H&P
58 year-old female with no known past medical history, brought to emergency department by husband due to fatigue and weakness. The patient does not speak and cannot provide history. Her husband describes a progressive decline from normal baseline two weeks ago, noting lethargy/fatigue. Noted decreased speech and attention one week ago, and absent speech and requiring assistance with ambulation for the past two days. Thorough review of systems unremarkable excepting vomiting with decreased oral intake (tolerating fluids) and prior headache which resolved.
On examination, vital signs were normal, the patient was lying in bed and in no acute distress. The patient was non-verbal and did not follow commands (GCS E4-M5-V2). She was unable to comply with a thorough neurological examination, however pupils were equal and reactive, eyes tracked without nystagmus, no facial asymmetry noted, reflexes 1+ and symmetric in UE/LE, cannot participate in strength/sensory testing. Abdominal examination notable for infraumbilical and left-sided mass which elicits groans with palpation, though no rigidity or guarding. Mucous membranes moist, no skin tenting.
Labs
- CBC: 13.5 (97% neutrophils) , 12.9, 38.2, 240
- BMP: 107, 2.4, 70, 28, 9, 10, 0.44, 102
- Serum osmolarity: 224
- Urine osmolarity: 239
- UNa: 20
Imaging
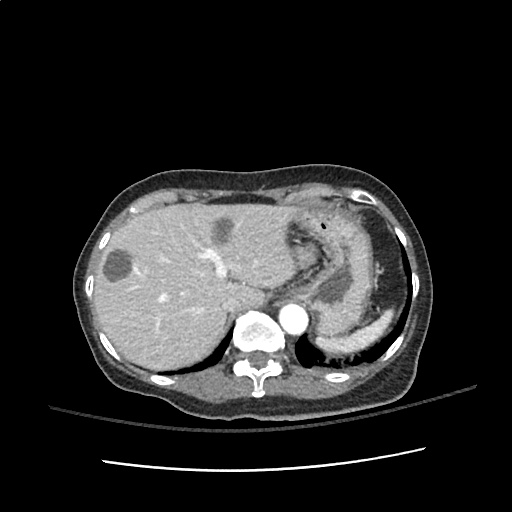
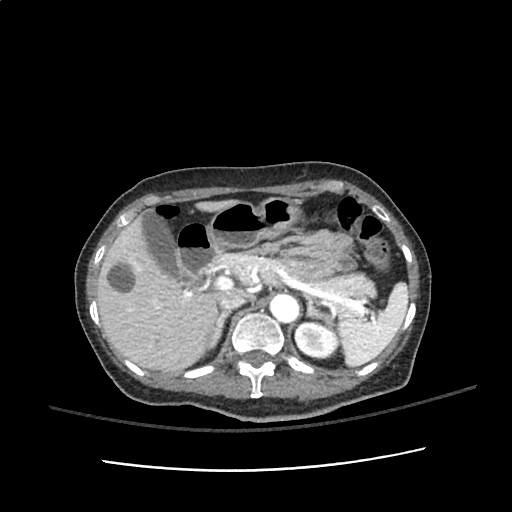
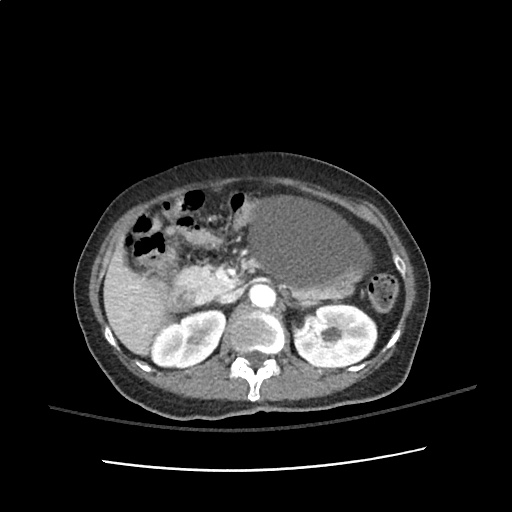
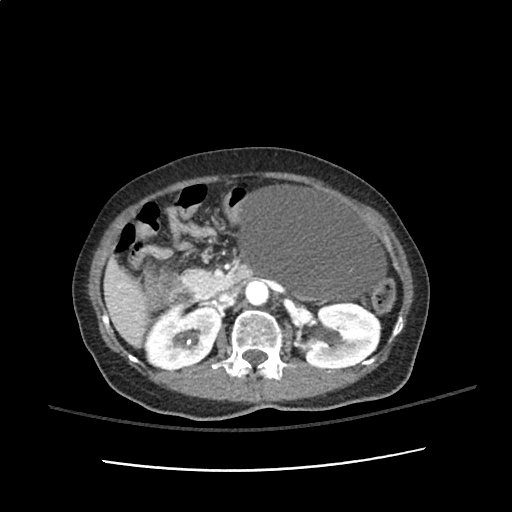
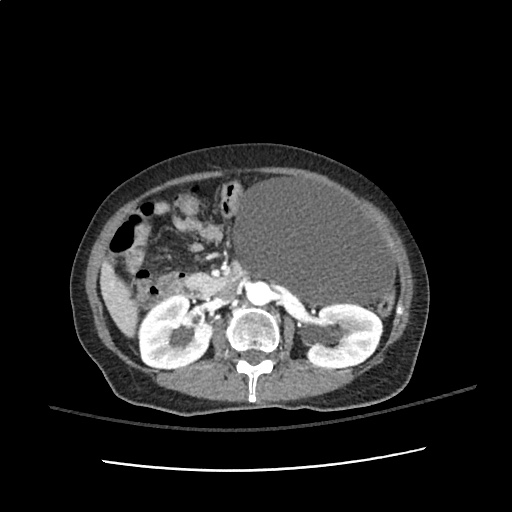
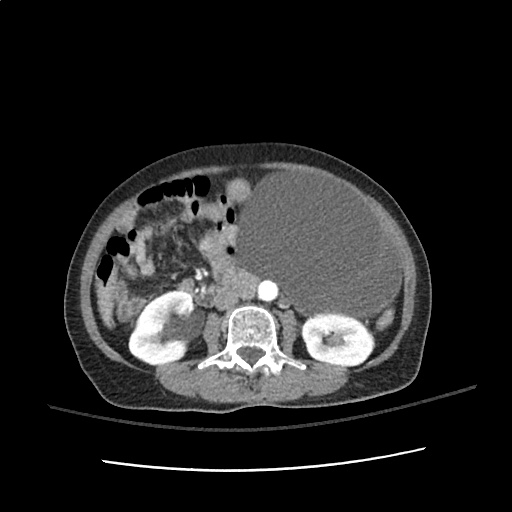
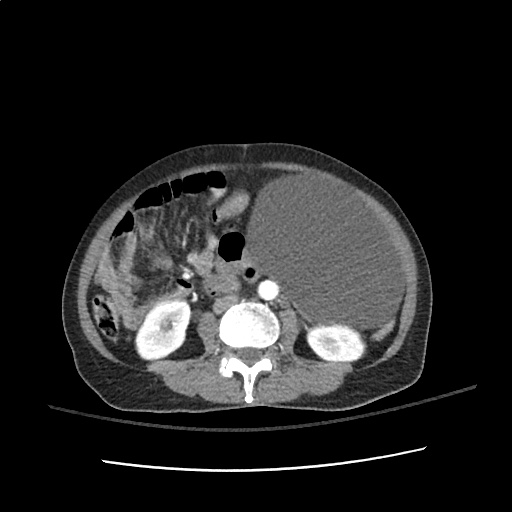
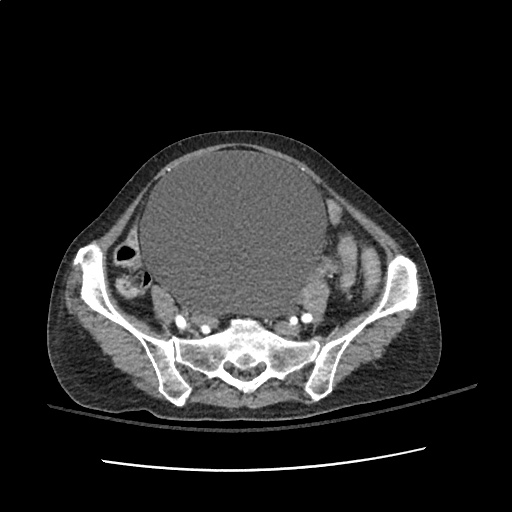
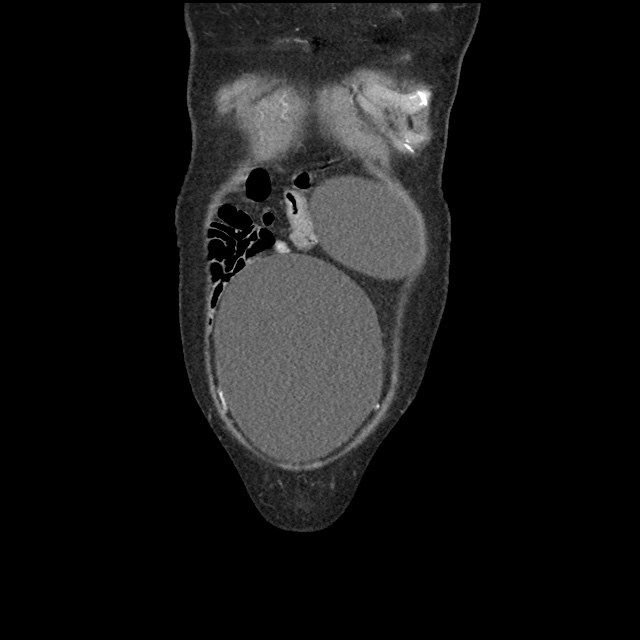
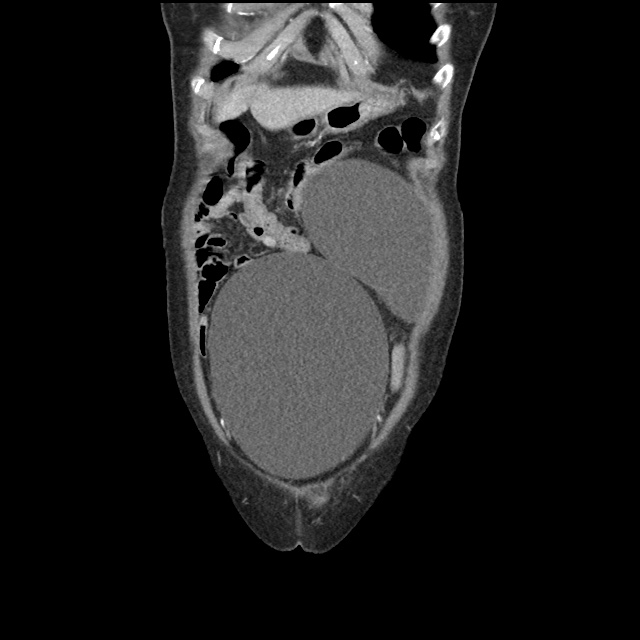
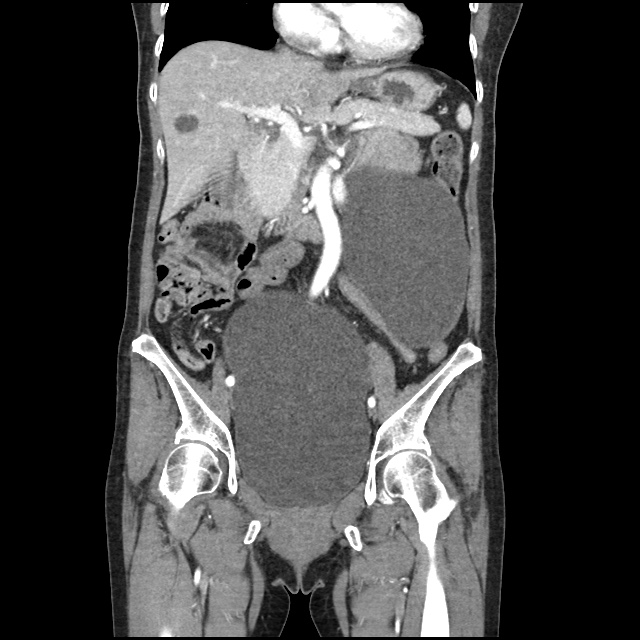
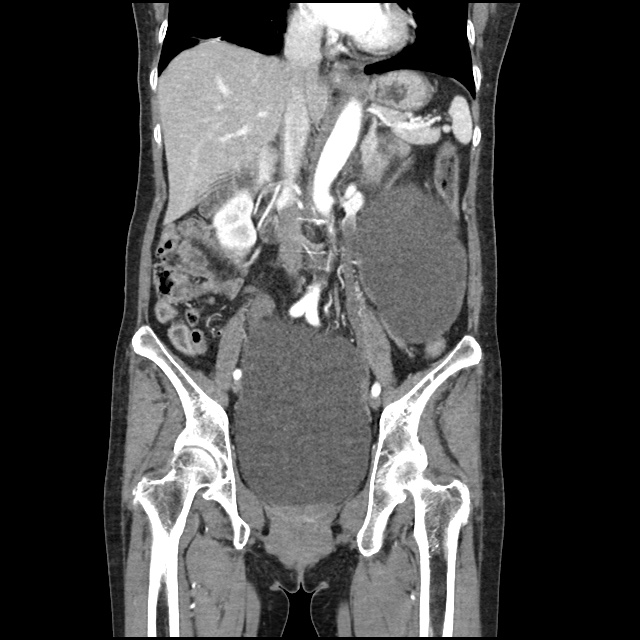
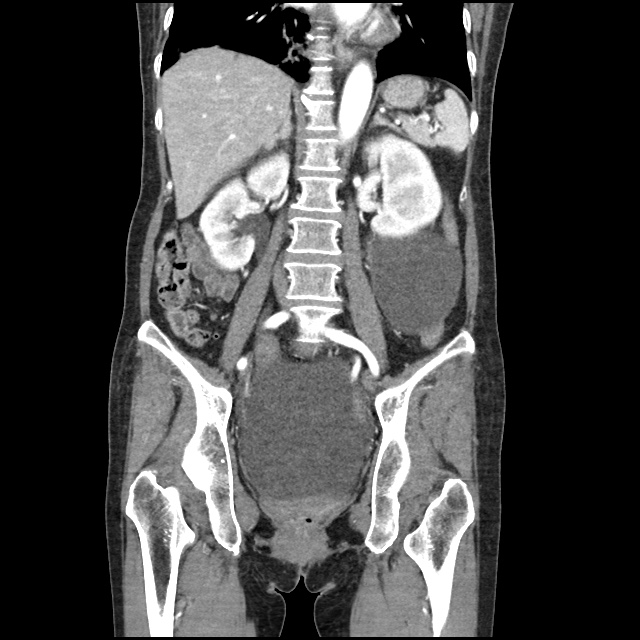
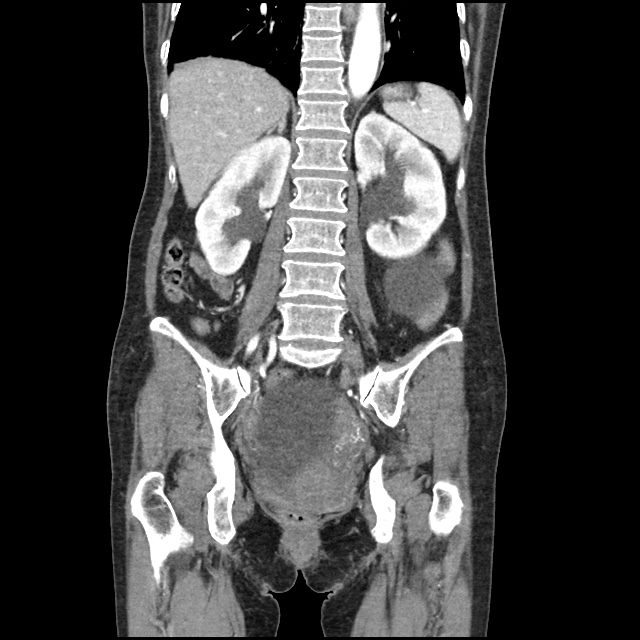
CT abdomen/pelvis with intravenous contrast
