Brief H&P:
A 50 year-old male with a history of colonic mucinous adenocarcinoma on chemotherapy presented with a chief complaint of “vomiting”. He was unwilling to provide further history, repeating that he had vomited blood prior to presentation. His initial vital signs were notable for tachycardia. Physical examination showed some dried vomitus, brown in color, at the nares and lips; left upper quadrant abdominal tenderness to palpation; and guaiac-positive stool. Point-of-care hemoglobin was 3g/dL below the most recent measure two months prior. As his evaluation progressed, he developed hypotension and was transfused two units of uncrossmatched blood with adequate blood pressure response – he was started empirically on broad-spectrum antibiotics for an intra-abdominal source. Notable laboratory findings included a normal hemoglobin/hematocrit, acute kidney injury, and elevated anion gap metabolic acidosis presumably attributable to serum lactate of 10.7mmol/L. Computed tomography of the abdomen and pelvis demonstrated pneumoperitoneum with complex ascites concerning for bowel perforation. The patient deteriorated, was intubated, started on vasopressors and admitted to the surgical intensive care unit. The initial operative report noted extensive adhesions and perforated small bowel with feculent peritonitis. He has since undergone multiple further abdominal surgeries and remains critically ill.
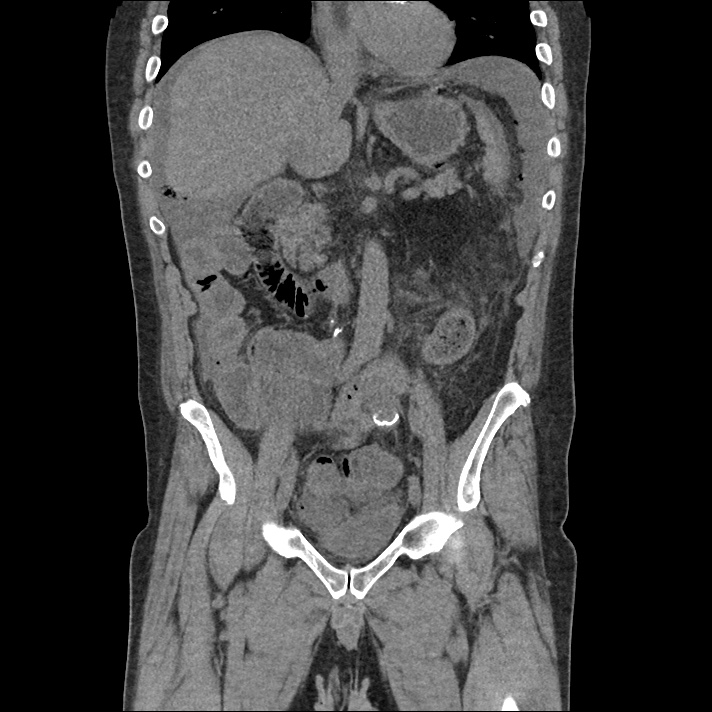
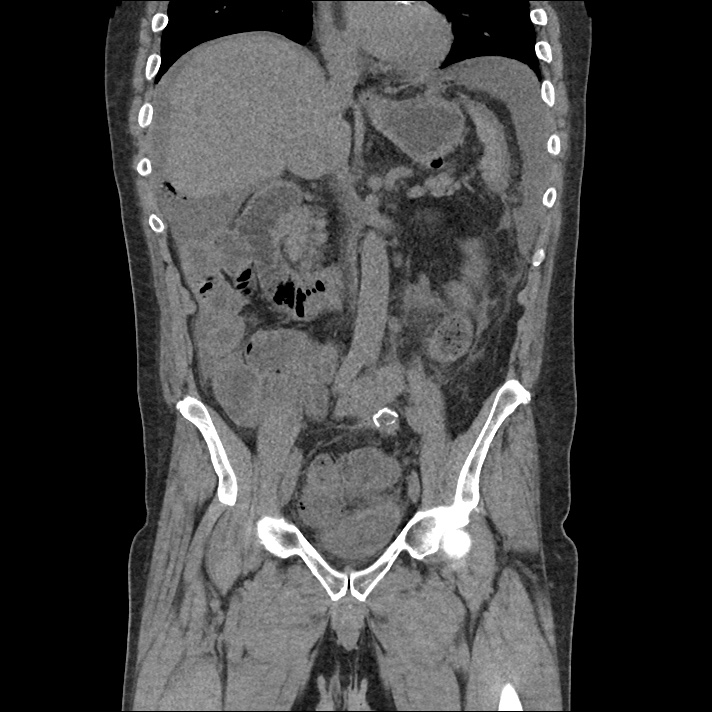
Imaging
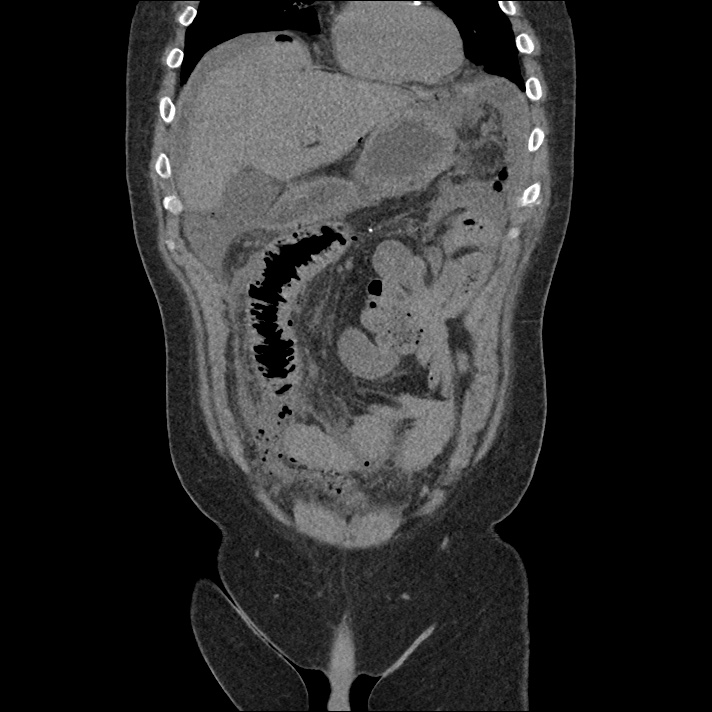
