HPI:
42 year-old male with no significant medical history presenting to ENT clinic after referral from PMD for perforated TM. The patient last had normal hearing approximately 1yr ago when he noted acute onset of right ear pain, discharge, hearing loss and ringing in the setting of fever and a productive cough. He does not recall an inciting event (trauma, swimming) to this initial episode, and had no previous history of ear infections. He saw his PMD several days later, was told he had a perforated ear drum and was treated with antibiotics.
Since then, the patient has not had any further ear pain or discharge but is left with persistent and constant hearing loss and ringing (high-pitched, non-pulsatile).
PMH:
None
PSH:
None
FH:
Non-contributory
SHx:
Worked in construction for 20yrs
Meds:
None
Allergies:
NKDA
Physical Exam:
| Gen: | Well-appearing, no acute distress |
| Head: | NC/AT |
| Eyes: | PERRL (4-2mm), disc margins sharp |
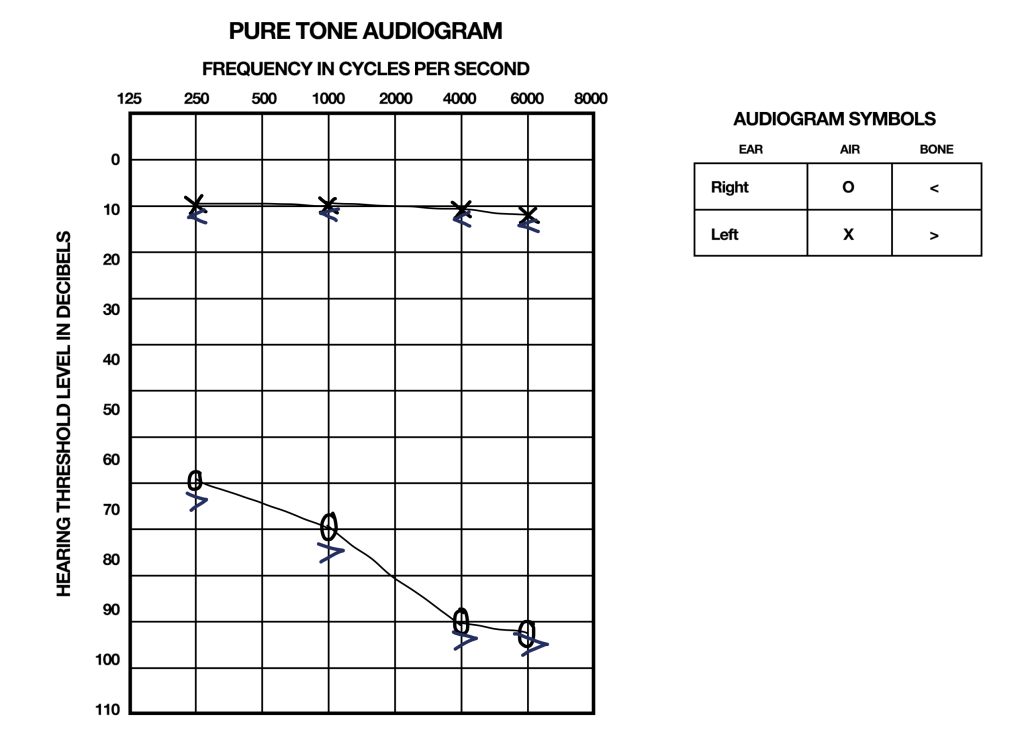
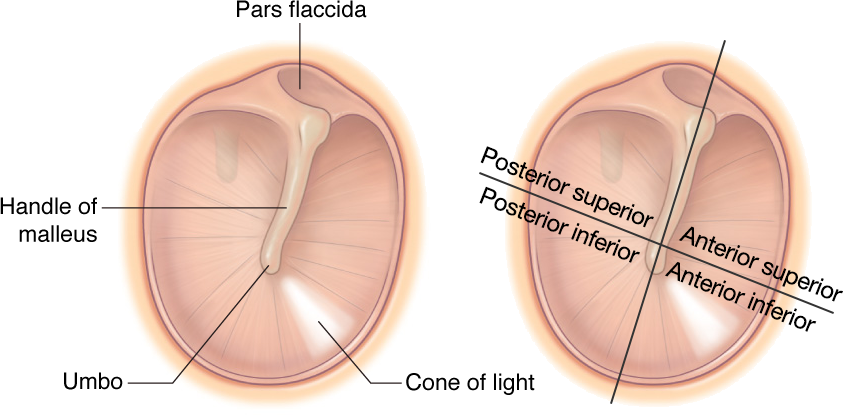
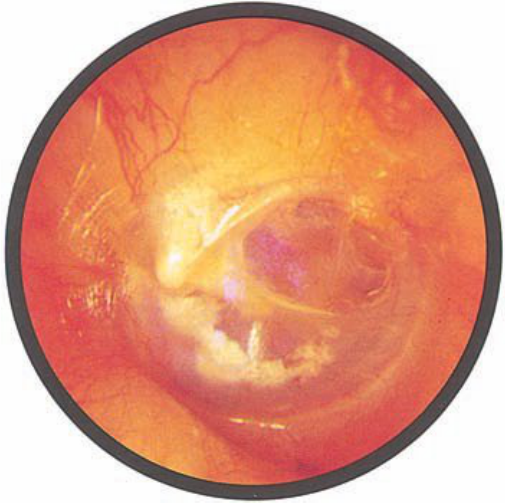
| Ears: | Weber lateralizes to left, AC > BC b/l AD: Decreased acuity to finger rub, EAC with some cerumen, cleared to reveal central perforation in posterior-superior quadrant of tympanic membrane. AS: EAC clear, TMI |
| Nose: | Nasal mucosa pink, septum midline |
| Mouth: | MMM, no lesions, good dentition, no pharyngeal erythema/exudates |
| Neck: | Trachea midline, supple, no cervical lymphadenopathy, no thyroid enlargement |
Studies
Assessment/Plan:
