HPI
30 year-old female with a history of autoimmune polyglandular syndrome (adrenal, thyroid and endocrine pancreatic insufficiency), polysubstance use, brought to the emergency department by ambulance with reported chief complaint of fever. On presentation, the patient reported fever for one day, associated with cough. She was lethargic and confused, answering yes/no questions but unable to provide detailed history. She states that she has been taking her home medications as prescribed, which include hydrocortisone, fludrocortisone, synthroid and insulin. No collateral information was immediately available.
Additional history was obtained from chart review upon discharge. The patient was hospitalized two weeks prior with pneumonia and discharged after two days. For 2-3 days prior to presentation, she reported the following symptoms to family members: nausea/vomiting, cough, decreased oral intake, fevers, and palpitations – she did not take her home medications during this time.
Physical Exam
| VS: | T | 38.6 | HR | 112 | RR | 18 | BP | 149/82 | O2 | 90% RA |
| Gen: | Alert, fatigued, slow responses. | |||||||||
| HEENT: | No meningeal irritation, dry mucous membranes. | |||||||||
| Pulmonary: | Tachypnea, inspiratory wheezing and faint crackles at left and right inferior lung fields, appreciated anteriorly as well. | |||||||||
| Neuro: | Alert, oriented to self, situation, not month/year. PERRL, EOMI, facial muscles symmetric, tongue protrudes midline without fasciculation. Peripheral sensation grossly intact to light touch and moves all extremities on command. | |||||||||
Labs
- VBG: alkalemia, primary respiratory
- CBC: no leukocytosis, normal differential, normocytic anemia
- BMP: 131, 2.5 , 94, 28, 11, 1.6, 115
- Mg: 1.3
- Lactate: 1.0
- TSH: 17 , T4: 1.03
- Troponin: 0.129
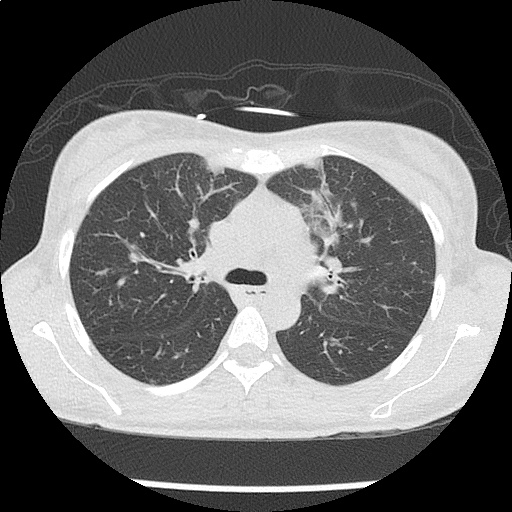
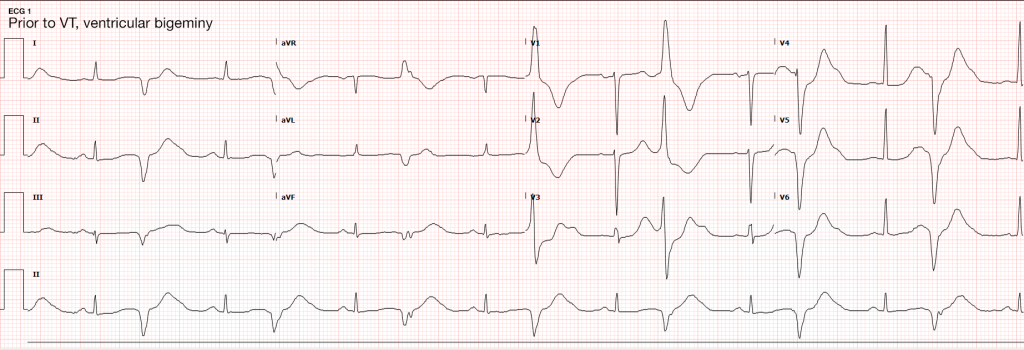
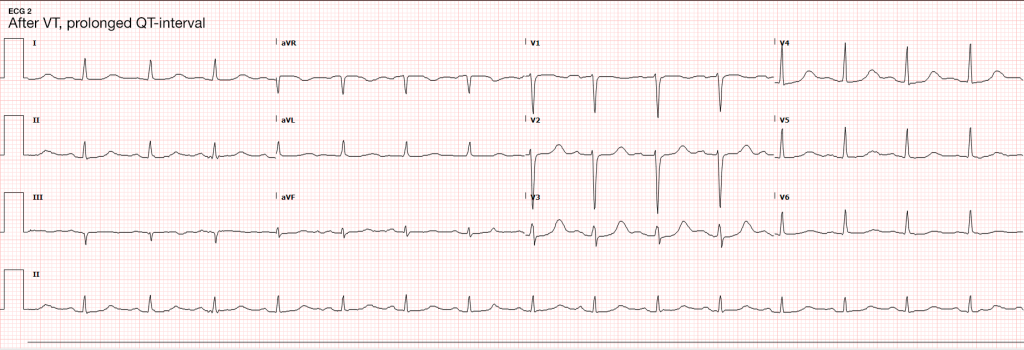
ECG
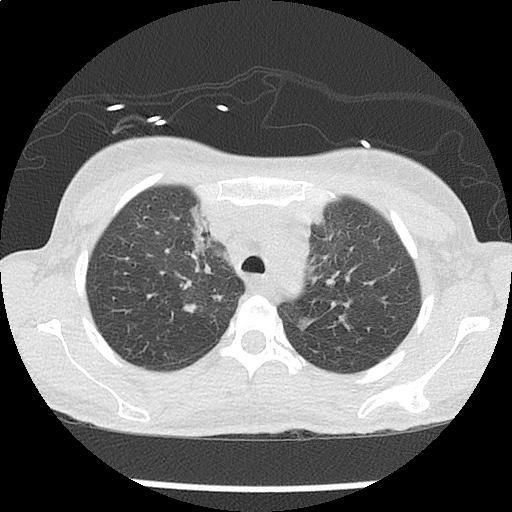
Imaging
- CXR: Negative acute.
- CT Head: Negative acute.
- CT Cardiac: NICM, EF 35%.
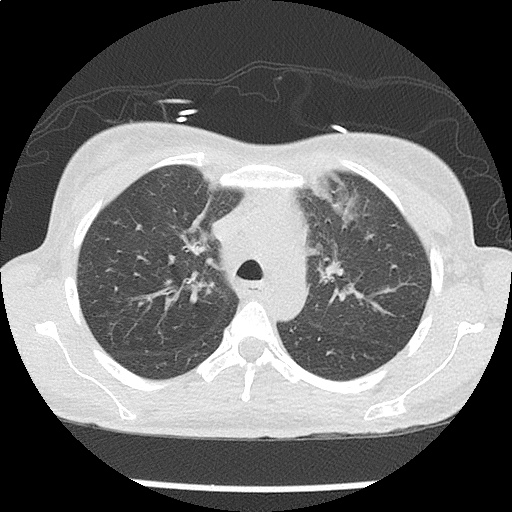
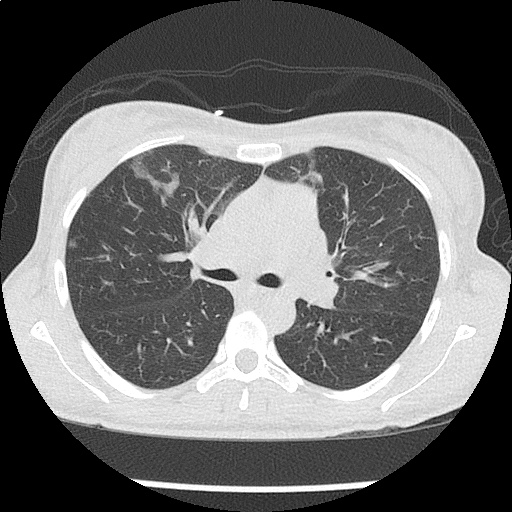
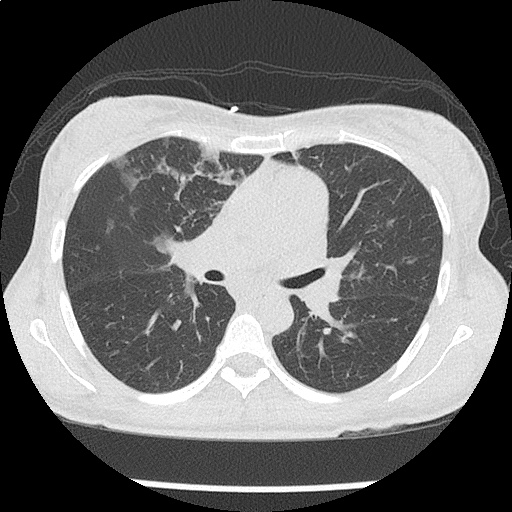
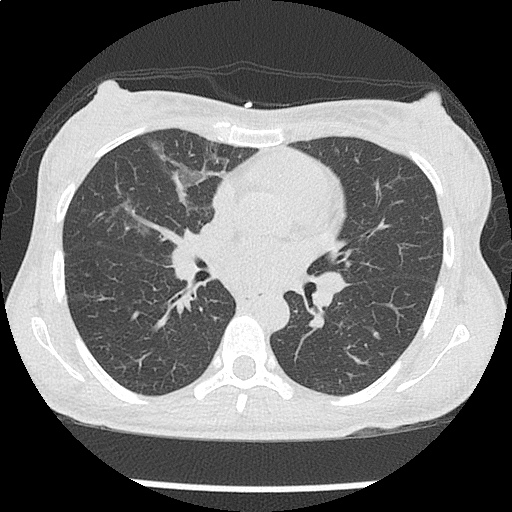
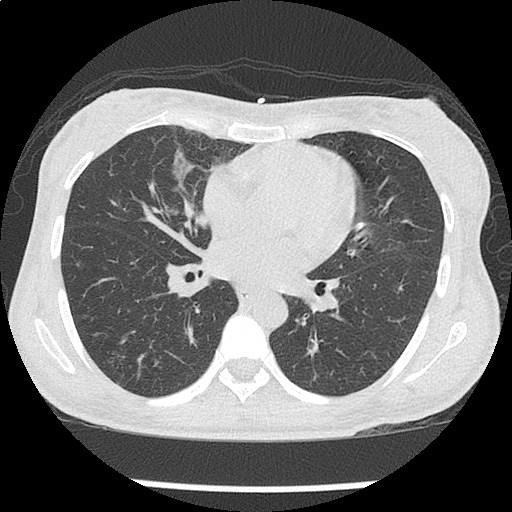
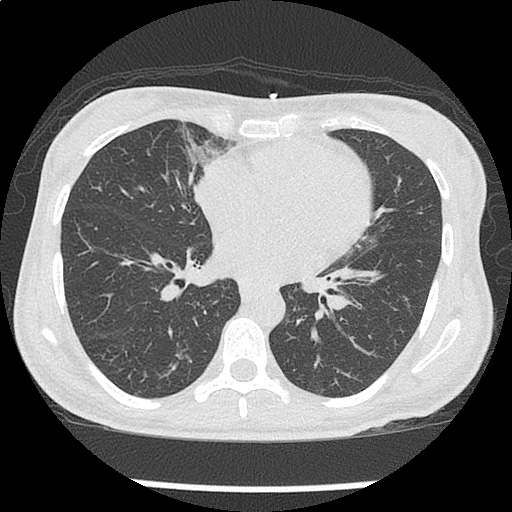
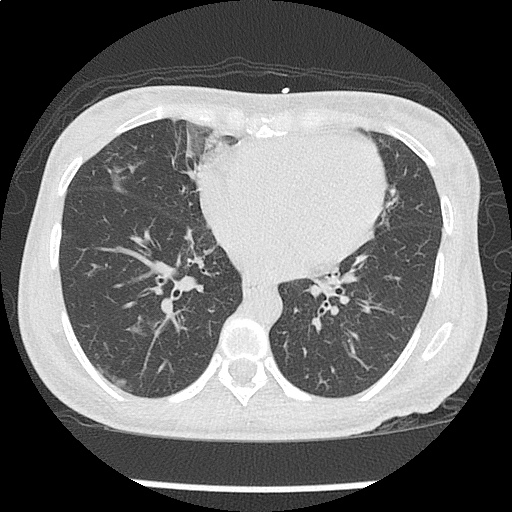
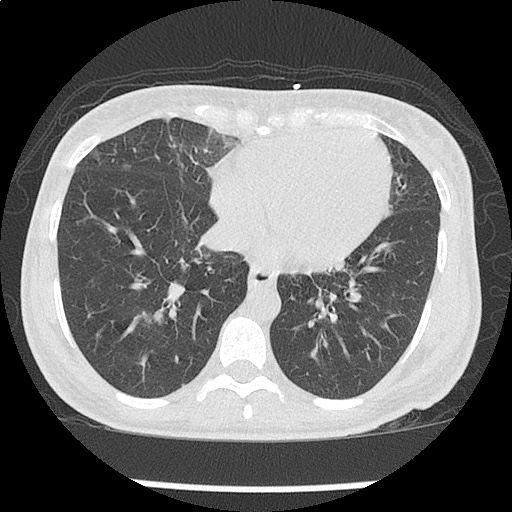
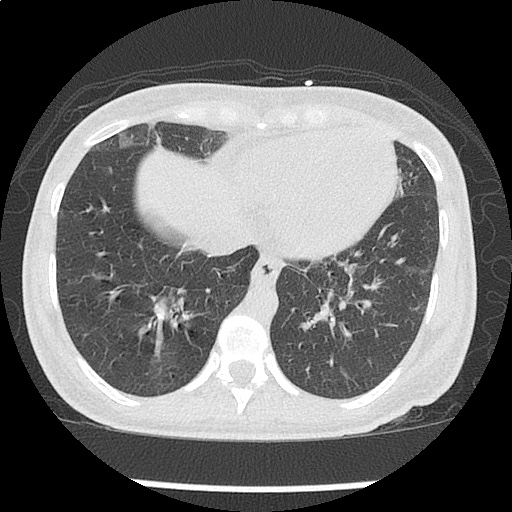
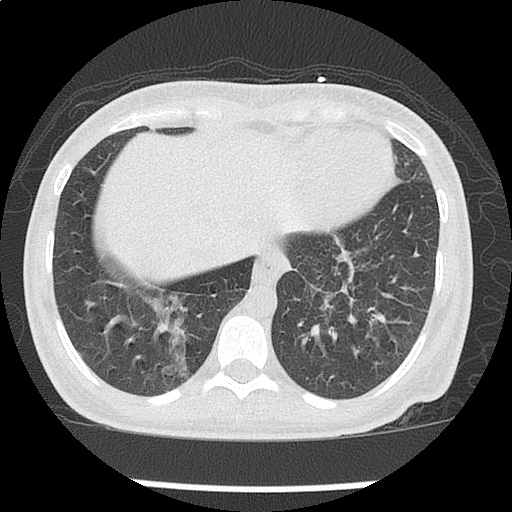
CT Chest non-contrast
- Diffuse patchy GGO (pulmonary edema, atypical pneumonia, alveolar hemorrhage, others).
- Multiple bilateral pulmonary nodules.
- Possible pulmonary arterial hypertension.
