CC:
Yellow eyes
HPI:
51yo AA male with hx DM, HTN, sarcoidosis presents with yellowing of eyes and full-body itching x3wks. This was associated with dark urine and loose, light-brown stools. He denies N/V, abdominal pain, PO intolerance, F/C, recent travel, weight loss. He states that this has not occurred in the past, and he does not have any prior history of post-prandial abdominal pain.
PMH:
|
PSH:
|
FH:
|
SHx:
|
Meds:
|
Allergies:
|
Physical Exam:
| VS: | T | 97.9 | HR | 102 | RR | 12 | BP | 128/68 | O2 | 99% RA |
| Gen: | WA, NAD | |||||||||
| HEENT: | Marked scleral icterus, PERRL, yellowing of posterior oropharynx and floor of mouth, MMM, no cervical lymphadenopathy | |||||||||
| CV: | RRR, S1/S2 normal, no murmurs | |||||||||
| Lungs: | CTAB with good air movement | |||||||||
| Abd: | Obese, +BS, soft, NT/ND, no rebound/guarding, no palpable organomegaly, negative Murphy | |||||||||
| GU: | No inguinal lymphadenopathy | |||||||||
| Ext: | Warm, well-perfused, no LE edema, peripheral pulses 2+ | |||||||||
| Skin: | No visible skin lesions | |||||||||
| Neuro: | AAOx3 | |||||||||
Labs:
- CBC: 16/12.4/35.1/281
- LFT: AST 281, ALT 302, AP 264, T.bili 22.1, D.bili 16.8
Studies:
- RUQ US: Biliary sludge, no stones, no GBW thickening, no pericholycystic fluid
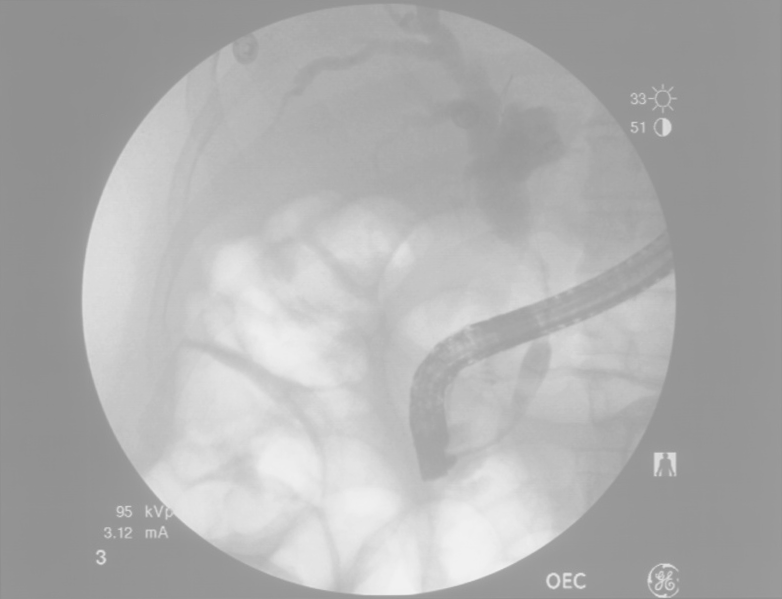
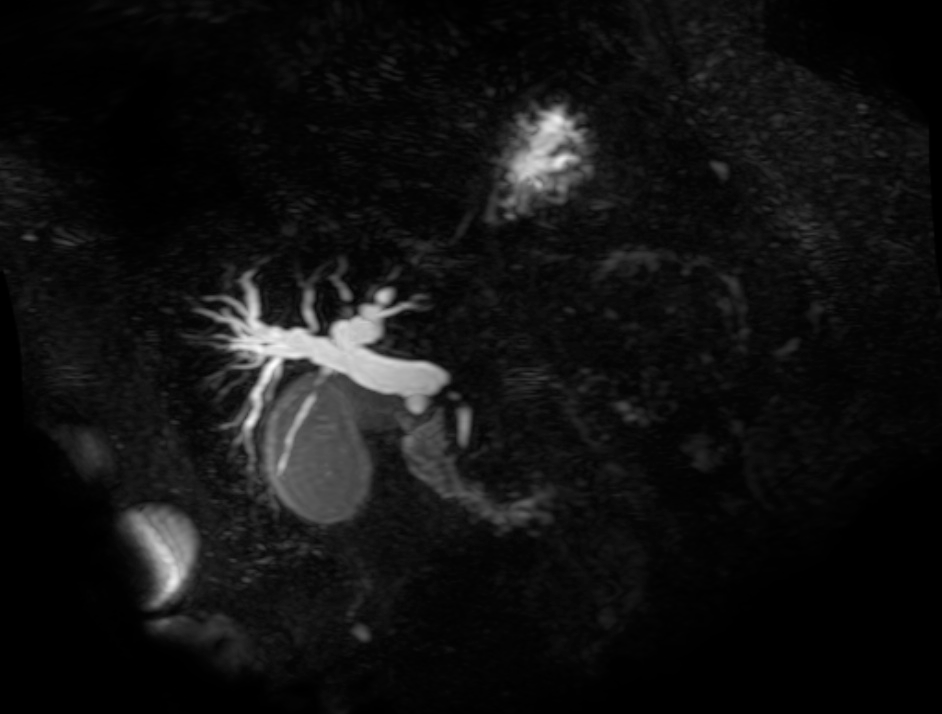
- ERCP: 3cm stricture of distal CBD, biopsies taken
Assessment/Plan:
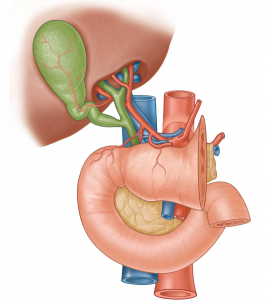
51AAM w/DM, HTN, sarcoidosis with 3wks painless jaundice. Obstructive pattern along with only modest elevation of liver enzymes suggests the obstruction is likely extrahepatic which was supported by ERCP finding of a distal CBD stricture. Patient has no history of prior instrumentation to cause iatrogenic stricture, and while sarcoidosis is associated with cholestatic complications (portal granulomas), pathology from biopsy showed papillary adenocarcinoma. The patient was scheduled for surgery with a plan for initial laparoscopic survey of the abdomen followed by Whipple if no evidence of widespread disease.
Imaging:
Differential Diagnosis of Hyperbilirubinemia: 1, 2
Evaluation of Hyperbilirubinemia: 3
References:
- Heathcote, E. J. (2007). Diagnosis and Management of Cholestatic Liver Disease. Clinical Gastroenterology and Hepatology, 5(7), 776–782. doi:10.1016/j.cgh.2007.05.008
- Hirschfield, G. M., Heathcote, E. J., & Gershwin, M. E. (2010). Pathogenesis of cholestatic liver disease and therapeutic approaches. Gastroenterology, 139(5), 1481–1496. doi:10.1053/j.gastro.2010.09.004
- McGill, J. M., & Kwiatkowski, A. P. (1998). Cholestatic liver diseases in adults. The American Journal of Gastroenterology, 93(5), 684–691. doi:10.1111/j.1572-0241.1998.206_a.x




Pingback: Differential Diagnosis of Biliary Duct Dilation
Pingback: Differential Diagnosis of Lactic Acidosis