Brief HPI:
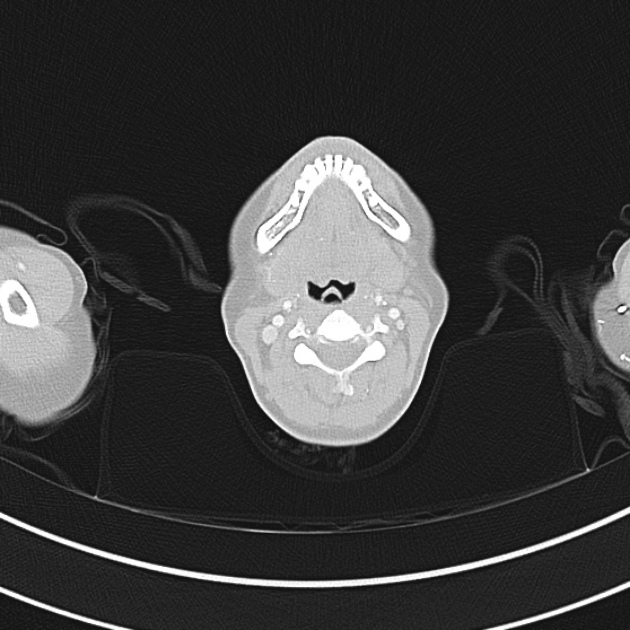
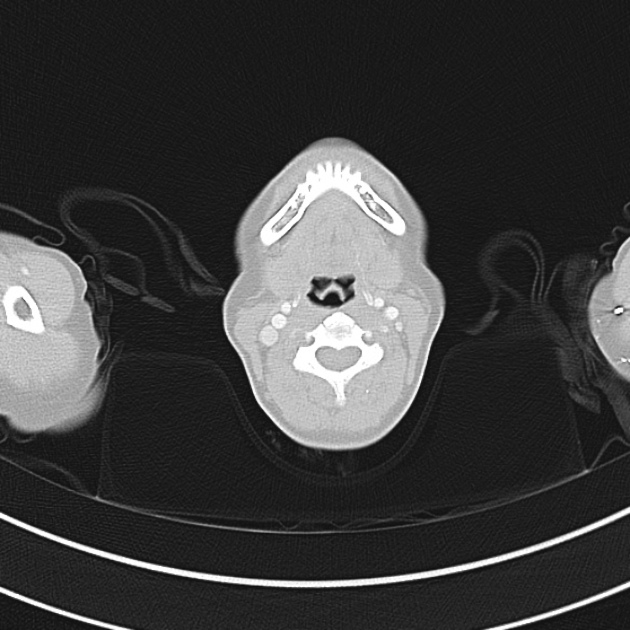
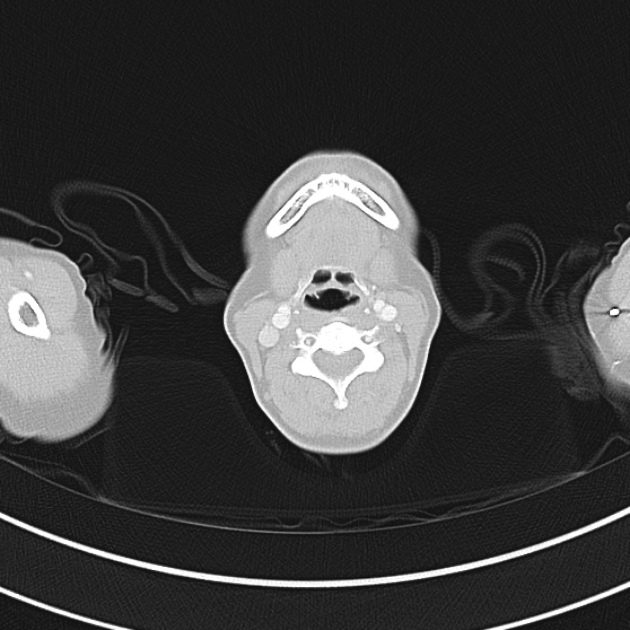
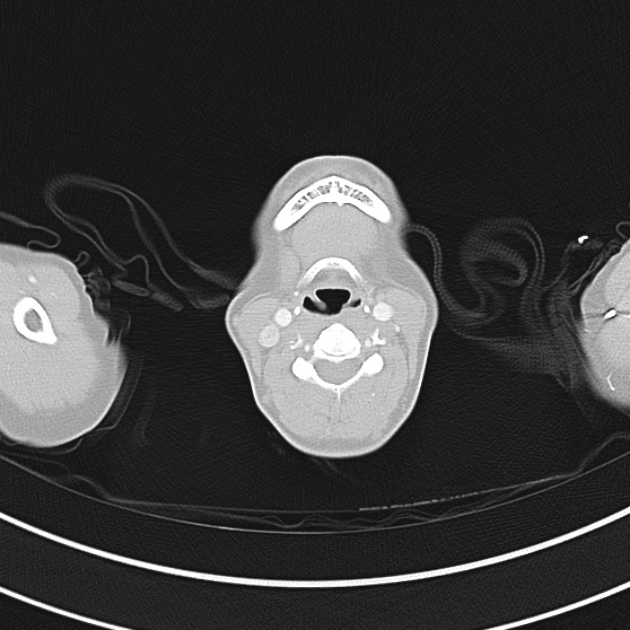
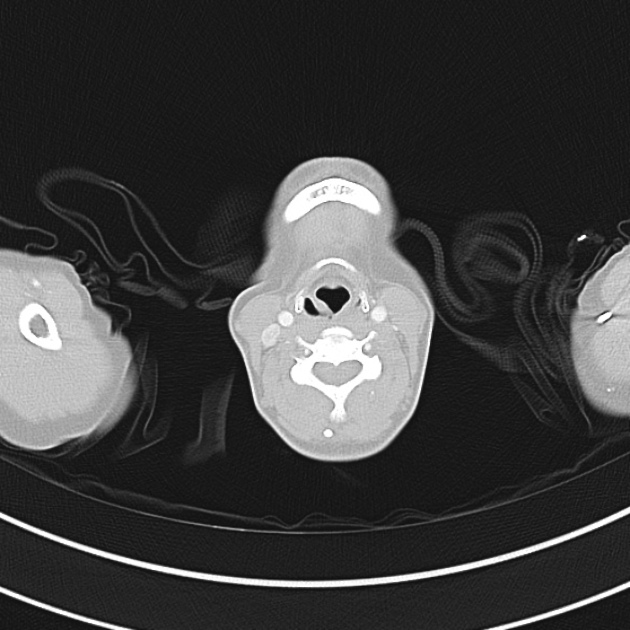