Hospital Course
The patient’s evaluation in the emergency department was concerning for severe sepsis secondary to suspected pulmonary source (given association of fever with cough, hypoxia and abnormal chest imaging findings). The patient had persistent alteration in mental status concerning for CNS infection. While preparing for lumbar puncture, cardiac monitoring revealed sustained polymorphic ventricular tachycardia without appreciable pulse. CPR was initiated, amiodarone 150mg IV push administered and at first pulse check a perfusing sinus rhythm was noted with immediate recovery of prior baseline mental status. Amiodarone load was continued and additional potassium sulfate (PO and IV) was administered. Review of telemetry monitoring revealed preceding 30-45 minutes of non-sustained ventricular tachycardia. The patient had two more episodes of sustained ventricular tachycardia requiring defibrillation. The patient was admitted to the medical intensive care unit for continued management.
#Sustained Ventricular Tachycardia
Initially attributed to critical hypokalemia and hypomagnesemia. However, after appropriate repletion serial ECG’s continued to demonstrate prolonged QT interval (possibly acquired secondary to medications, later review revealed multiple promotility agents for treatment of gastroparesis which could contribute to QT-prolongation including erythromycin and metoclopramide, also associated with endocrinopathies). Early echocardiography demonstrated global hypokinesis with estimated EF 30-35%. This was initially attributed to severe sepsis, as well as recurrent defibrillation. However, cardiac CT after resolution of acute illness showed persistent depressed ejection fraction, no evidence of coronary atherosclerosis. The presence of non-ischemic cardiomyopathy (may be attributable to chronic endocrine dysfunction or prior history of methamphetamine abuse) associated with malignant dysrhythmias warranted ICD placement for secondary prevention which the patient was scheduled to receive.
#Severe Sepsis
Attributed to pulmonary source given CT findings, healthcare associated and covered broadly. Mental status gradually improved and returned to baseline. CT head was negative, lumbar puncture deferred.
#Hypokalemia
Unclear etiology. Adrenal insufficiency commonly associated with hyperkalemia and no history of surreptitious fludrocortisone use. Possibly secondary to GI losses. Improved with repletion.
#Autoimmune Polyglandular Syndrome
Started on stress-dose steroids in emergency department. Transiently developed DKA which was reversed appropriately and hydrocortisone was tapered to home regimen. Home levothyroxine was resumed.
