HPI:
43F with a history of HTN and diastolic heart failure presenting with two days of shortness of breath. Reports that symptoms are worse at night when lying down to sleep and associated with a cough productive of white sputum. She also reports intermittent left-sided chest pain, described as sharp and exacerbated by cough or deep inspiration. She denies fevers/chills, nausea/vomiting, sick contacts or recent travel.
m
PMH:
- Hypertension
- Diabetes Mellitus (Type II)
- Hyperlipidemia
- Diastolic heart failure
PSH:
- Cesarean section
FH:
- Father with MI at 76 years-old
SHx:
- Lives at home.
- Denies tobacco, alcohol or drug abuse.
Meds:
- Lasix 40mg p.o. daily
- Lisinopril 20mg p.o. daily
- Atenolol 50mg p.o. daily
- Omeprazole 20mg p.o. daily
- Lantus 14 units daily
- Novolin 6 units t.i.d
Allergies:
NKDA
Physical Exam:
| VS: | T | 98.2 | HR | 81 | RR | 19 | BP | 219/91 | O2 | 95% RA |
| Gen: | Adult female in no acute distress, alert and responding appropriately to questions. | |||||||||
| HEENT: | PERRL, EOMI, mucous membranes moist. | |||||||||
| CV: | RRR, no murmurs appreciated, no JVD. | |||||||||
| Lungs: | Crackles at right lung base. | |||||||||
| Abd: | Soft, non-tender, non-distended, without rebound/guarding. | |||||||||
| Ext: | 1+ pitting edema in bilateral lower extremities to knee. | |||||||||