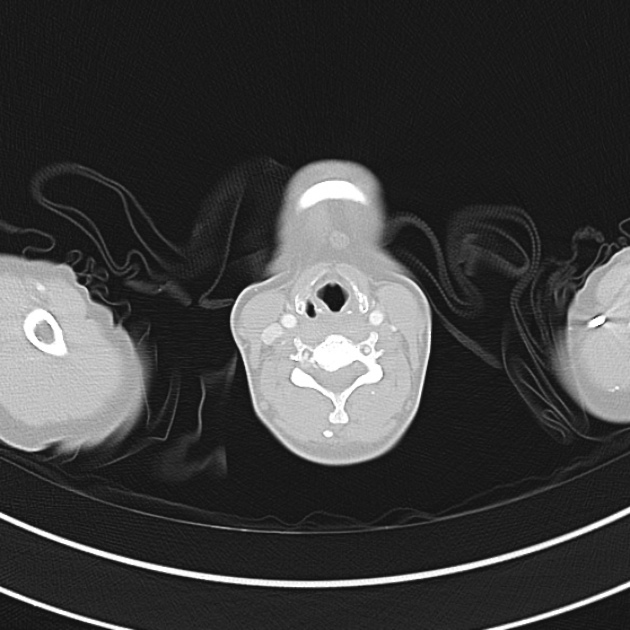
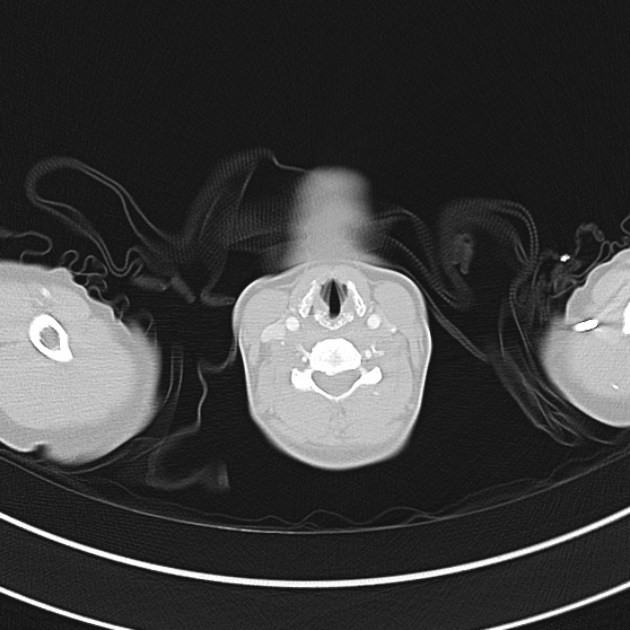
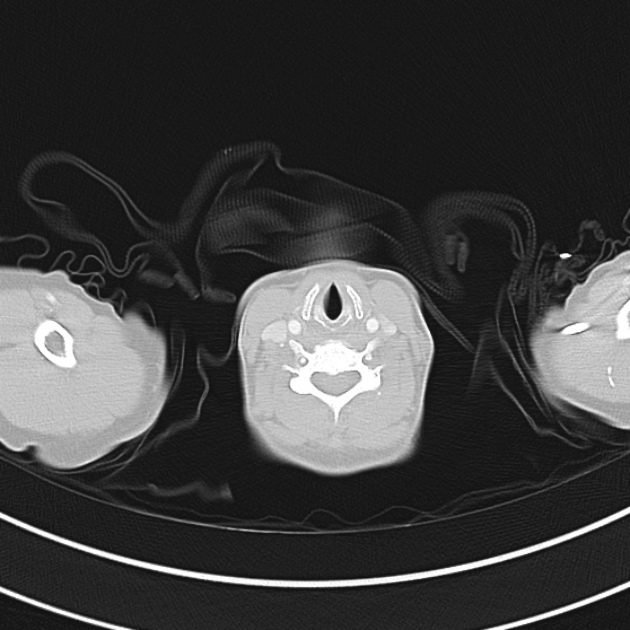
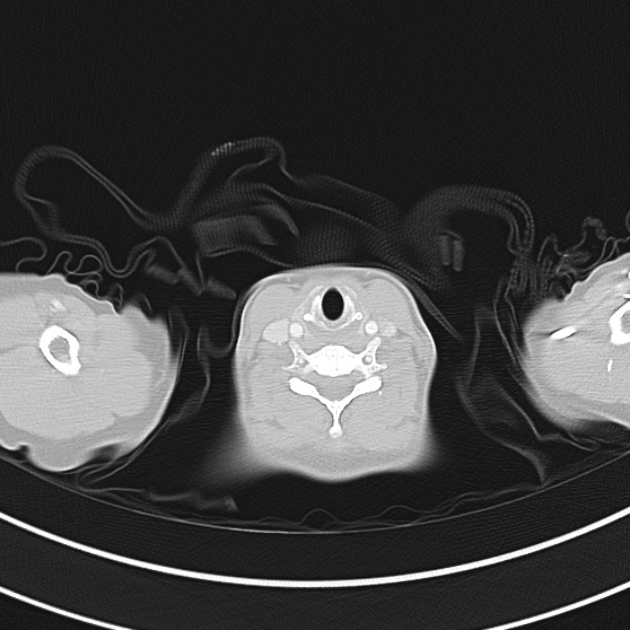
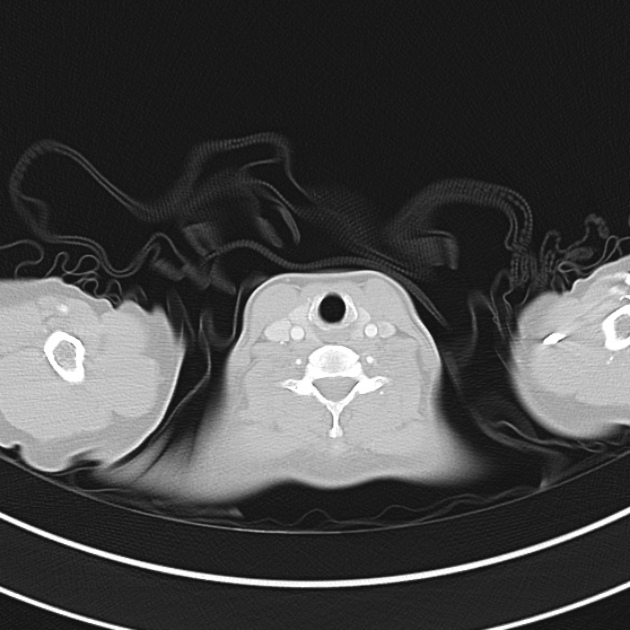
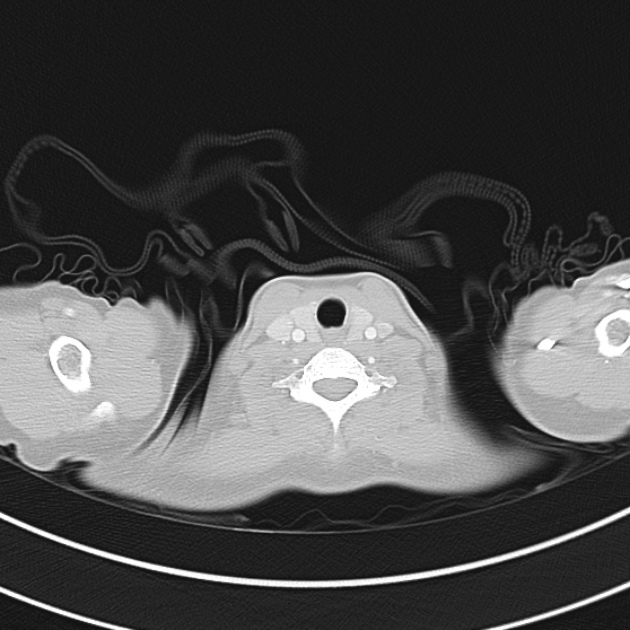
