Brief H&P:
A 63 year-old male with a history of hypertension, tobacco use, and nephrolithiasis presents with left-sided flank pain. He notes sudden-onset approximately 4 hours prior to presentation and describes radiation to his groin. Pain was associated with nausea, denies hematuria and states pain is different compared to prior kidney stones. On evaluation, vital signs are notable for tachycardia (114bpm), blood pressure measured at 112/65mmHg. The patient appears uncomfortable and examination is notable for a pulsatile abdominal mass above the umbilicus.
ED Course
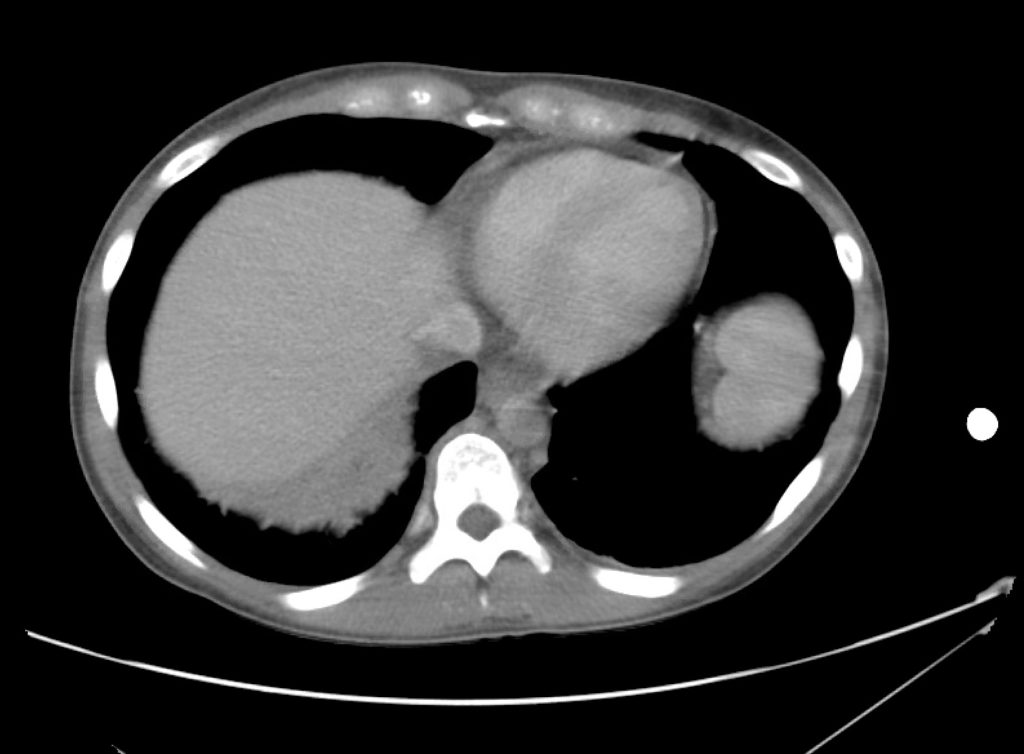
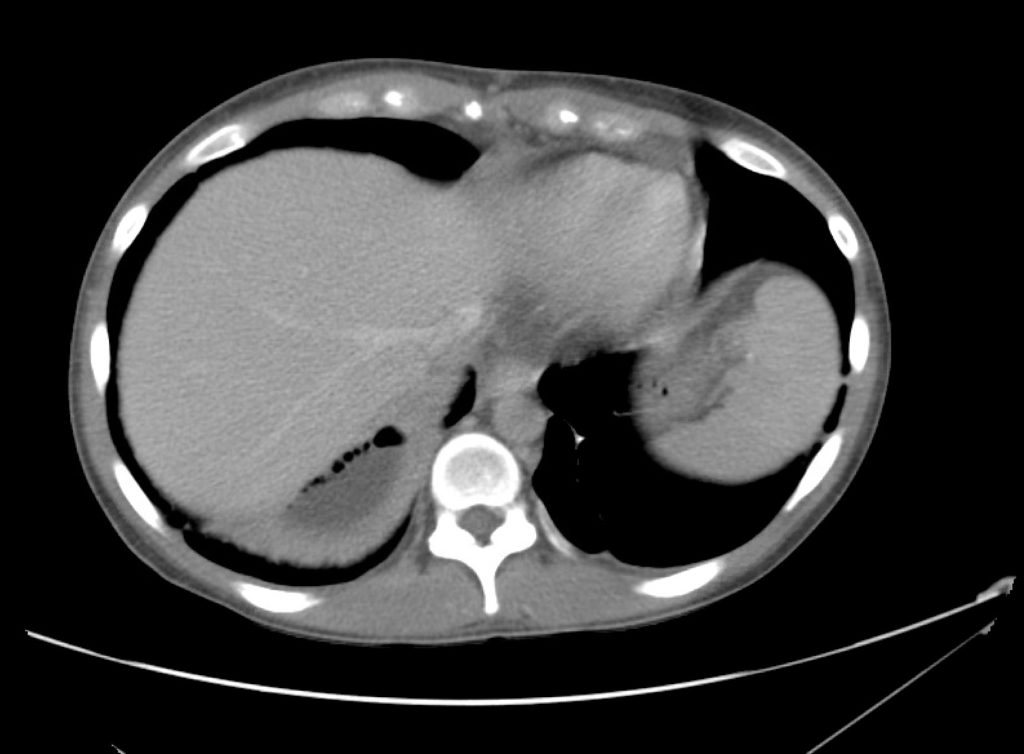
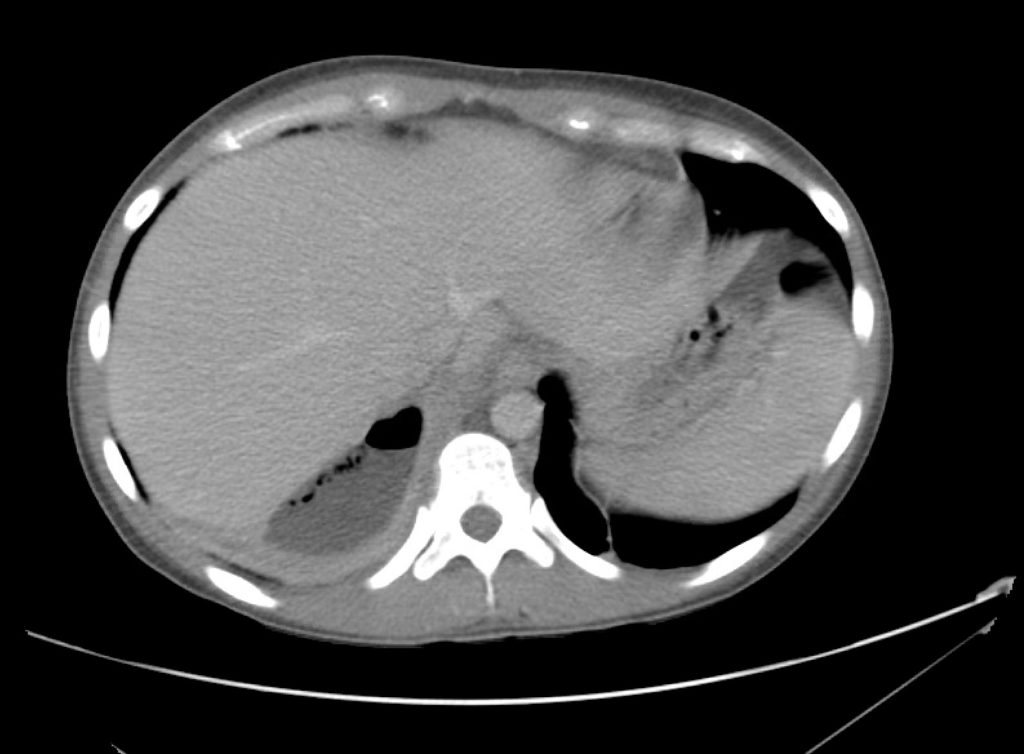
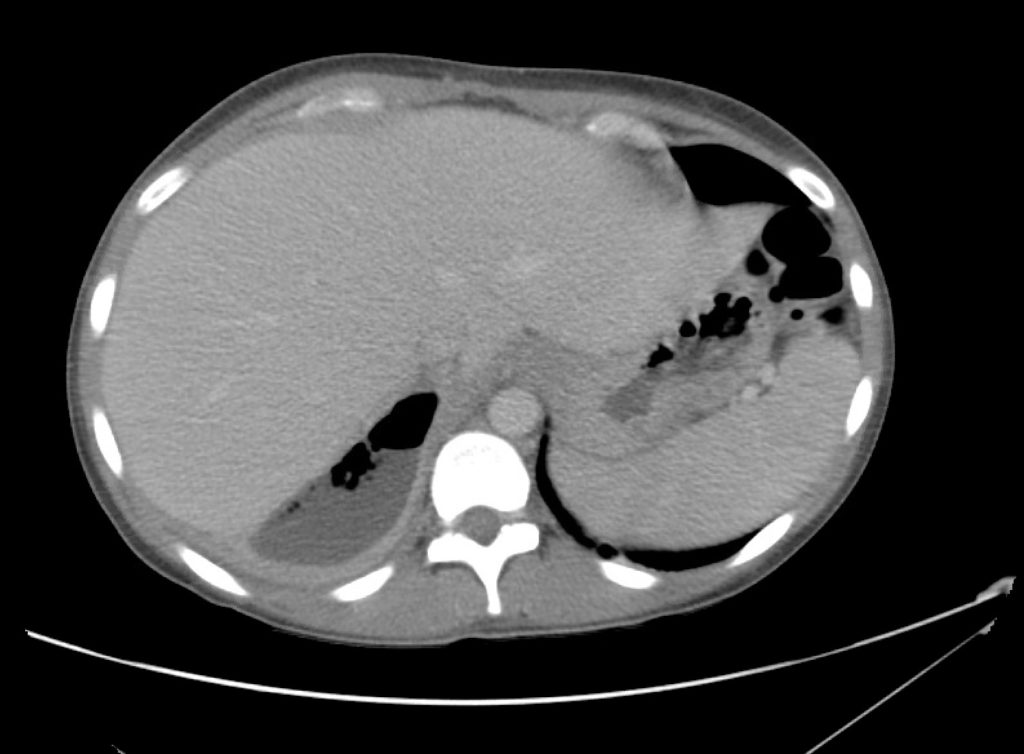
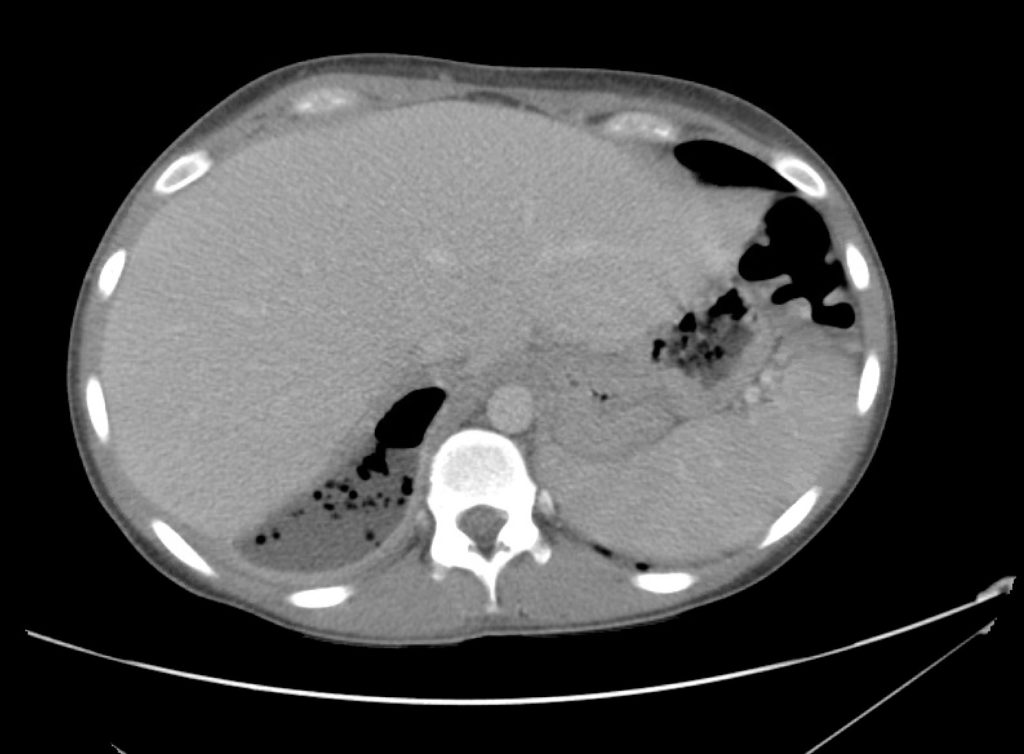
