HPI:
40 year-old male with a history of diabetes presents with right foot pain and swelling. His symptoms began 3 days ago with pain on the lateral surface of his right foot, described as aching, non-radiating and exacerbated with walking. Yesterday, he noted more prominent swelling and redness involving 4th and 5th toes. He denies trauma, fevers, and discharge.
PMH:
- Diabetes mellitus, diagnosed 8yrs ago
PSH:
- None
FH:
- Non-contributory
SHx:
- Lives with wife and 2 children and works an office job.
- Ten year history of tobacco use, quit 3 years ago.
- No EtOH or drug abuse.
Meds:
- Metformin 500mg p.o. b.i.d.
- Ibuprofen p.r.n. joint pain
Allergies:
NKDA
Physical Exam:
| VS: | T | 101.2 | HR | 88 | RR | 14 | BP | 147/71 | O2 | 100% RA |
| Gen: | Obese male, pleasant and in no acute distress, lying in bed with right foot raised. | |||||||||
| HEENT: | PERRL, EOMI, dry mucous membranes. | |||||||||
| CV: | RRR, normal S1/S2, no extra heart sounds, no murmurs. | |||||||||
| Lungs: | CTAB | |||||||||
| Abd: | +BS, non-tender. | |||||||||
| Ext: | Right lower extremity with 8x8cm area of erythema predominantly involving lateral aspect of foot, dorsum of foot and 3-5th digits. There is a shallow, 1x1cm ulcer on the plantar surface of foot near 5th MTP. Area is also notable for ecchymosis and palpable crepitus. There is minimal tenderness to palpation or with active/passive range of motion. | |||||||||
| Skin: | The remainder of the skin exam is unremarkable. | |||||||||
| Neuro: | AAOx3. | |||||||||
Labs/Studies:
- BMP: 134/4.3/104/26/18/1.4/206
- WBC: 27.3/13.1/40/189 (90% neutrophils)
- Lactate: 1.2
- CRP: [pending]
Imaging:
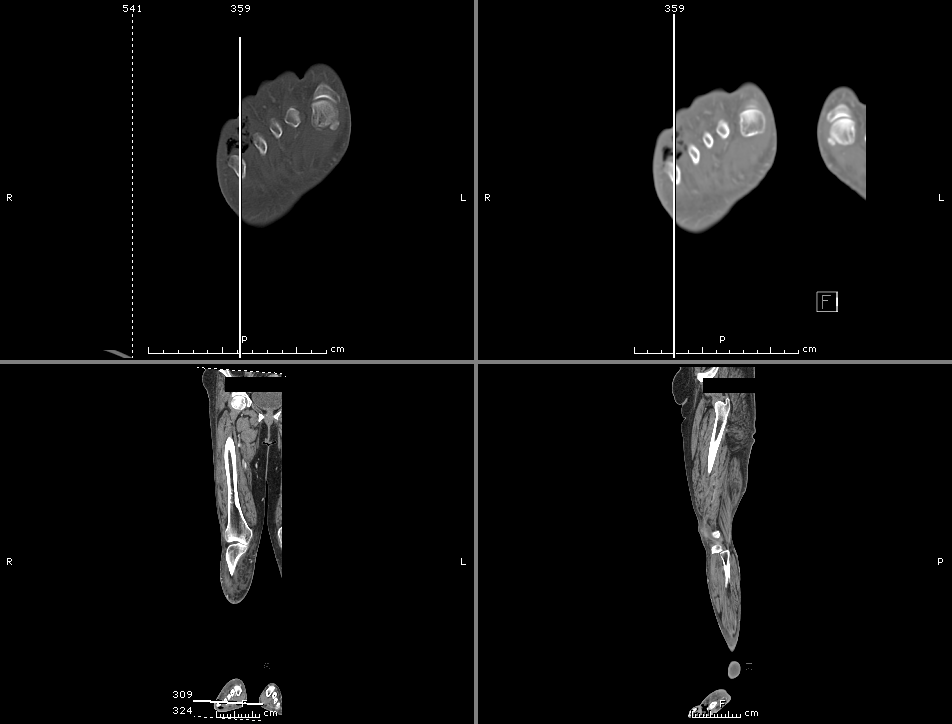
- Calf cellulitis and gas-producing cellulitis in the lateral foot and toes.
- Thigh and inguinal lymphadenopathy.
- Although gas is seen down to the level of the bone, no definite bony changes are identified to establish a diagnosis of osteomyelitis. Please note that MRI is more sensitive for detection of early osteomyelitis.
Assessment/Plan:
40M with DM and diabetic foot ulcer resulting in a necrotizing soft tissue infection as evidenced by gas on imaging. Recommended surgical debridement and started on broad-spectrum antibiotics including:
- vancomycin 1g i.v. q.12.h.
- cefepime 2g i.v. q.8.h.
- metronidazole 500mg i.v. q.8.h.
The patient underwent amputation of 3-5th digits with good surgical margins and was discharged on post-operative day three in good condition.
Skin and soft-tissue layers and their infections: 1
Necrotizing Soft-Tissue Infections (NSTI):2,3,4
Risk Factors
- IVDA
- Comorbid conditions
- DM
- Obesity
- Immunosuppression
Physical Exam
- Early (non-specific)
- Swelling
- Erythema
- Pain
- Late (non-sensitive)
- Tense edema outside affected skin perimeter
- Disproportionate pain
- Ecchymosis
- Bullae
- Crepitus
- Systemic signs (fever, tachycardia, hypotension)
Treatment
- Surgical debridement
- Antimicrobials
- Carbapenem, combination B-lactam B-lactamase
- Vancomycin, linezolid (MRSA coverage)
- Clindamycin (inhibit protein synthesis)
- Supportive therapy
LRINEC score 5
| Name | Value | Score |
|---|---|---|
| CRP | ≥150 | 4 |
| WBC | 15-25 >25 |
1 2 |
| Hb | 11-13.5 <11 |
1 2 |
| Na | <135 | 2 |
| Creatinine | >1.6 | 2 |
| Glucose | >180 | 1 |
<5 Low risk, 6-7 Intermediate risk, >8 High risk
References:
- Morchi, R. (2/18/14). Emergency Medicine Procedures Cadaver Lab. Clinical Clerkship at UCLA. Los Angeles, CA.
- Goldstein, E. J. C., Anaya, D. A., & Dellinger, E. P. (2007). Necrotizing Soft-Tissue Infection: Diagnosis and Management. Clinical infectious diseases, 44(5), 705–710. doi:10.1086/511638
- Headley, A. J. (2003). Necrotizing soft tissue infections: a primary care review. American family physician, 68(2), 323–328.
- McHenry, C. R., Piotrowski, J. J., Petrinic, D., & Malangoni, M. A. (1995). Determinants of mortality for necrotizing soft-tissue infections. Annals of surgery, 221(5), 558–63.
- Wong, C.-H., Khin, L.-W., Heng, K.-S., Tan, K.-C., & Low, C.-O. (2004). The LRINEC (Laboratory Risk Indicator for Necrotizing Fasciitis) score: A tool for distinguishing necrotizing fasciitis from other soft tissue infections. Critical Care Medicine, 32(7), 1535–1541. doi:10.1097/01.CCM.0000129486.35458.7D