Endocrine Emergencies: Hyperthyroidism
Symptoms
| Constitutional | Weight loss, heat intolerance, perspiration |
| Cardiopulmonary | Palpitations, chest pain, dyspnea |
| Neuropsychiatric | Tremor, anxiety, double vision, muscle weakness |
| Neck | Fullness, dysphagia, dysphonia |
| Musculoskeletal | Extremity swelling |
| Reproductive | Irregular menses, decreased libido, gynecomastia |
Signs
| Vital signs | Tachycardia, widened pulse pressure, fever |
| Cardiovascular | Hyperdynamic precordium, CHF, atrial fibrillation, systolic flow murmur |
| Ophthalmologic | Widened palpebral fissure, periorbital edema, proptosis, diplopia, restricted superior gaze |
| Neurologic | Tremor, hyperreflexia, proximal muscle weakness |
| Dermatologic | Palmar erythema, hyperpigmented plaques or non-pitting edema of tibia |
| Neck | Enlarged or nodular thyroid |
Thyroid Storm
Essentially an exaggeration of thyrotoxicosis featuring marked hyperthermia (104-106°F), tachycardia (HR > 140bpm), and altered mental status (agitation, delirium, coma).
- Precipitants
- Medical: Sepsis, MI, CVA, CHF, PE, visceral ischemia
- Trauma: Surgery, blunt, penetrating
- Endocrine: DKA, HHS, hypoglycemia
- Drugs: Iodine, amiodarone, inhaled anesthetics
- Pregnancy: post-partum, hyperemesis gravidarum
Scoring (Burch, Wartofsky)
| Fever | |
| 99-100 | 5 |
| 100-101 | 10 |
| 101-102 | 15 |
| 102-103 | 20 |
| 103-104 | 25 |
| >104 | 30 |
| Tachycardia | |
| 90-110 | 5 |
| 110-120 | 10 |
| 120-130 | 15 |
| 130-140 | 20 |
| >140 | 25 |
| Mental Status | |
| Normal | 0 |
| Mild agitation | 10 |
| Extreme lethargy | 20 |
| Coma, seizure | 30 |
| CHF | |
| Absent | 0 |
| Mild (edema) | 5 |
| Moderate (rales, atrial fibrillation) | 10 |
| Pulmonary edema | 15 |
| GI | |
| None | 0 |
| Nausea/vomiting, abdominal pain | 10 |
| Jaundice | 20 |
| Precipitating Event | |
| None | 0 |
| Present | 10 |
- >45: thyroid storm
- 25-44: impending thyroid storm
- <25: unlikely thyroid storm
Management
- Supportive measures
- Volume resuscitation and cooling
- Benzodiazepines for agitation
- Beta-blockade
- Propranolol 60-80mg PO q4h
- Propranolol 0.5-1.0mg IV, repeat q15min then 1-2mg q3h
- Esmolol continuous infusion
- Endocrinology consultation
- PTU, SSKI
- Precipitants
- Critical illness: sepsis (especially PNA), CVA, MI, CHF, trauma, burns
- Endocrine: DKA, hypoglycemia
- Drugs: amiodarone, lithium, phenytoin, rifampin, medication non-adherence
- Environmental: cold exposure
- Recognition
- History: hypothyroidism, thyroidectomy scar and acute precipitating illness
- Hypothermia: temp <95.9°F (or normal in presence of infection)
- AMS: lethargy, confusion, coma, agitation, psychosis, seizures
- Hypotension: refractory to volume resuscitation and pressors
- Bradypnea: with hypercapnia and hypoxia
- Hyponatremia
- Airway protection
- Fluid resuscitation
- Thyroid hormone replacement
- Young, otherwise healthy patients: T3 10ug IV q4h
- Elderly, cardiac compromise: 300ug IV x1
- Hydrocortisone: 50-100mg IV q6-8h
- Treat precipitating illness
- Maintenance
- Hydrocortisone 20mg qAM, 10mg qPM
- Fludrocortisone 50-100ug daily
- Minor illness (x2)
- Hydrocortisone 40mg qAM, 20mg qPM
- Fludrocortisone 50-200ug daily
- Adrenal Crisis
- Dexamethasone 4mg IV or hydrocortisone 100mg IV
- 2-3L 0.9% NaCl
- Treat precipitating illness
- Causes
- GI losses (diarrhea, laxative use)
- Renal losses (hyperaldosteronism, diuretics)
- Cellular shifts (alkalosis)
- ECG changes
- U-waves 4
- T-wave flattening
- Ventricular arrhythmias (exacerbated with digoxin use)
- Treatment
- Maximum rate 10-20mEq/h with ECG monitoring
- If malignant ventricular arrhythmias or arrest imminent, consider more rapid administration (10mEq over 5 minutes)
- Causes
- GI, renal losses
- Thyroid dysfunction
- Treatment
- 1-2g IV over 5-60 minutes or IVP for Torsades
- Sharma, A., & Levy, D. (2009). Thyroid and Adrenal Disorders. In Rosen’s Emergency Medicine (8th ed., Vol. 2, pp. 1676-1692). Elsevier Health Sciences.
