Case 1
64M with a history of HFrEF (LVEF 20-25%), CAD, AICD (unknown indication), COPD, CKD III presenting with gradual onset shortness of breath, progressive bilateral lower extremity edema.
Examination consistent with severe acute decompensated heart failure presumed secondary to left ventricular dysfunction.
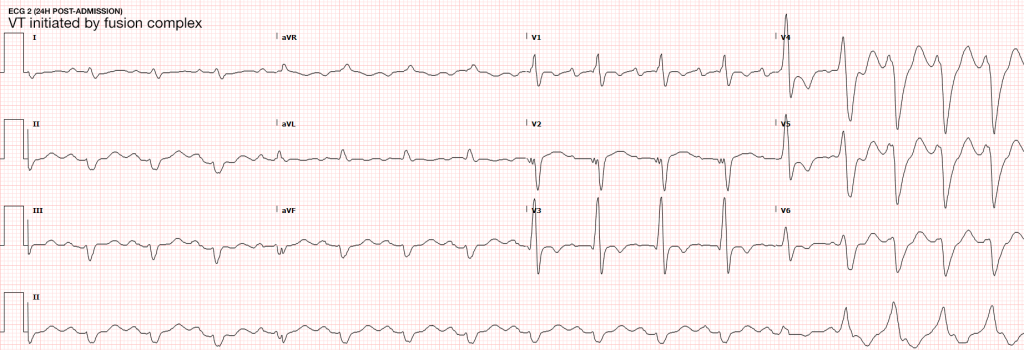
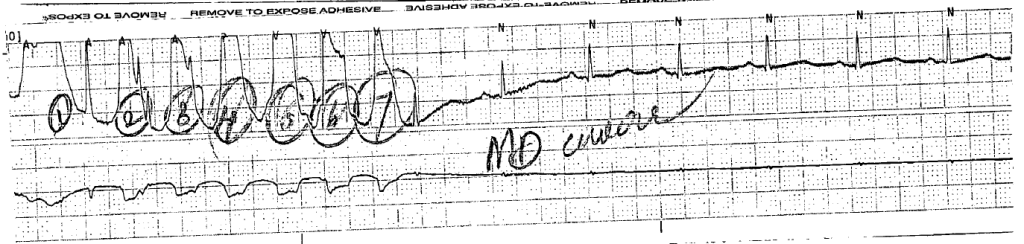
Telemetry monitoring with multiple episodes of nonsustained ventricular tachycardia.
In the ED, the patient developed worsening respiratory failure despite initiation of therapy, requiring endotracheal intubation. Continuous cardiac monitoring revealed persistent salvos of NSVT, progressing to slow ventricular tachycardia without device intervention.
Device interrogation revealed multiple events, 3 shocks, several ATP’s over the recorded period.
Evaluation and Management:
- NSVT with known (severe) ischemic heart disease
- For repetitive monomorphic ventricular tachycardia: amiodarone, beta-blockade (if tolerated), procainamide (IIA, C)1
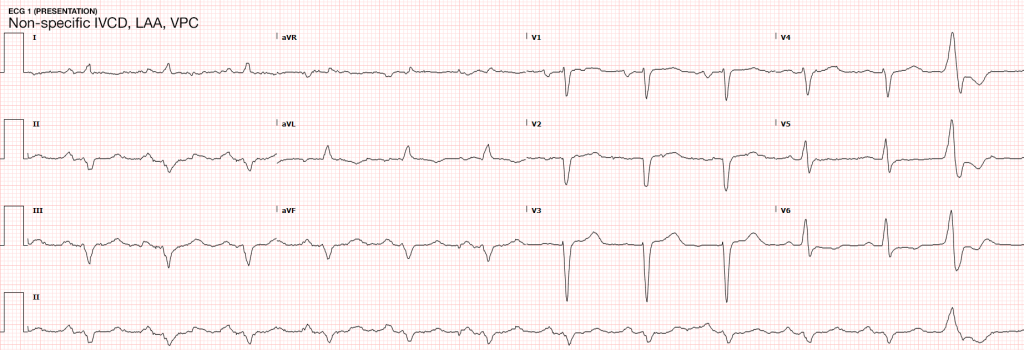
ECG’s
Case 2
31F with autoimmune polyglandular syndrome (adrenal, thyroid and endocrine pancreatic insufficiency), presenting with fever and cough.
