Brief H&P
A 27 year-old male with sickle cell disease (HbSC) on hydroxurea and with a history of 2-3 hospitalizations per year for vaso-occlusive pain crises manifested by arthralgias and back pain presents to the emergency department with 3 days of worsening joint pain affecting his entire body but predominantly his knees and lower back. He is familiar with this pain and attempted therapy at home with ibuprofen, then hydrocodone-acetaminophen, and finally hydromorphone without improvement and presented to the emergency department.
On review of systems, he denied chest pain, cough, or shortness of breath. He has some periumbilical abdominal pain but tolerated normal oral intake on the day of presentation without vomiting nor changes in bowel habits. He otherwise denied fevers, peripheral numbness/weakness, urinary or fecal incontinence or retention. He similarly denies trauma, weight loss, night sweats, or intravenous drug use.
Objectively, the patient’s vital signs were normal and he was well-appearing. Mucous membranes were moist and skin turgor was normal. There were no appreciable joint effusions, warmth, nor limitation to active/passive range of motion of any joints. His back had no midline tenderness to palpation or percussion, normal range of motion in all axes and extremity sensation and strength testing were normal. Abdominal and genitourinary examinations were normal. The patient had preserved perineal sensation to light touch and normal rectal tone – a core temperature was obtained which was also normal.
Peripheral access was established and a parenteral dose of hydromorphone equivalent to his home oral dose was administered (0.015mg/kg). Repeat dosing was required at 15 minutes due to persistent pain scale of 10. Diphenhydramine and acetaminophen were also administered, for potential opioid-sparing effects, recognizing the limited evidence to support these relatively benign adjuncts.
Laboratory studies were notable for anemia (though stable compared to baseline measures), appropriate reticulocyte count, no evidence of hemolysis and with normal electrolytes and renal function.
A thorough history and examination did not identify a critical precipitant for the patient’s symptoms which were presumed to be secondary to a vaso-occlusive pain crisis. On reassessment, the patient’s pain was improved and an oral dose of hydromorphone was administered with continued observation and serial reassessments for two hours thereafter. The patient’s hematologist was available for follow-up the subsequent morning and the patient was discharged home.
Pharmacokinetics of Commonly-Used Opiate Analgesics1-3
| Medication | Route | Onset | Peak | Duration |
|---|---|---|---|---|
| Morphine | IV | 5-10min | 20min | 3-5h |
| IM | 15-30min | 30-60min | ||
| PO | 30min | 1h | ||
| Oxycodone | PO | 10-15min | 30-60min | 3-6h |
| Hydrocodone | PO | 10-20min | 4-8h | |
| Fentanyl | IV | <1min | 2-5min | 30-60min |
| Hydromorphone | IV | 5min | 10-20min | 3-4h |
| PO | 15-30min | 30-60min | ||
| Codeine | PO | 30-60min | 60-90min | 4-6h |
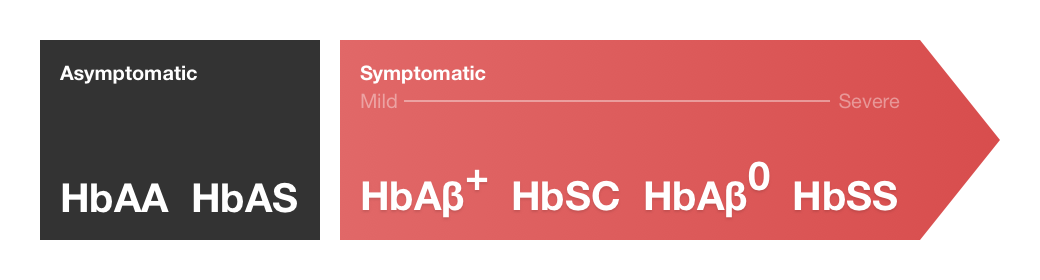
Spectrum of Sickle Cell Trait and Disease4
Algorithm for the Evaluation and Management of Sickle Cell Crises4-10
References:
- Lexicomp Online®, Adult Drug Information, Hudson, Ohio: Lexi-Comp, Inc.; November 4, 2017.
- Trescot AM, Datta S, Lee M, Hansen H. Opioid pharmacology. Pain Physician. 2008;11(2 Suppl):S133-S153.
- Vieweg WVR, Lipps WFC, Fernandez A. Opioids and methadone equivalents for clinicians. Prim Care Companion J Clin Psychiatry. 2005;7(3):86-88.
- Glassberg J. Evidence-based management of sickle cell disease in the emergency department. Emergency Medicine Practice. 2011;13(8):1–20–quiz20.
- Raam R, Mallemat H, Jhun P, Herbert M. Sickle Cell Crisis and You: A How-to Guide. Ann Emerg Med. 2016;67(6):787-790. doi:10.1016/j.annemergmed.2016.04.016.
- Piel FB, Steinberg MH, Rees DC. Sickle Cell Disease. N Engl J Med. 2017;376(16):1561-1573. doi:10.1056/NEJMra1510865.
- Lovett PB, Sule HP, Lopez BL. Sickle cell disease in the emergency department. Emerg Med Clin North Am. 2014;32(3):629-647. doi:10.1016/j.emc.2014.04.011.
- Yawn BP, John-Sowah J. Management of Sickle Cell Disease: Recommendations From the 2014 Expert Panel Report. Vol 92. 2015:1069-1076.
- Zempsky WT. Evaluation and Treatment of Sickle Cell Pain in the Emergency Department: Paths to a Better Future. Clinical Pediatric Emergency Medicine. 2010;11(4):265-273. doi:10.1016/j.cpem.2010.09.002.
- Aliyu ZY, Tumblin AR, Kato GJ. Current therapy of sickle cell disease. Haematologica. 2006;91(1):7-10.