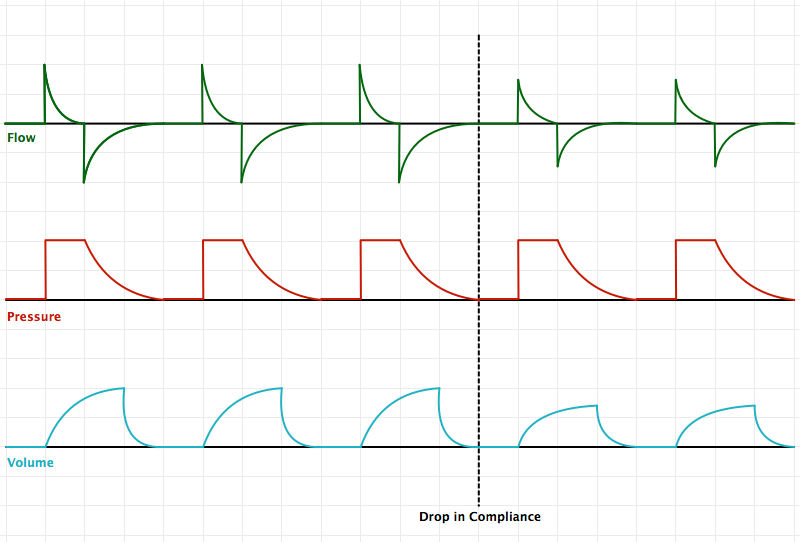
An Introduction to Mechanical Ventilation:5,6,7
This is a simplification of the general principles underlying the most common ventilator modes. For more detail, see the articles cited in the references.

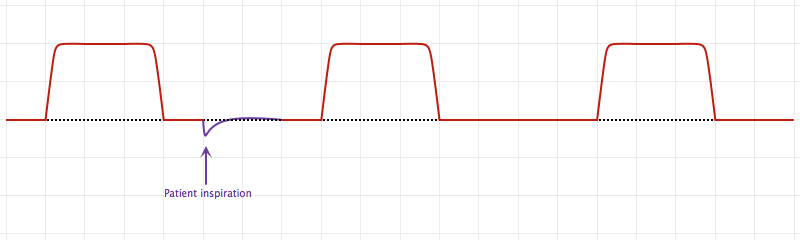
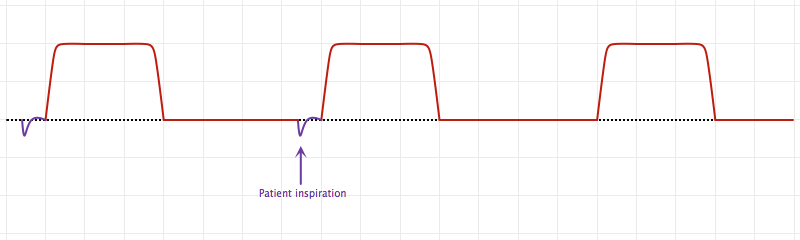
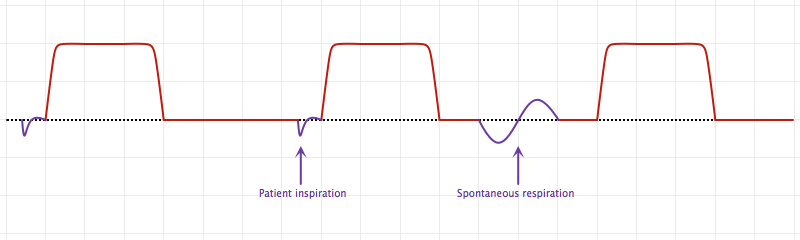
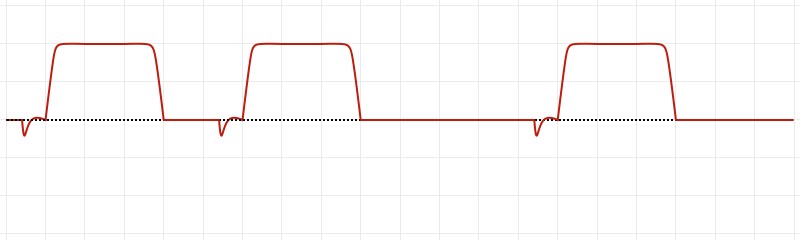
Breath Sequences:
Control Variables:
References:
- Pierrakos C, Karanikolas M, Scolletta S, Karamouzos V, Velissaris D. Acute respiratory distress syndrome: pathophysiology and therapeutic options. J Clin Med Res. 2012;4(1):7–16. doi:10.4021/jocmr761w.
- Fanelli V, Vlachou A, Ghannadian S, Simonetti U, Slutsky AS, Zhang H. Acute respiratory distress syndrome: new definition, current and future therapeutic options. J Thorac Dis. 2013;5(3):326–334. doi:10.3978/j.issn.2072-1439.2013.04.05.
- ARDS Definition Task Force, Ranieri VM, Rubenfeld GD, et al. Acute respiratory distress syndrome: the Berlin Definition. In: Vol 307. 2012:2526–2533. doi:10.1001/jama.2012.5669.
- Ware LB, Matthay MA. The acute respiratory distress syndrome. N. Engl. J. Med. 2000;342(18):1334–1349. doi:10.1056/NEJM200005043421806.
- Deng, J. (10/20/13). Principles of Mechanical Ventilation. Medical Intensive Care Unit Lecture. Los Angeles, CA.
- Singer BD, Corbridge TC. Basic invasive mechanical ventilation. South. Med. J. 2009;102(12):1238–1245. doi:10.1097/SMJ.0b013e3181bfac4f.
- Hamed HMF, Ibrahim HG, Khater YH, Aziz ES. Ventilation and ventilators in the ICU: What every intensivist must know. Current Anaesthesia & Critical Care. 2006;17(1-2):77–83. doi:10.1016/j.cacc.2006.07.008.