Evaluation consistent with sepsis presumed secondary to pulmonary source.
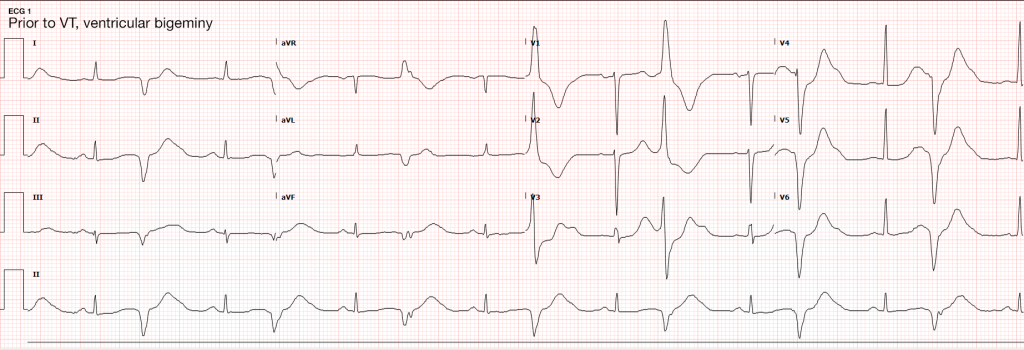
Telemetry monitoring initially with ventricular bigeminy, then nonsustained ventricular tachycardia.
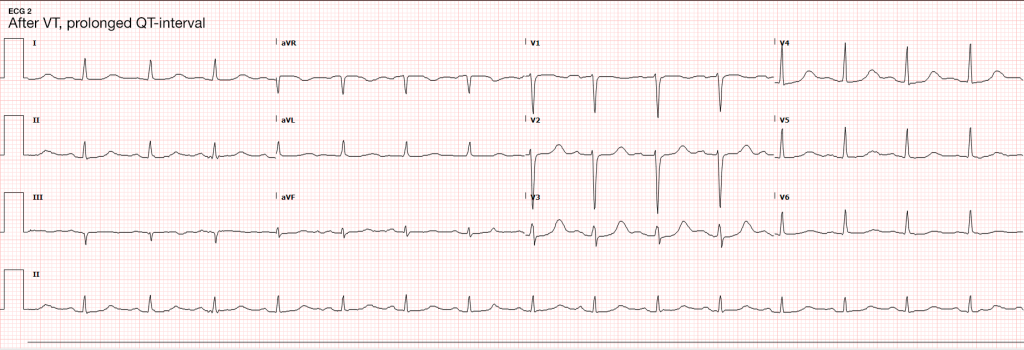
In the ED, the patient developed pulseless ventricular tachycardia – apparently polymorphic. Chest compressions and epinephrine produced return of spontaneous circulation with recovery to baseline neurologic function.
ECG revealed prolonged QTc and chemistry panel notable for critical hypokalemia/hypomagnesemia.
Evaluation and Management:
- NSVT progressing to VT
- Initially attributed to electrolyte disturbances. However, serial ECG’s continued to show prolonged QTc (possibly acquired, home medications included metoclopramide and erythromycin). Early echocardiography demonstrated global hypokinesis with EF 30-35% attributed to severe sepsis and recurrent defibrillation. Cardiac CT after resolution of acute illness showed persistently depressed ejection fraction without coronary atherosclerosis. The presence of NICM associated with malignant dysrhythmias warranted ICD placement.