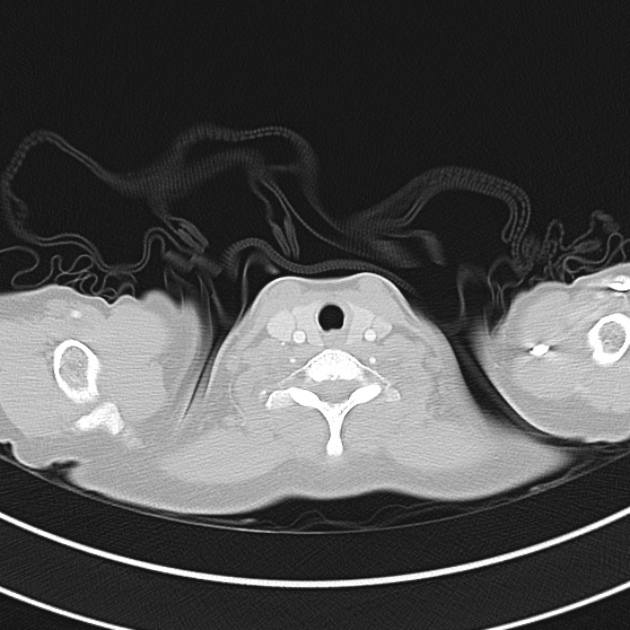
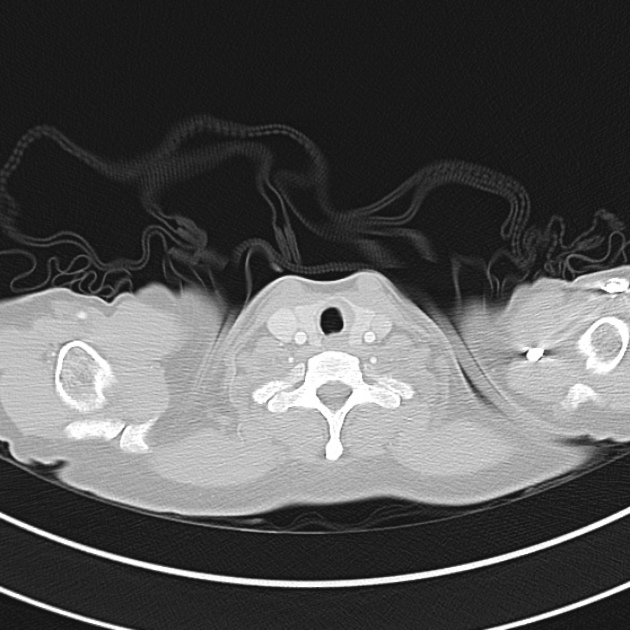
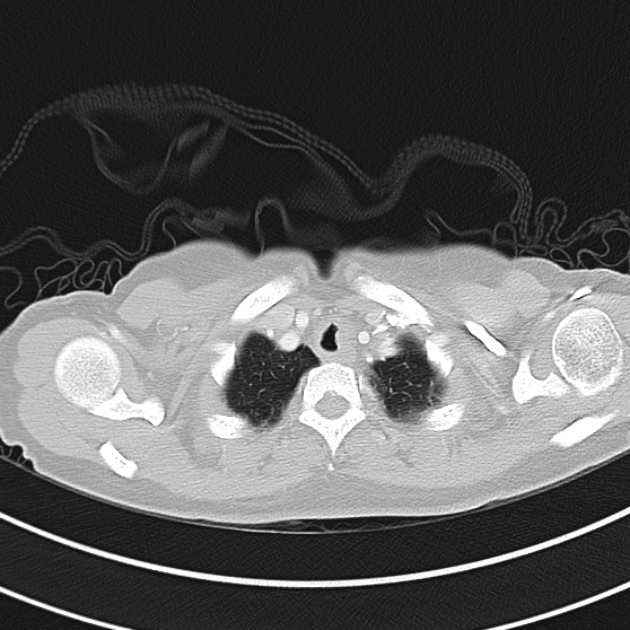
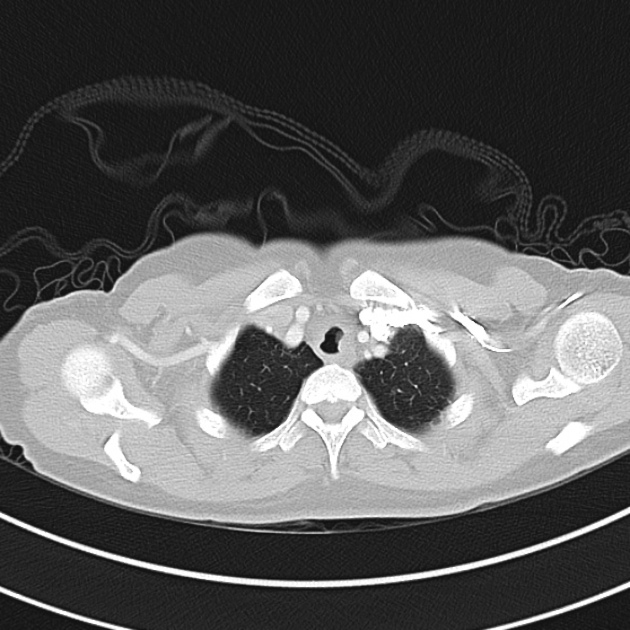
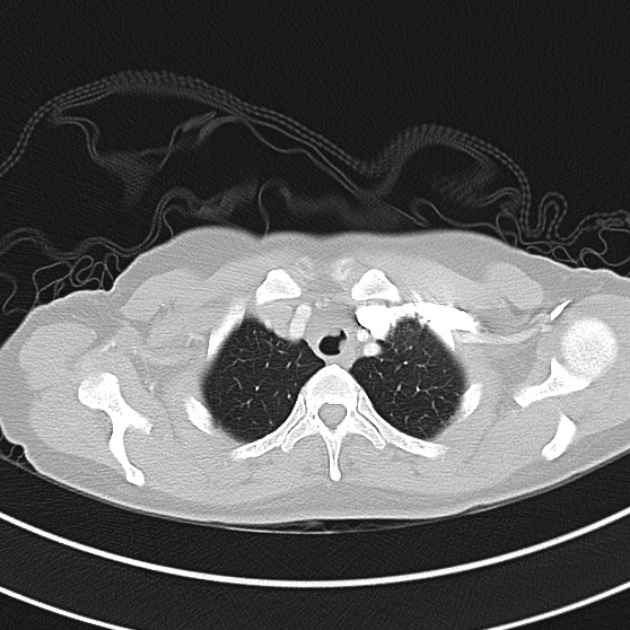
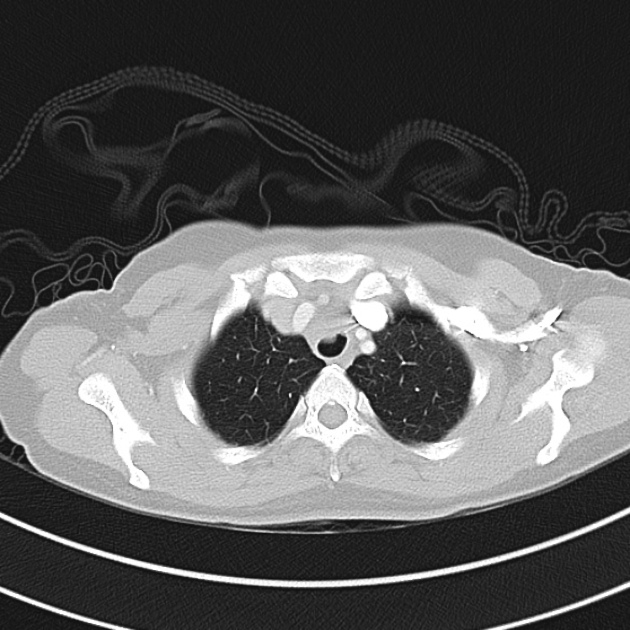