- Large, 15 cm cystic mass in the left abdomen, which likely arises from the mesentery. This mass is suspicious for neoplasm.
- Multiple low-density cystic lesions in the liver, which measure up to 4.5 cm in diameter and are concerning for metastatic disease. Alternatively, these may represent benign hepatic cysts which are unrelated to the mesenteric mass.
- Massively distended bladder, with moderate bilateral hydronephrosis and mild hydroureter.
Hospital Course
The patient was admitted to the medical intensive care unit. The following problem list details findings from the extensive inpatient evaluation.
#Altered Mental Status: The patient’s dramatically depressed level of consciousness improved gradually with correction of hyponatremia and the patient was alert, oriented and at baseline at the time of discharge. Evaluation included MRI brain which showed only chronic microvascular changes. A lumbar puncture was notable for isolated elevation of CSF protein. The patient was treated empirically for HSV encephalitis until CSF HSV PCR resulted negative. Neurology was consulted and identified increased CSF oligoclonal bands of unclear significance.
#Hyponatremia: Nephrology consulted, presumed SIADH based on urine studies (secondary to infection or malignancy). Corrected upon discharge.
#Pelvic Mass: Initially thought to arise from small bowel on CT abdomen/pelvis, after bladder decompression and transvaginal ultrasound, thought to arise from adnexa. Gynecology consulted, cyst characteristics (homogenous, fluid-filled) suggest benign process and tumor markers within normal limits. No acute intervention, drainage or biopsy warranted.
#Bladder distension: Unclear etiology, associated with mild/moderate hydronephrosis. Thought to be secondary to bladder outlet obstruction secondary to pelvic mass. Indwelling catheter placed, discontinued prior to discharge with successful spontaneous voiding trial and normal post-void residual.