- Cardioversion for hemodynamic compromise (I, B), B-blockade (I, B), amiodarone if no LQTS (I, C), urgent angiography if ischemia not excluded (I, C)1
- Correction of electrolyte abnormalities (specifically hypokalemia) may decrease progression to VF.2
ECG’s
Definition3,4
- > 3-5 consecutive beats originating below the AV node
- Rate > 100bpm
- Duration <30s
Epidemiology3,5
- Occurs in 0-4% of ambulatory patients
- Increased frequency in males and with increasing age
In some patients, NSVT is associated with an increased risk of sustained tachyarrhythmias and sudden cardiac death. In others it is of little prognostic significance.6,7,8
Evaluation
- In all patients:
- History: including arrhythmogenic medications/substances, pertinent family history
- Physical examination
- ECG/CXR
- TTE
- In selected patients:
- Exercise testing
- Advanced imaging (CT/C-MR)
- Electrophysiologic studies
- Genetic testing
NSVT in the absence of structural heart disease
NSVT in Idiopathic Ventricular Tachycardia
- Ventricular outflow arrhythmias:
- RVOT: 70-80%, LBBB pattern
- LVOT: 20-30%, RBBB pattern
- Mechanism:
- Adrenergically mediated
- Occur during exercise, resolve as heart-rate increases, recur during recovery
- Management:
- Exclude arrhythmogenic right ventricular cardiomyopathy (imaging, myocardial biopsy)
- If symptomatic, beta-blockade, ± IC anti-arrhythmic, CCB (verapamil) for ILVT
- Prognosis:
- Good, rare tachycardia-induced cardiomyopathy, rare SCD
NSVT in Polymorphic Ventricular Tachycardia
- Mechanism
- LQTS (acquired or inherited)
- Familial catecholaminergic polymorphic VT
- Management
- Symptomatic (ex. syncope, cardiac arrest): ICD
- Asymptomatic QTc > 550ms: consider ICD
- Prognosis
- Increased risk SCD
Arrhythmogenic Right Ventricular Cardiomyopathy
- Mechanism
- Fibrosis, fibro-fatty replacement of myocardium in RVIT/RVOT/RV apex
- May occur with only subtle structural abnormalities of the right ventricle
- LBBB morphology
- Management
- Anti-arrhythmics of limited utility
- Catheter ablation, ICD backup
- Prognosis
- Increased risk SCD
NSVT with apparent structural heart disease1
Hypertension and LVH
- Mechanism
- Stretch-induced abnormal automaticity
- Fibrotic tissue
- Presence of NSVT correlates with degree of hypertrophy and subendocardial fibrosis
- Management
- Evaluation for ischemic heart disease
- Aggressive medical management of hypertension (including beta-blockade)
- Prognosis
- Unclear
Valvular Disease
- Mechanism
- High incidence in AS, severe MR (25%)
- Mechanical stress from dysfunctional valvular apparatus
- Management
- Beta-blockade if symptomatic
- Prognosis
- No evidence that NSVT is an independent predictor of SCD.
Ischemic Heart Disease9-14
- Mechanism
- Monomorphic VT associated with re-entry at the borders of ventricular scars
- Ischemia induces polymorphic NSVT/VF
- Management
- Revascularization, beta-blockade, statin, ACE/ARB
- MADIT I, MUSTT: ICD for ICM LVEF <40%, NSVT, EPS inducible VT
- MADIT II, SCD-HeFT: ICD for moderate-to-severe LV dysfunction irrespective of NSVT or EPS findings
- Prognosis
- NSTEMI with NSVT >48h after admission 2x risk SCD (MERLIN-TIMI 36)
- STEMI with NSVT common, not as predictive of ACM or SCD as LVEF (CARISMA)
- NSVT <24h after admission for NSTEMI/STEMI not of prognostic significance.