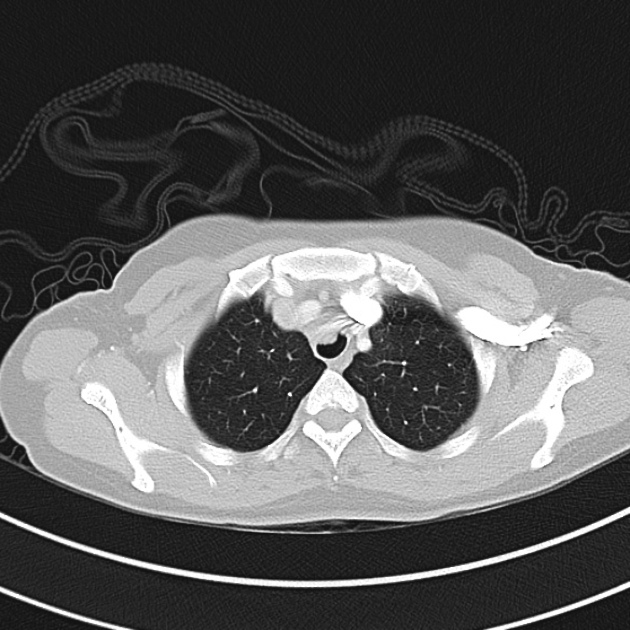
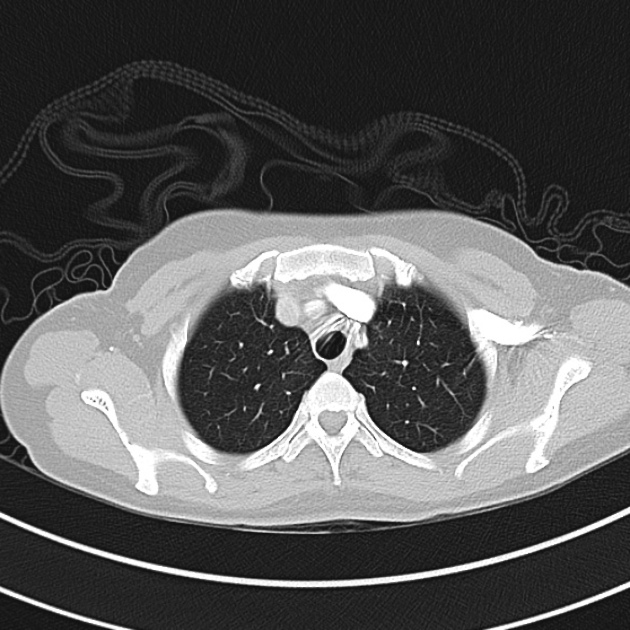
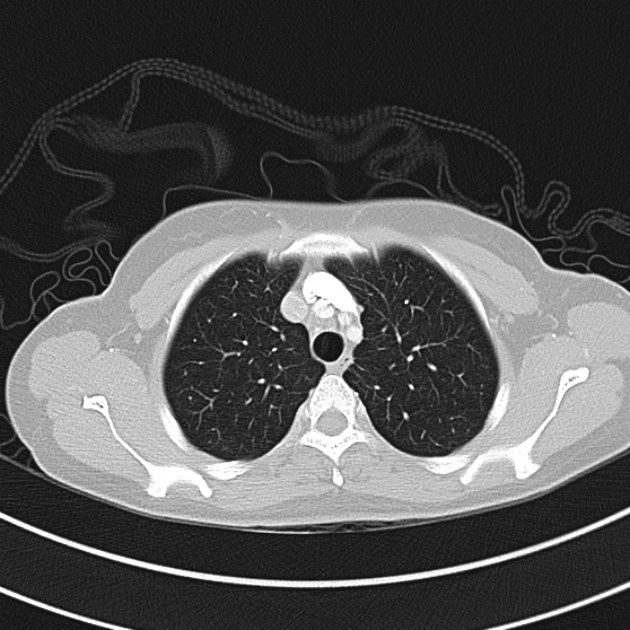
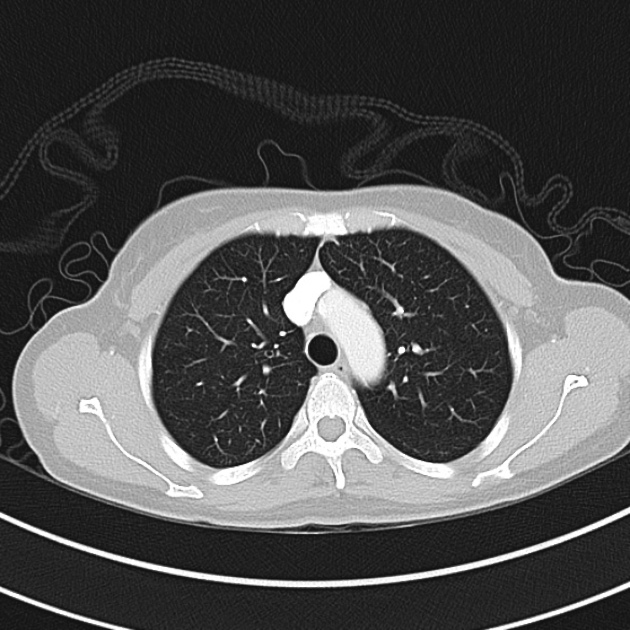
A 6 year-old boy with a history of asthma presents to the emergency department via EMS for dyspnea. The patient is agitated on exam with nasal flaring and intercostal retractions. The parents report that his difficulty breathing started two days ago. The first day his MDI inhaler provided transient relief; however, over the next 24 hours he required nebulized albuterol 3 times with no significant relief. They deny any recent infections or steroid use and state that his immunizations are up-to-date.
On evaluation, vital signs are notable for BP 93/61, HR 140, RR 47, and SpO2 90%. He is afebrile; capillary glucose 113mg/dL. On examination, the patient is agitated with nasal flaring, intercostal retractions, shallow breathing with diminished breath sounds throughout.
