Brief HPI:
A 43 year-old female with no reported medical history presents with shortness of breath. She notes 2 months of gradually worsening symptoms associated with unproductive cough and intermittent subjective fevers. Symptoms are worsened with activity and when laying flat. She has no history of similar symptoms in the past.
Vital signs are notable for tachycardia, tachypnea and hypoxia. Examination demonstrates absent breath sounds in the entire right lung field. A plain chest radiograph is obtained and shown below. The patient was placed on non-invasive positive pressure with minimal improvement and an emergent therapeutic thoracentesis was performed. Pleural fluid was exudative and a large volume was submitted for cytology.
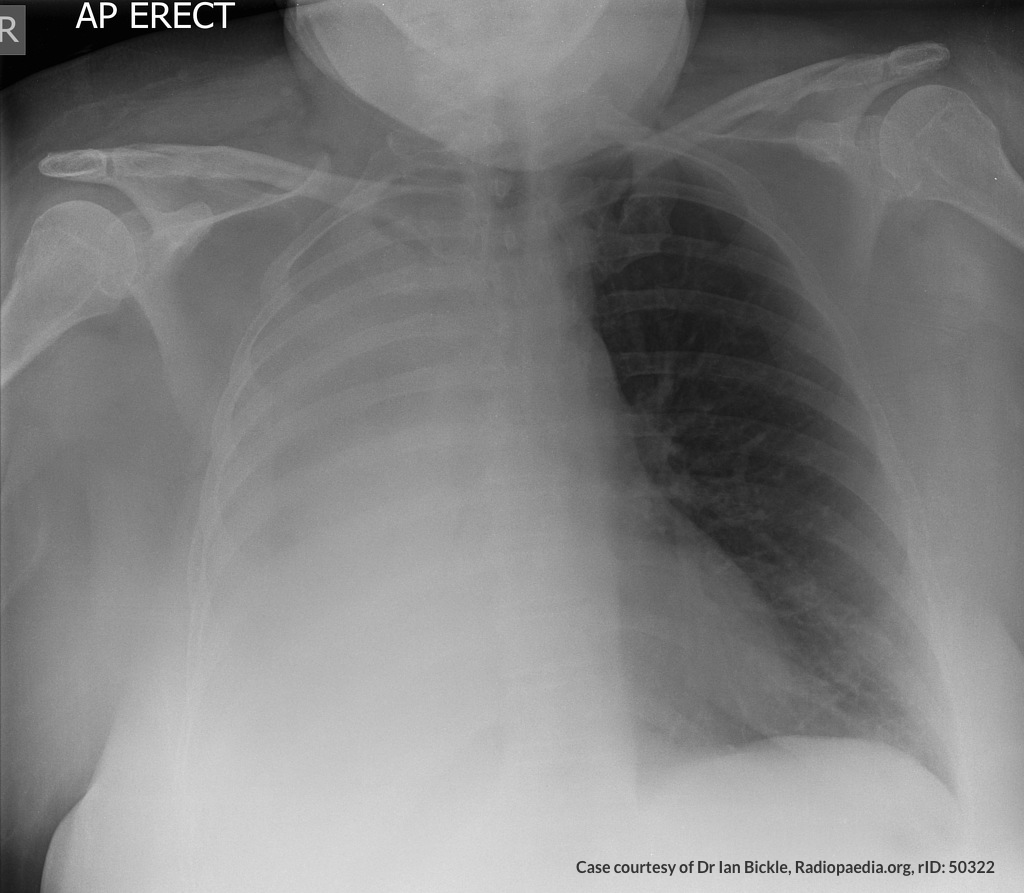 Whiteout right lung field
Whiteout right lung fieldAn Algorithm for the Analysis of Pleural Fluid
References
- Light RW, Girard WM, Jenkinson SG, George RB. Parapneumonic effusions. Am J Med. 1980;69(4):507-512.
- Heffner JE, Brown LK, Barbieri CA. Diagnostic value of tests that discriminate between exudative and transudative pleural effusions. Primary Study Investigators. Chest. 1997;111(4):970-980. doi:10.1378/chest.111.4.970.
- Romero S, Martinez A, Hernandez L, et al. Light’s criteria revisited: consistency and comparison with new proposed alternative criteria for separating pleural transudates from exudates. Respiration. 2000;67(1):18-23. doi:10.1159/000029457.
- Light RW. Clinical practice. Pleural effusion. N Engl J Med. 2002;346(25):1971-1977. doi:10.1056/NEJMcp010731.
- Sahn SA, Huggins JT, San Jose E, Alvarez-Dobano JM, Valdes L. The Art of Pleural Fluid Analysis. Clinical Pulmonary Medicine. 2013;20(2):77-96. doi:10.1097/CPM.0b013e318285ba37.
- Light RW. The Light criteria: the beginning and why they are useful 40 years later. Clinics in Chest Medicine. 2013;34(1):21-26. doi:10.1016/j.ccm.2012.11.006.
- Aggarwal AN, Agarwal R, Sehgal IS, Dhooria S, Behera D. Meta-analysis of Indian studies evaluating adenosine deaminase for diagnosing tuberculous pleural effusion. Int J Tuberc Lung Dis. 2016;20(10):1386-1391. doi:10.5588/ijtld.16.0298.