Hypertrophic Cardiomyopathy
- Mechanism
- Genetic myocardial disease
- Myocyte disarray, fibrosis, ischemia result in arrhythmogenic substrate
- Management
- Restriction of physical activity
- ICD (NSVT, LV thickness, FH SCD, syncope, abnormal BP response to exercise)
- Beta-blockade, anti-arrhythmic for symptoms
- Prognosis
- Increased risk SCD (1% annual)
Other Conditions
- Non-ischemic dilated cardiomyopathy
- Giant-cell myocarditis
- Repaired TOF
- Amyloidosis
- Sarcoidosis
- Chagas cardiomyopathy
Algorithm for the Evaluation of NSVT1
References
- Zipes DP, Camm AJ, Borggrefe M, et al. ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death–executive summary: A report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Develop Guidelines for Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death) Developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Eur Heart J. 2006;27(17):2099–2140. doi:10.1093/eurheartj/ehl199.
- Higham PD, Adams PC, Murray A, Campbell RW. Plasma potassium, serum magnesium and ventricular fibrillation: a prospective study. Q J Med. 1993;86(9):609–617.
- Katritsis DG, Zareba W, Camm AJ. Nonsustained ventricular tachycardia. J Am Coll Cardiol. 2012;60(20):1993–2004. doi:10.1016/j.jacc.2011.12.063.
- Katritsis DG, Camm AJ. Nonsustained ventricular tachycardia: where do we stand? Eur Heart J. 2004;25(13):1093–1099. doi:10.1016/j.ehj.2004.03.022.
- Wellens HJ. Electrophysiology: Ventricular tachycardia: diagnosis of broad QRS complex tachycardia. Heart. 2001;86(5):579–585.
- Buxton AE, Lee KL, Fisher JD, Josephson ME, Prystowsky EN, Hafley G. A randomized study of the prevention of sudden death in patients with coronary artery disease. Multicenter Unsustained Tachycardia Trial Investigators. N Engl J Med. 1999;341(25):1882–1890. doi:10.1056/NEJM199912163412503.
- Jouven X, Zureik M, Desnos M, Courbon D, Ducimetière P. Long-term outcome in asymptomatic men with exercise-induced premature ventricular depolarizations. N Engl J Med. 2000;343(12):826–833. doi:10.1056/NEJM200009213431201.
- Udall JA, Ellestad MH. Predictive implications of ventricular premature contractions associated with treadmill stress testing. Circulation. 1977;56(6):985–989.
- Preliminary report: effect of encainide and flecainide on mortality in a randomized trial of arrhythmia suppression after myocardial infarction. The Cardiac Arrhythmia Suppression Trial (CAST) Investigators. N Engl J Med. 1989;321(6):406–412. doi:10.1056/NEJM198908103210629.
- Goldstein S. Propranolol therapy in patients with acute myocardial infarction: the Beta-Blocker Heart Attack Trial. Circulation. 1983;67(6 Pt 2):I53–7.
- Moss AJ. MADIT-I and MADIT-II. J Cardiovasc Electrophysiol. 2003;14(9 Suppl):S96–8.
- Moss AJ, Hall WJ, Cannom DS, et al. Improved survival with an implanted defibrillator in patients with coronary disease at high risk for ventricular arrhythmia. Multicenter Automatic Defibrillator Implantation Trial Investigators. N Engl J Med. 1996;335(26):1933–1940. doi:10.1056/NEJM199612263352601.
- Buxton AE, Lee KL, Fisher JD, Josephson ME, Prystowsky EN, Hafley G. A randomized study of the prevention of sudden death in patients with coronary artery disease. Multicenter Unsustained Tachycardia Trial Investigators. N Engl J Med. 1999;341(25):1882–1890. doi:10.1056/NEJM199912163412503.
- Bardy GH, Lee KL, Mark DB, et al. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med. 2005;352(3):225–237. doi:10.1056/NEJMoa043399.
- WikEM: Nonsustained Ventricular Tachycardia