Algorithm for the Management of Pediatric Asthma1-11

PASS12
|
Wheezing |
Work of Breathing |
Prolonged Expiration |
| Mild (0) |
None or end-expiration |
Normal or minimal retractions |
Normal or minimally prolonged |
| Moderate (1) |
Throughout expiration |
Intercostal retractions |
Moderately prolonged |
| Severe (2) |
Severe wheezing or absent |
Suprasternal retractions, abdominal wall movement |
Severely prolonged |
This algorithm was developed by Dr. Joshua Niforatos. Joshua is an emergency medicine resident at The Johns Hopkins School of Medicine and an alumnus of the Cleveland Clinic Lerner College of Medicine.
Special thanks to
Dr. Kelly Young, Director of the Pediatric Emergency Medicine Fellowship at Harbor-UCLA Medical Center and
Dr. Adeola Kosoko, Assistant Professor, Assistant Residency Program Director, Director Of Diversity, Inclusion, And Mission at McGovern Medical School for their review of the algorithm.
References
- Rowe, B., Bretzlaff, J., Bourdon, C., Bota, G., Camargo, C. (2000). Magnesium sulfate for treating exacerbations of acute asthma in the emergency department. The Cochrane database of systematic reviews https://dx.doi.org/10.1002/14651858.cd001490
- Camargo, C., Spooner, C., Rowe, B. (2003). Continuous versus intermittent beta-agonists in the treatment of acute asthma. The Cochrane database of systematic reviews https://dx.doi.org/10.1002/14651858.cd001115
- Camargo, C., Rachelefsky, G., Schatz, M. (2009). Managing asthma exacerbations in the emergency department: summary of the National Asthma Education And Prevention Program Expert Panel Report 3 guidelines for the management of asthma exacerbations. Proceedings of the American Thoracic Society 6(4), 357 – 366. https://dx.doi.org/10.1513/pats.p09st2
- Gouin, S., Robidas, I., Gravel, J., Guimont, C., Chalut, D., Amre, D. (2010). Prospective evaluation of two clinical scores for acute asthma in children 18 months to 7 years of age. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine 17(6), 598 – 603. https://dx.doi.org/10.1111/j.1553-2712.2010.00775.x
- Travers, A., Milan, S., Jones, A., Camargo, C., Rowe, B. (2012). Addition of intravenous beta(2)-agonists to inhaled beta(2)-agonists for acute asthma. The Cochrane database of systematic reviews 12(), CD010179. https://dx.doi.org/10.1002/14651858.cd010179
- Jat, K., Chawla, D. (2012). Ketamine for management of acute exacerbations of asthma in children. The Cochrane database of systematic reviews 11(), CD009293. https://dx.doi.org/10.1002/14651858.cd009293.pub2
- Ortiz-Alvarez, O., Mikrogianakis, A., Committee, C. (2012). Managing the paediatric patient with an acute asthma exacerbation. Paediatrics & child health 17(5), 251 – 262. https://dx.doi.org/10.1093/pch/17.5.251
- Jones, B., Paul, A. (2013). Management of acute asthma in the pediatric patient: an evidence-based review. Pediatric emergency medicine practice 10(5), 1 – 23- quiz 23-4.
- Nievas, I., Anand, K. (2013). Severe acute asthma exacerbation in children: a stepwise approach for escalating therapy in a pediatric intensive care unit. The journal of pediatric pharmacology and therapeutics : JPPT : the official journal of PPAG 18(2), 88 – 104. https://dx.doi.org/10.5863/1551-6776-18.2.88
- Rehder, K. (2017). Adjunct Therapies for Refractory Status Asthmaticus in Children. Respiratory care 62(6), 849 – 865. https://dx.doi.org/10.4187/respcare.05174
- Carroll, C., Sala, K. (2013). Pediatric status asthmaticus. Critical care clinics 29(2), 153 – 166. https://dx.doi.org/10.1016/j.ccc.2012.12.001
- Gorelick, M., Stevens, M., Schultz, T., Scribano, P. (2004). Performance of a novel clinical score, the Pediatric Asthma Severity Score (PASS), in the evaluation of acute asthma. Academic Emergency Medicine 11(1), 10 – 18. https://dx.doi.org/10.1197/s1069-6563(03)00579-7