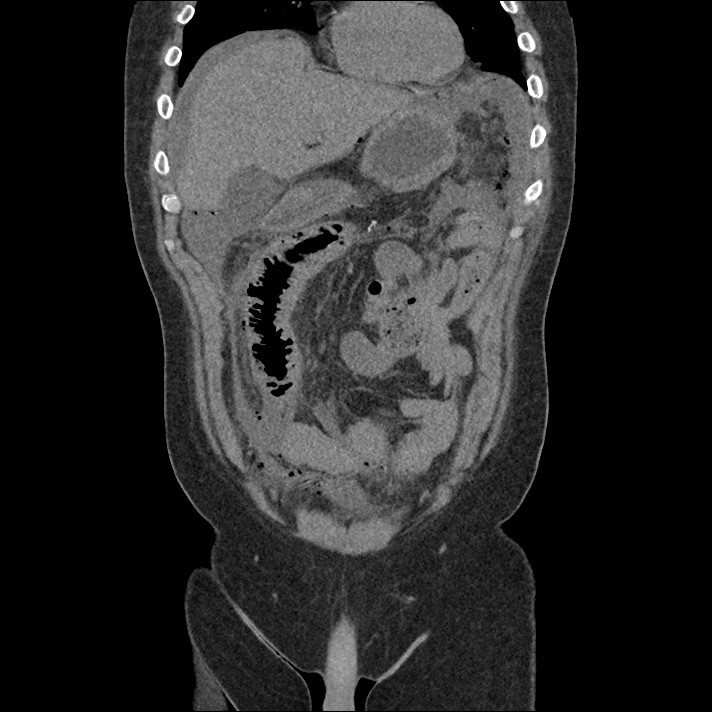
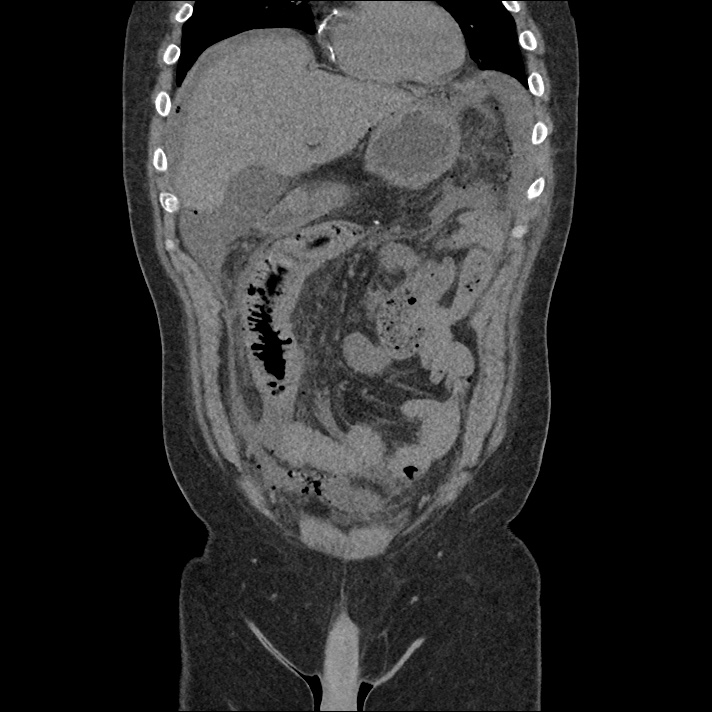
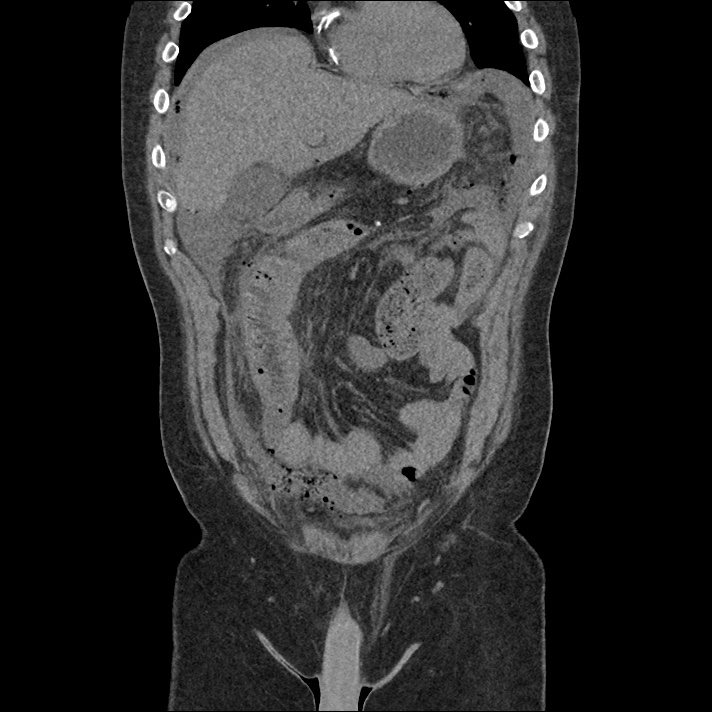
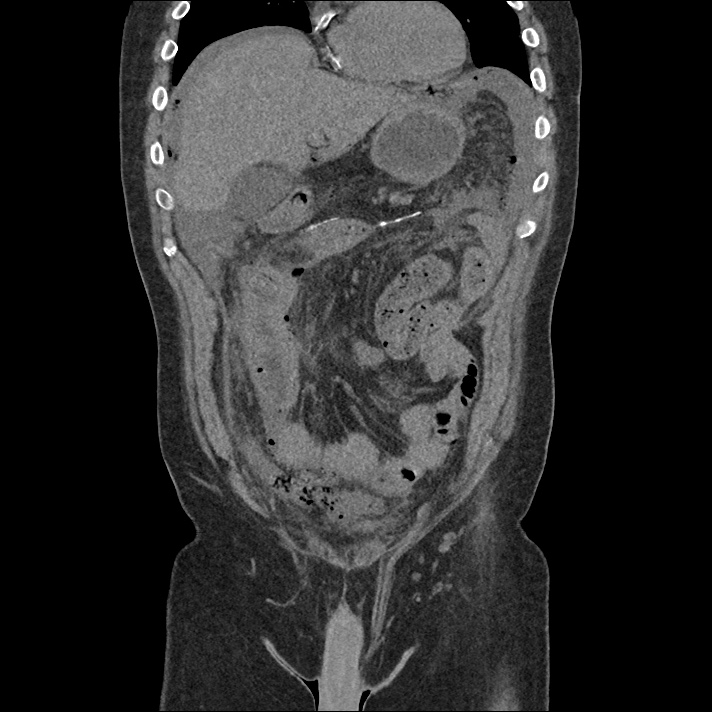
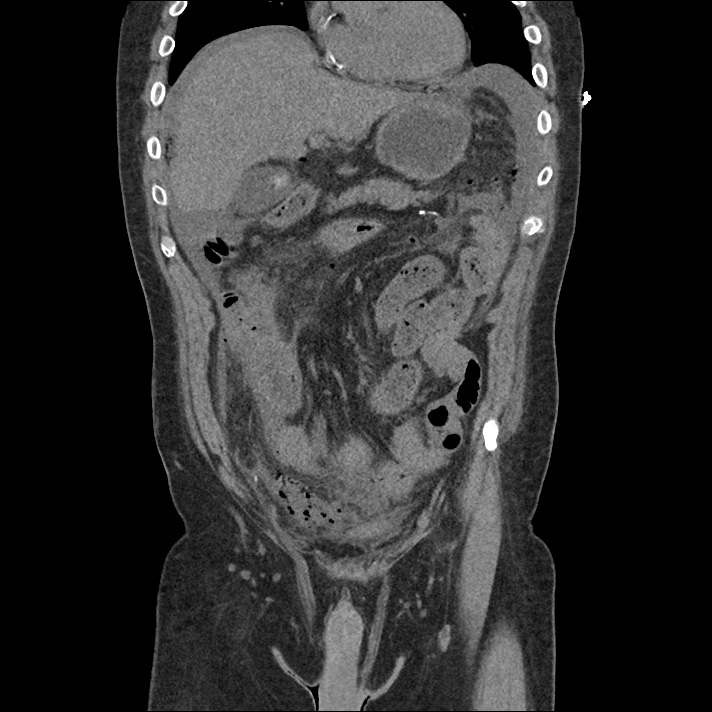
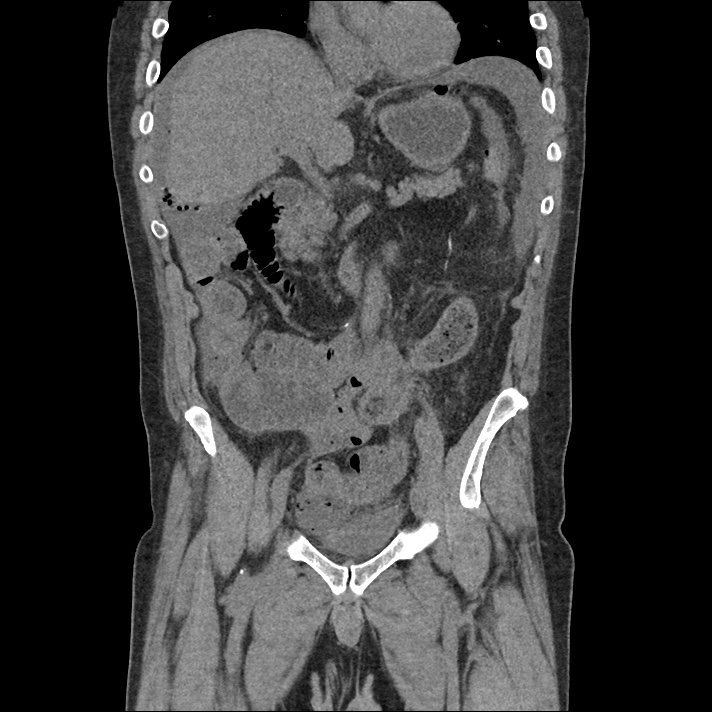
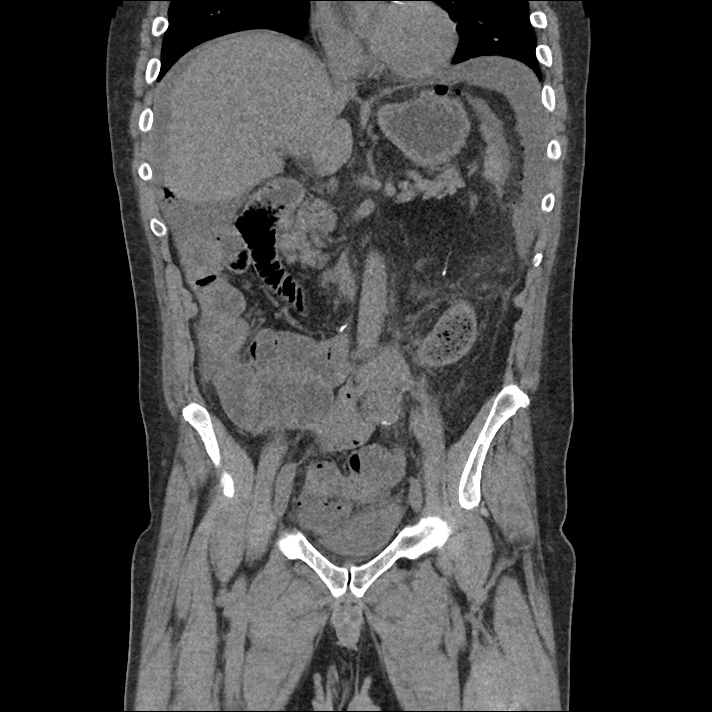
CT Abdomen/Pelvis
Free air is seen diffusely in the non-dependent portions of the abdomen: in the anterior abdomen and pelvis, inferior to the diaphragm, and in the perisplenic region. There is complex free fluid in the abdomen.