42M, no significant PMH, with perforated TM and audiogram showing mixed hearing deficit. The patient describes a history suggestive of acute otitis media complicated by TM perforation. Persistent perforation seen on examination today can result in the tinnitus and hearing loss the patient complains of. However the marked sensorineural component remains unexplained, particularly given the patient reported previously normal hearing. While there is some evidence that acute otitis media can lead to sensorineural hearing loss, it is typically only mild and only in high-frequency ranges.1,2 Plan for further evaluation with repeat audiogram and MRI IAC, RTC when studies completed.
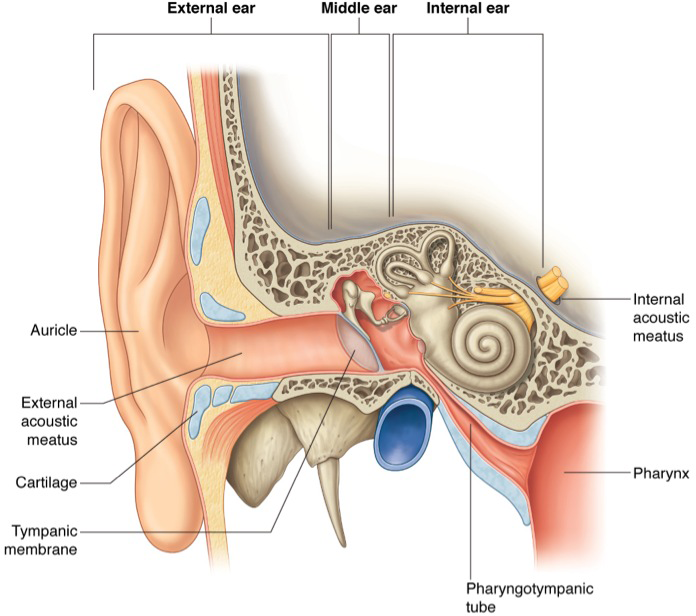
Examination of the Ear3
- External Auditory Canal: in acute otitis externa, the canal will be narrowed, swollen and erythematous
- Tympanic Membrane: use cone of light for orientation, identify malleus and move speculum to visualize all four quadrants
Differential Diagnosis of Hearing Loss4
Differential Diagnosis of Tinnitus5
References:
- Tarlow, M. (1998). Otitis media: pathogenesis and medical sequelae. Ear, nose, & throat journal, 77(6 Suppl), 3–6.
- Tsuprun, V., Cureoglu, S., Schachern, P. A., Ferrieri, P., Briles, D. E., Paparella, M. M., & Juhn, S. K. (2008). Role of pneumococcal proteins in sensorineural hearing loss due to otitis media. Otology & neurotology, 29(8), 1056–1060.
- Bickley, Lynn S., Peter G. Szilagyi, and Barbara Bates. Bates’ guide to physical examination and history taking. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins, 2009. Print.
- Isaacson, J. E., & Vora, N. M. (2003). Differential diagnosis and treatment of hearing loss. American family physician, 68(6), 1125–1132.
- Crummer, R. W., & Hassan, G. A. (2004). Diagnostic approach to tinnitus. American family physician, 69(1), 120–126.