| Neuro: | AAOx4, grossly normal peripheral sensation and motor strength. | |||||||||
Labs/Studies:
- Troponin: 0.15
- Procalcitonin: 0.15
- CBC: 10.9/9.1/26.4/296
- BMP: 134/4.6/104/22/56/2.87/214
Imaging:
- CXR: Consolidation involving the majority of the right lung, cardiomegaly.
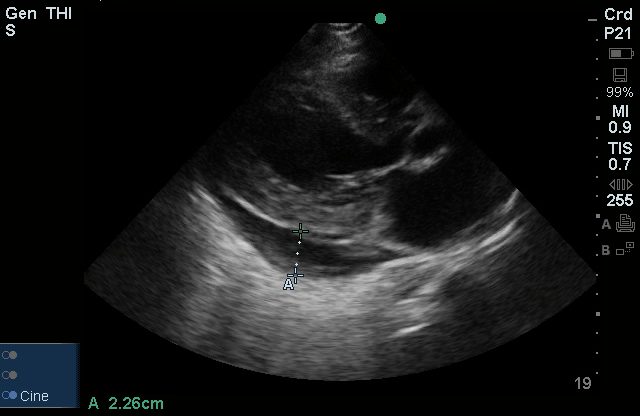
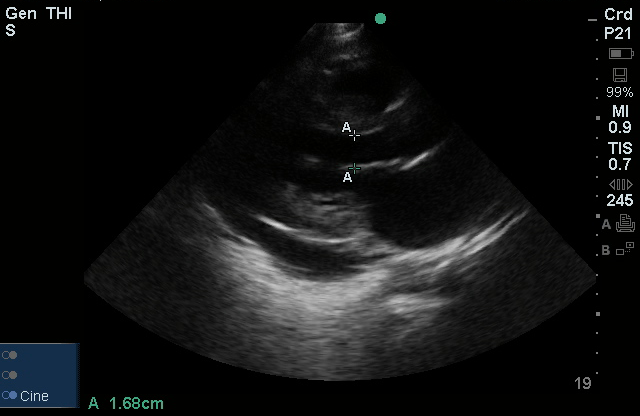
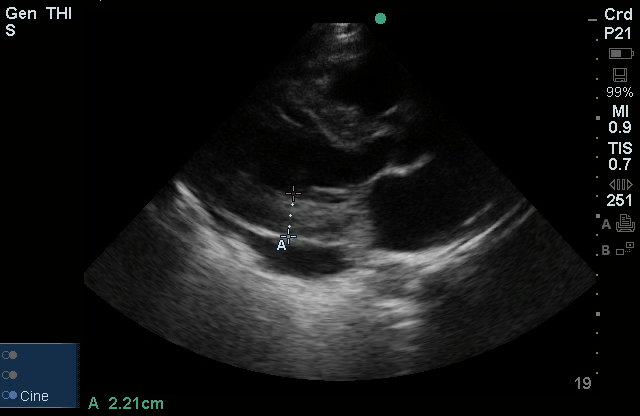
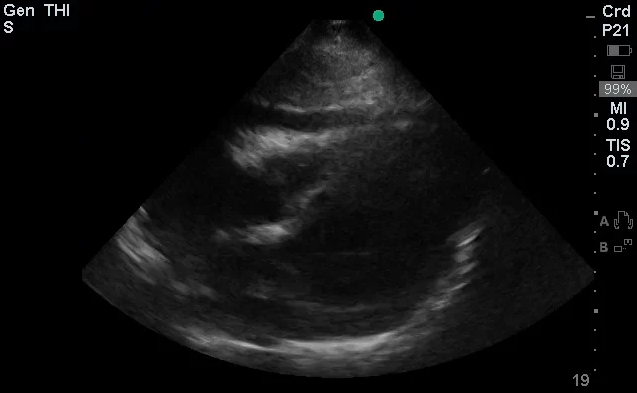
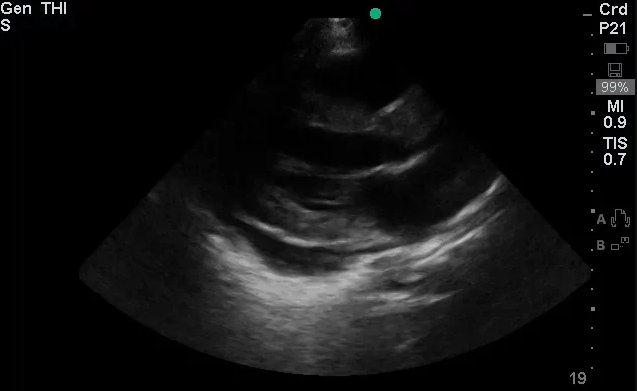
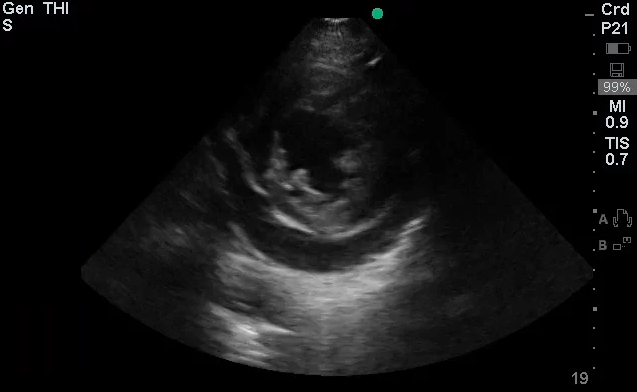
- Bedside Echo: LVEF 55%, concentric LVH, no wall motion abnormality, moderate pericardial effusion noted, RV not collapsed.
Assessment/Plan:
43F with a history of HTN, diastolic heart failure presenting with SOB.
#SOB: CXR finding of right-sided consolidation with history of productive cough, evidence of leukocytosis with neutrophil predominance, and relative hypoxemia suggestive of community-acquired pneumonia. No evidence of systemic inflammatory response. PE unlikely, patient is not bed-bound and alternative diagnosis more likely.
– Start empiric antimicrobial therapy ceftriaxone 1g IV q24h, azithromycin 500mg IV q24h.
#Pericardial Effusion: Noted on bedside echo, no evidence of RV collapse to suggest cardiac tamponade. Also, no JVD and pulsus paradoxus measured at 8mmHg.