- Savage MW, Mah PM, Weetman AP, Newell-Price J. Endocrine emergencies. Postgrad Med J. 2004;80(947):506–515. doi:10.1136/pgmj.2003.013474.
- ECC Committee, Subcommittees and Task Forces of the American Heart Association. 2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2005;112(24 Suppl):IV1–203. doi:10.1161/CIRCULATIONAHA.105.166550.
- Levis JT. ECG diagnosis: hypokalemia. Perm J. 2012;16(2):57.
Endocrine Emergencies: Hypothyroidism
Symptoms
| Constitutional | Weight gain, cold intolerance, fatigue |
| Cardiopulmonary | Dyspnea, decreased exercise capacity |
| Neuropsychiatric | Impaired concentration and attention |
| Musculoskeletal | Extremity swelling |
| Gastrointestinal | Constipation |
| Reproductive | Irregular menses, erectile dysfunction, decreased libido |
| Integumentary | Coarse hair, dry skin, alopecia, thin nails |
Signs
| Vital signs | Bradycardia, hypothermia |
| Cardiovascular | Prolonged QT, increased ventricular arrhythmia, accelerated CAD, diastolic heart failure, peripheral edema |
| Neurologic | Lethargy, slowed speech, agitation, seizures, ataxia/dysmetria, mononeuropathy, delayed relaxation of reflexes |
| Musculoskeletal | Proximal myopathy, pseudohypertrophy, polyarthralgia |
| Gastrointestinal | Ileus |
Myxedema Coma
Management
Interpretation of Thyroid Function Tests
| Condition | TSH | T4 |
|---|---|---|
| None | Normal | Normal |
| Hyperthyroidism | Low | High |
| Hypothyroidism | High | Low |
| Subclinical hyperthyroidism | Low | Normal |
| Subclinical hypothyroidism | High | Normal |
| Sick euthyroid | Low | Low |
Endocrine Emergencies: Adrenal Insufficiency
Either primary due to adrenal gland failure (often secondary to autoimmune destruction), or secondary most often due to exogenous glucocorticoid administration (usually requiring more than 30mg/day for > 3wks).
Symptoms
| Constitutional | Weakness, fatigue |
| Gastrointestinal | Anorexia, nausea, cramping |
| Neuropsychiatric | Depression, apathy |
| Reproductive | Amenorrhea, decreased libido |
| Musculoskeletal | Myalgia, arthralgia |
Signs
| General | Hyponatremia, orthostatic hypotension, low-grade fever |
| Primary | Hyperpigmentation, hyperkalemia, hyperchloremia, acidosis |
| Secondary | Hypoglycemia |
Management
Life-Threatening Electrolyte Abnormalities3
Critical Hypokalemia
Critical Hypomagnesemia
Conclusion
Unfortunately, this patient’s comprehensive clinical picture does not fit neatly into a particular category of endocrinologic pathology. Her underlying autoimmune disorder manifests both primary adrenal and thyroid dysfunction. Components of the patient’s presentation are suggestive of critical hypothyroidism (myxedema coma) including alteration in mental status, QT-prolongation and hyponatremia as well as possible precipitant of pneumonia. However, despite elevated TSH, the patient’s free T4 level was within normal range. Also absent was hypoventilation (the patient was appropriately tachypneic for degree of hypoxia and with resultant respiratory alkalosis) or bradycardia/hypothermia.
Similarly, adrenal insufficiency is typically associated with hyperkalemia, whereas our patient had critical hypokalemia that was determined to be at least a contributory factor to her ventricular dysrhythmia. The etiology of the patient’s hypokalemia remained unexplained.

Pingback: Differential Diagnosis of Nonsustained Ventricular Tachycardia