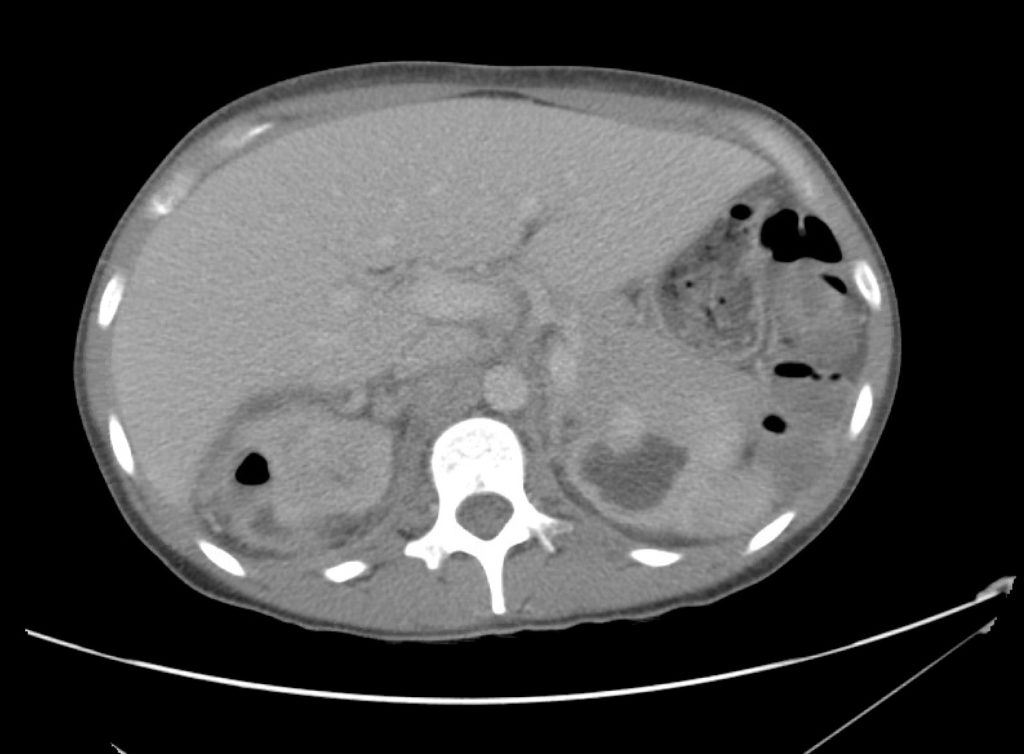
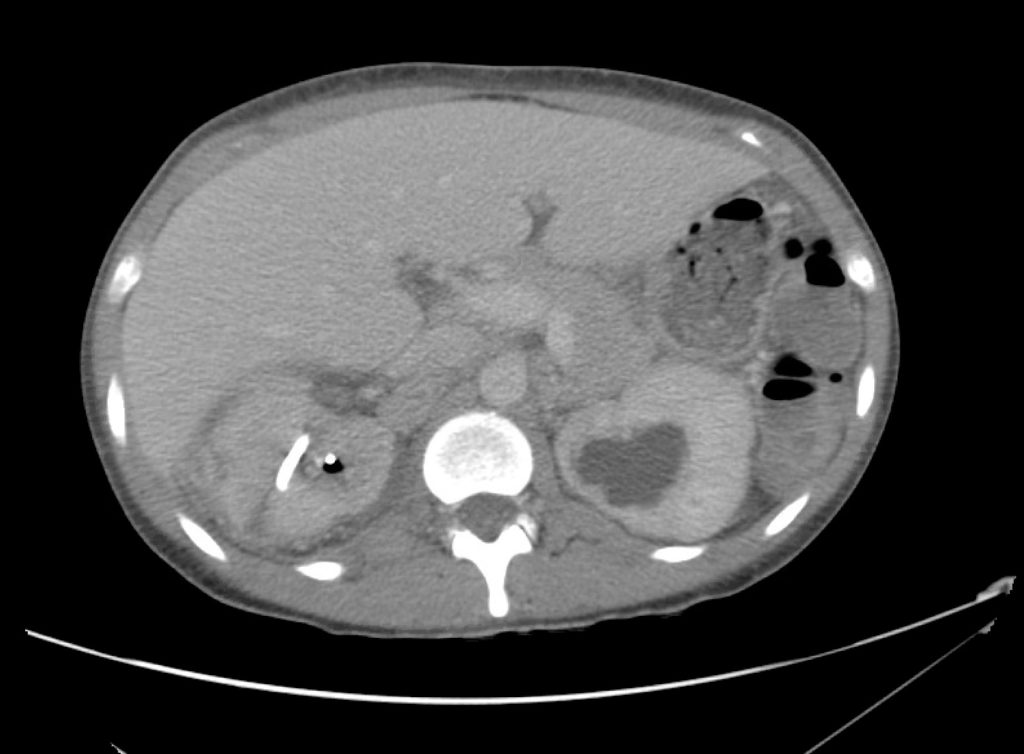
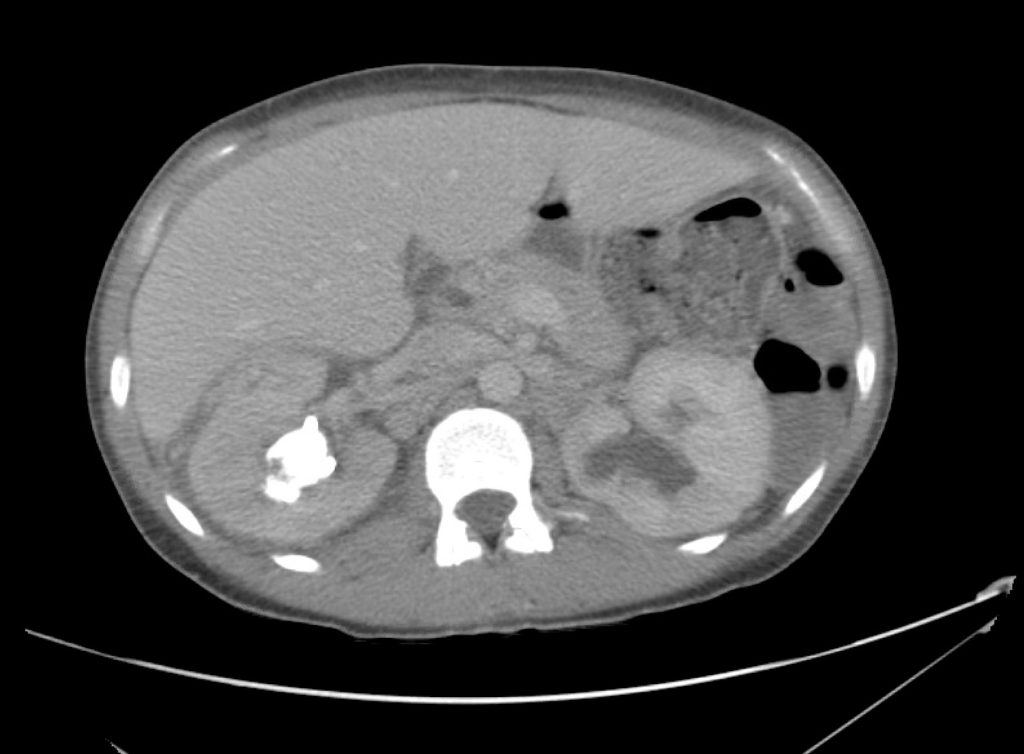
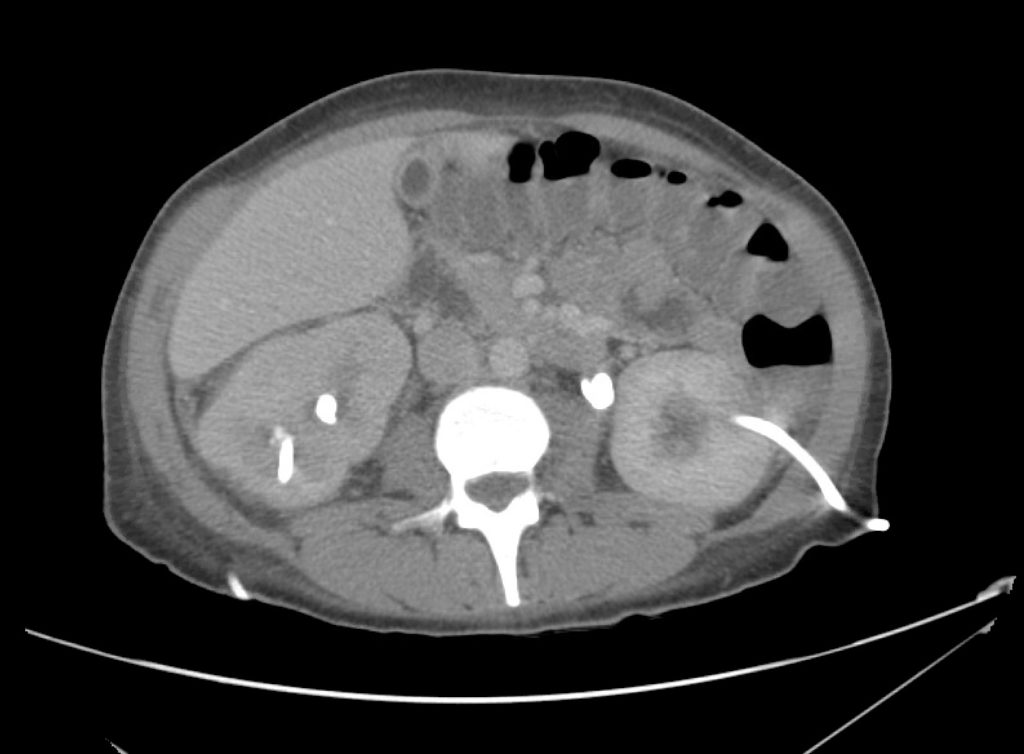
A point-of-care ultrasound is performed which shows no hydronephrosis and an 8cm infrarenal abdominal aortic aneurysm. Vascular surgery was consulted and a CTA was performed revealing ruptured abdominal aortic aneurysm. Uncrossmatched blood products were administered en route to the operating room due to hypotension.
Algorithm for the Evaluation of Flank Pain with Ultrasound
Gallery
The ultrasound images and videos used in this post come from The POCUS Atlas, a collaborative collection focusing on rare, exotic and perfectly captured ultrasound images.
References
- Moore CL, Daniels B, Singh D, Luty S, Molinaro A. Prevalence and clinical importance of alternative causes of symptoms using a renal colic computed tomography protocol in patients with flank or back pain and absence of pyuria. Acad Emerg Med. 2013;20(5):470-478.
- Prince L.A., & Johnson G.A. (2020). Aneurysmal disease. Tintinalli J.E., & Ma O, & Yealy D.M., & Meckler G.D., & Stapczynski J, & Cline D.M., & Thomas S.H.(Eds.),Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 9e. McGraw Hill.
- Bueschen AJ. Flank Pain. In: Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition. Boston: Butterworths; 1990. Chapter 182. Available from: https://www.ncbi.nlm.nih.gov/books/NBK292/
- Carter MR, Green BR. Renal calculi: emergency department diagnosis and treatment. Emerg Med Pract. 2011;13(7):1-17;
- https://wikem.org/wiki/Abdominal_aortic_aneurysm