– Obtain formal transthoracic echocardiogram to evaluate effusion.
– Consult cardiology if worsening hemodynamics
#Elevated Troponin: No ECG changes suggestive of acute ST-elevation MI. May represent NSTEMI though historical features not consistent with ACS.
– Trend troponin/EKG q.8.h. x3
– Give aspirin 325mg, consider anti-coagulation.
– Consider stress echo prior to discharge
#Elevated Creatinine: Baseline unknown, likely acute component with or without chronic kidney disease.
– Volume resuscitation as tolerated, follow repeat chemistry.
#Hypertension: Asymptomatic, resume home medications.
Physiology of Cardiac Tamponade 1
- Intrapericardial pressure (IPP) normally reflects intrathoracic pressure (ITP).
- Inspiration: low ITP → low RAP → increased RA filling.
- Expiration: high ITP → low LAP → increased LA filling.
- Increased pericardial fluid → increased IPP → increased LA/RA filling pressures (diastolic dysfunction) → increased variation with respiration.
- Earliest hemodynamic change in cardiac tamponade is JVD or IVC dilation.
IVC variation as marker for RAP 1
| IVC Diameter (cm) | Change with Respiration (%) | RAP (mmHg) |
|---|---|---|
| <2.1 | >50% | 0-5 |
| <2.1 | <50% | 5-10 |
| >2.1 | >50% | 5-10 |
| >2.1 | <50% | >15 |
Grading Pericardial Effusions 1
| Grade | Echo-free space (mm) | Size (mL) |
|---|---|---|
| Small | <10 | 100 |
| Moderate | 10-20 | 100-500 |
| Large | >20 | >500 |
History and Physical Exam in Patients with Acute Pericarditis 2,3
| Symptom/Sign | ACS | Pericarditis | PE |
|---|---|---|---|
| Quality | Pressure | Sharp | Sharp |
| Pleuritic | No | Yes | Yes |
| Positional | No | Yes (worse when supine) | No |
| Duration | Minutes to hours | Hours to days | Hours to days |
| Improves with NG | Yes | No | No |
| Friction Rub | No | Yes | No |
| S3 | Maybe | No | No |
Differential Diagnosis of Pericardial Effusion 2-8
References:
- Schairer, J. R., Biswas, S., Keteyian, S. J., & Ananthasubramaniam, K. (2011). A Systematic Approach to Evaluation of Pericardial Effusion and Cardiac Tamponade. Cardiology in Review, 19(5), 233–238. doi:10.1097/CRD.0b013e31821e202c
- Khandaker MH, Espinosa RE, Nishimura RA, et al. Pericardial Disease: Diagnosis and Management. Mayo Clinic Proceedings. 2010;85(6):572-593. doi:10.4065/mcp.2010.0046.
- Lange, RA, Hillis, LD. Clinical practice. Acute pericarditis. The New England journal of medicine. 2004;351(21), 2195–2202. doi:10.1056/NEJMcp041997
- Imazio M, Adler Y. Management of pericardial effusion. Eur Heart J. 2013;34(16):1186-1197. doi:10.1093/eurheartj/ehs372.
- LeWinter MM. Clinical practice. Acute pericarditis. N Engl J Med. 2014;371(25):2410-2416. doi:10.1056/NEJMcp1404070.
- Vakamudi S, Ho N, Cremer PC. Pericardial Effusions: Causes, Diagnosis, and Management. Prog Cardiovasc Dis. 2017;59(4):380-388. doi:10.1016/j.pcad.2016.12.009.
- Imazio M, Mayosi BM, Brucato A, et al. Triage and management of pericardial effusion. J Cardiovasc Med (Hagerstown). 2010;11(12):928-935. doi:10.2459/JCM.0b013e32833e5788.
- Maisch B, Seferović PM, Ristić AD, et al. Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European society of cardiology. Eur Heart J. 2004;25(7):587-610. doi:10.1016/j.ehj.2004.02.002.


Pingback: Differential Diagnosis of Hypotension