Brief HPI:
A 28 year-old female with a history of systemic lupus erythematosus and end-stage renal disease without access to scheduled hemodialysis presents to the emergency department with 1 week of worsening dyspnea, fatigue and leg swelling. Her symptoms are reminiscent of prior episodes resolving with hemodialysis. On evaluation, vital signs are normal and laboratory tests demonstrate microcytic anemia (Hb 5.9g/dL) but no hyperkalemia. A plain chest radiograph is normal and the patient ambulates without hypoxia.
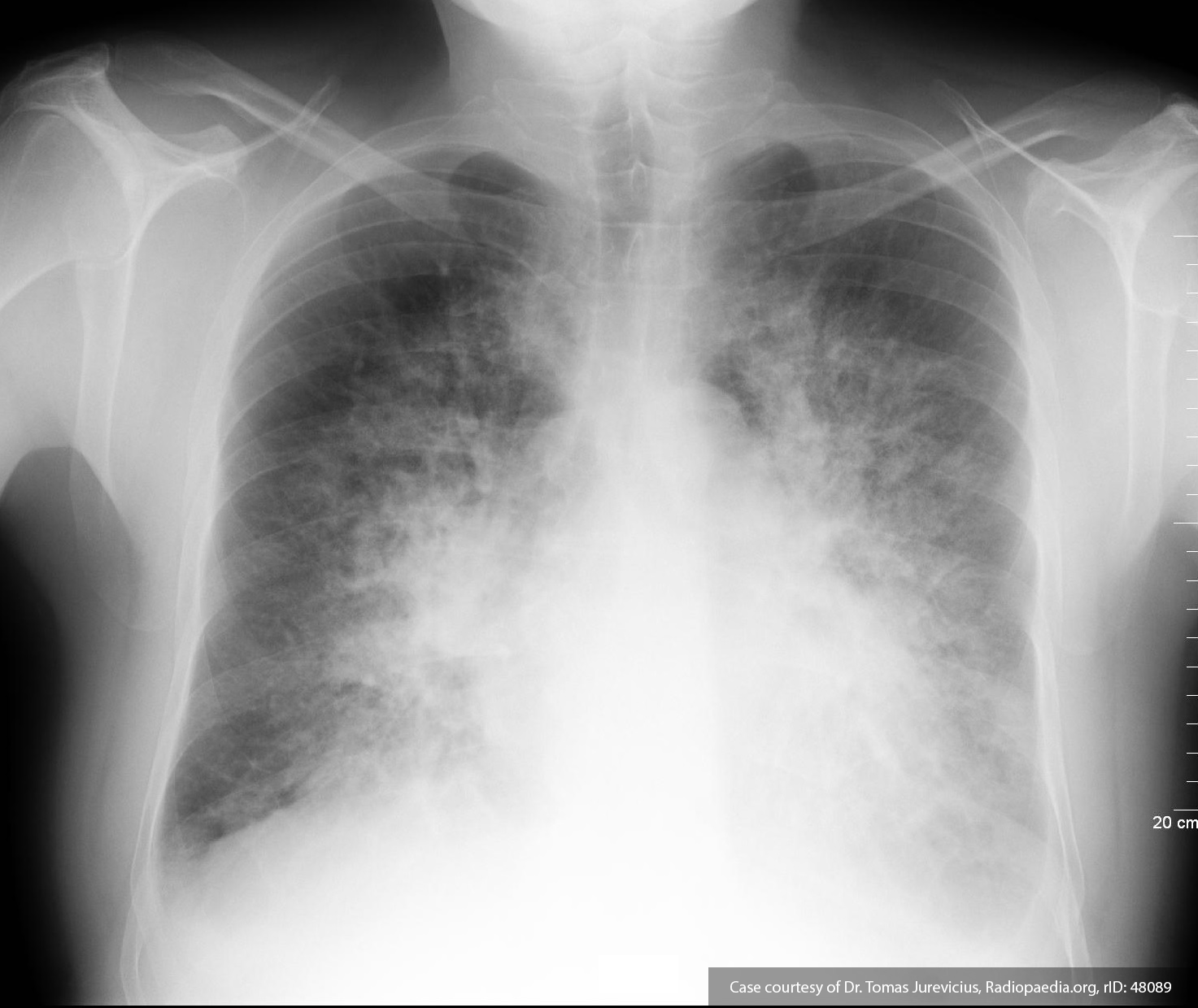
The patient was deemed to not meet any requirements for emergent hemodialysis. One unit of packed red blood cells was ordered for transfusion for symptomatic anemia. During transfusion, the patient developed worsening dyspnea and was found to be hypertensive and hypoxic. A chest radiograph was obtained and is shown below.
The transfusion was discontinued, the patient was placed on non-invasive positive pressure ventilation, and emergent hemodialysis was initiated with subsequent resolution of presumed transfusion associated circulatory overload.
Algorithm for the Evaluation and Management of Transfusion Reactions
References
- Carson JL, Triulzi DJ, Ness PM. Indications for and Adverse Effects of Red-Cell Transfusion. N Engl J Med. 2017;377(13):1261-1272. doi:10.1056/NEJMra1612789.
- Delaney M, Wendel S, Bercovitz RS, et al. Transfusion reactions: prevention, diagnosis, and treatment. Lancet. 2016;388(10061):2825-2836. doi:10.1016/S0140-6736(15)01313-6.
- Goel R, Tobian AAR, Shaz BH. Noninfectious transfusion-associated adverse events and their mitigation strategies. Blood. 2019;133(17):1831-1839. doi:10.1182/blood-2018-10-833988.
- Osterman JL, Arora S. Blood product transfusions and reactions. Emerg Med Clin North Am. 2014;32(3):727-738. doi:10.1016/j.emc.2014.04.012.
- Silvergleid AJ. Approach to the patient with a suspected acute transfusion reaction. Post TW, ed. UpToDate. Waltham, MA: UpToDate Inc. https://www.uptodate.com (Accessed on September 01, 2019.)
- Suddock JT, Crookston KP. Transfusion Reactions. January 2019.