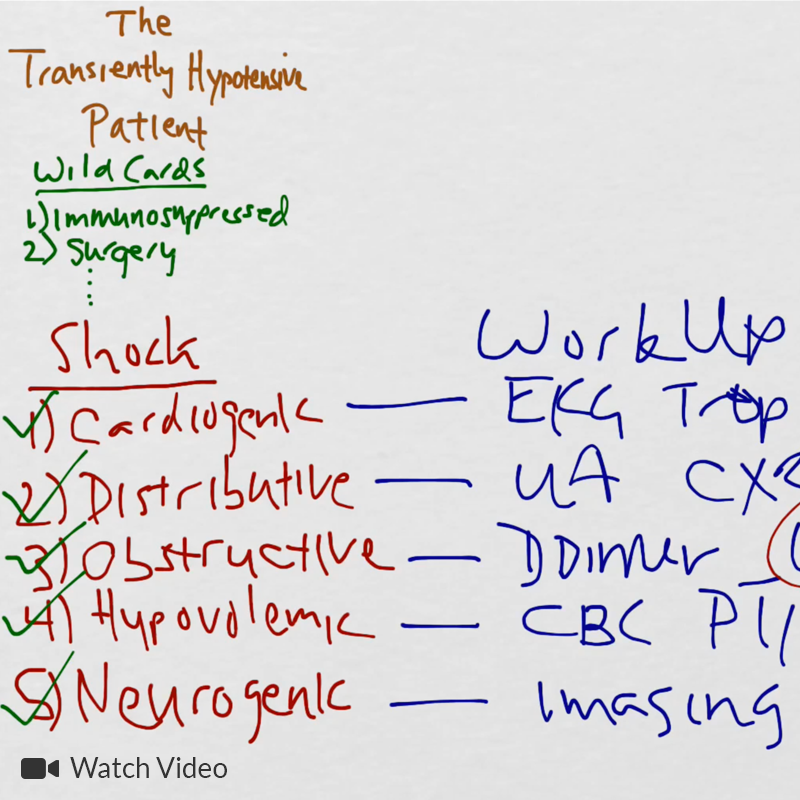
Algorithm for the Evaluation of Hypotension1
This process for the evaluation of hypotension in the emergency department was developed by Dr. Ravi Morchi. In the case above, a systematic approach to the evaluation of hypotension using ultrasonography and appropriately detailed physical examination may have expedited the patient’s care. The expertly-designed algorithm traverses the cardiovascular system, halting at evaluable checkpoints that may contribute to hypotension.
- The process begins with the cardiac conduction system to identify malignant dysrhythmias (bradycardia, or non-sinus tachycardia >170bpm), which, in unstable patients are managed with electricity.
- The next step assesses intravascular volume with physical examination or bedside ultrasonography of the inferior vena cava. Decreased right atrial pressure (whether due to hypovolemia, hemorrhage, or a distributive process) is evidenced by a small and collapsible IVC. If hemorrhage is suspected, further ultrasonography with FAST and evaluation of the abdominal aorta may identify intra- or retroperitoneal bleeding.
- If a normal or elevated right atrial pressure is identified, evaluate for dissociation between the RAP and left ventricular end-diastolic volume. This is typically caused by a pre- or intra-pulmonary obstructive process such as tension pneumothorax, cardiac tamponade, massive pulmonary embolism, pulmonary hypertension, or elevated intra-thoracic pressures secondary to air-trapping. Thoracic ultrasonography can identify pneumothorax, pericardial effusion, or signs of elevated right ventricular systolic pressures (RV:LV, septal flattening).
- Assuming adequate intra-vascular volume is arriving at the left ventricle, rapid echocardiography can be used to provide a gross estimate of cardiac contractility and point to a cardiogenic process. If there is no obvious pump failure, auscultation may reveal murmurs that would suggest systolic output is refluxing to lower-resistance routes (ex. mitral insufficiency, aortic insufficiency, or ventricular septal defect).
- Finally, if the heart rate is suitable, volume deficits are not grossly at fault, no obstructive process is suspected, and cardiac contractility is adequate and directed appropriately through the vascular tree, the cause may be distributive. Physical examination may reveal dilated capillary beds and low systemic vascular resistance.
Guided Lecture

Watch “The Transiently Hypotensive Patient: Who Cares?” from EM Ed. In this lecture Dr. Basrai reviews the diagnostic pathway for a patient who presents with transient hypotension.
References
- Morchi R. Diagnosis Deconstructed: Solving Hypotension in 30 Seconds. Emergency Medicine News. 2015.