ID:
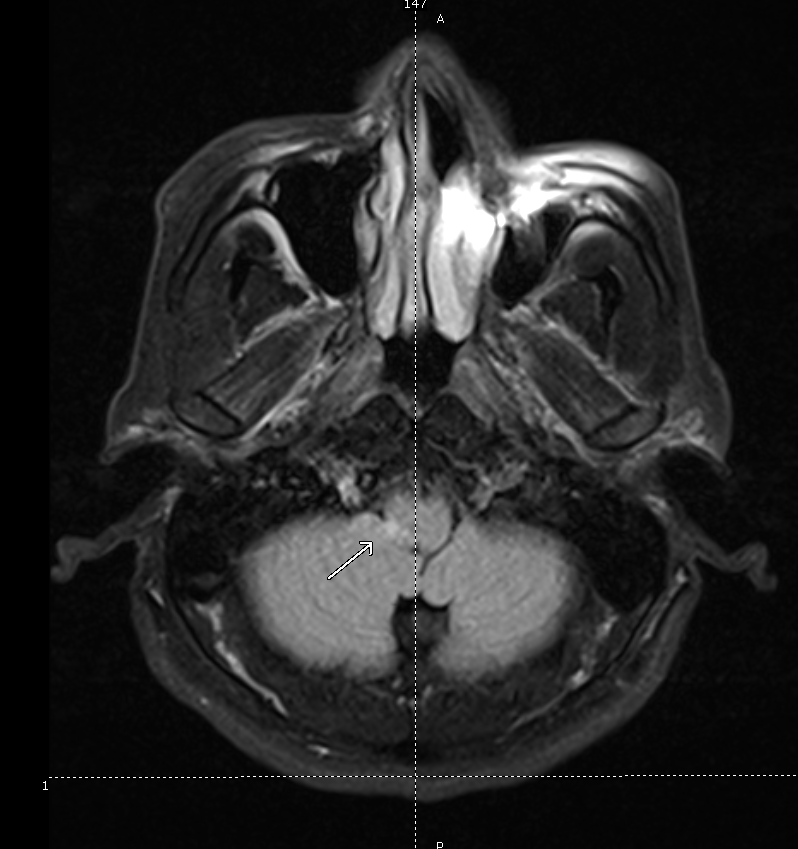
A 70 year-old female with a PMH of HTN, DM, hyperlipidemia and stage I breast cancer s/p lumpectomy with sentinel LN biopsy several years ago presented for elective surgery complicated by post-operative bleeding. She is now 4 days post-op and was found to be confused, somnolent and occasionally agitated.
HPI:
The patient could not be interviewed.
PE:
- VS: Stable and within normal limits
- General: unremarkable except for crackles in bilateral lung bases
- MSE: only arouses to sternal rub and becomes agitated, moving all four extremities spontaneously and symmetrically.
- Reflexes: corneal and gag reflexes present, suppresses eye movements with head turn, deep tendon reflexes 3+ throughout UE/LE bilaterally.
Assessment:
70 year-old woman with a history of HTN, DM, hyperlipidemia and breast cancer presents with worsening confusion, somnolence and occasional agitation four days after surgery. The combination of significantly altered consciousness and absence of focal neurological findings, all in the setting of a complicated surgical course suggest delirium.
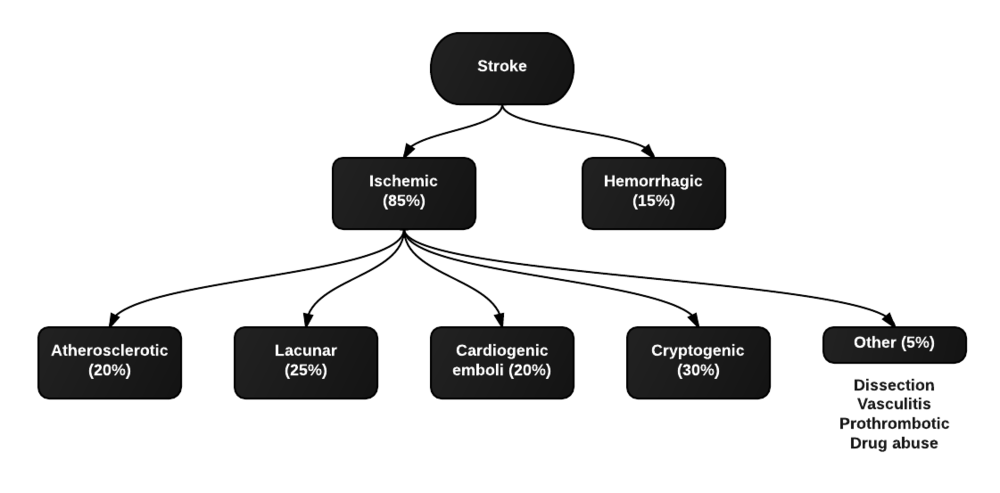
Differential Diagnosis of Altered Mental Status:
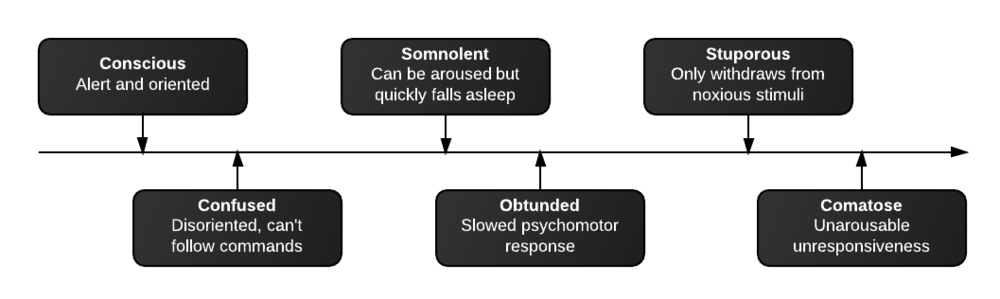
Levels of consciousness
There are different levels of consciousness, they are named in the diagram below but are better described by the characteristics observed.
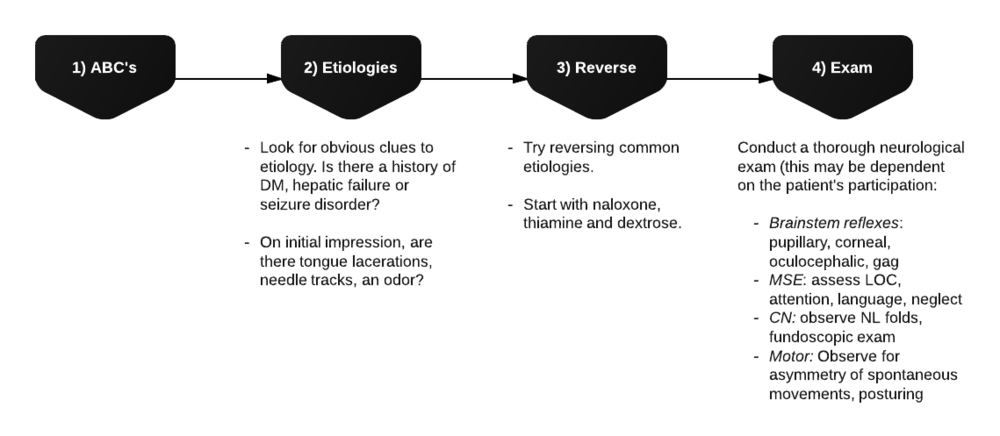
Initial assessment
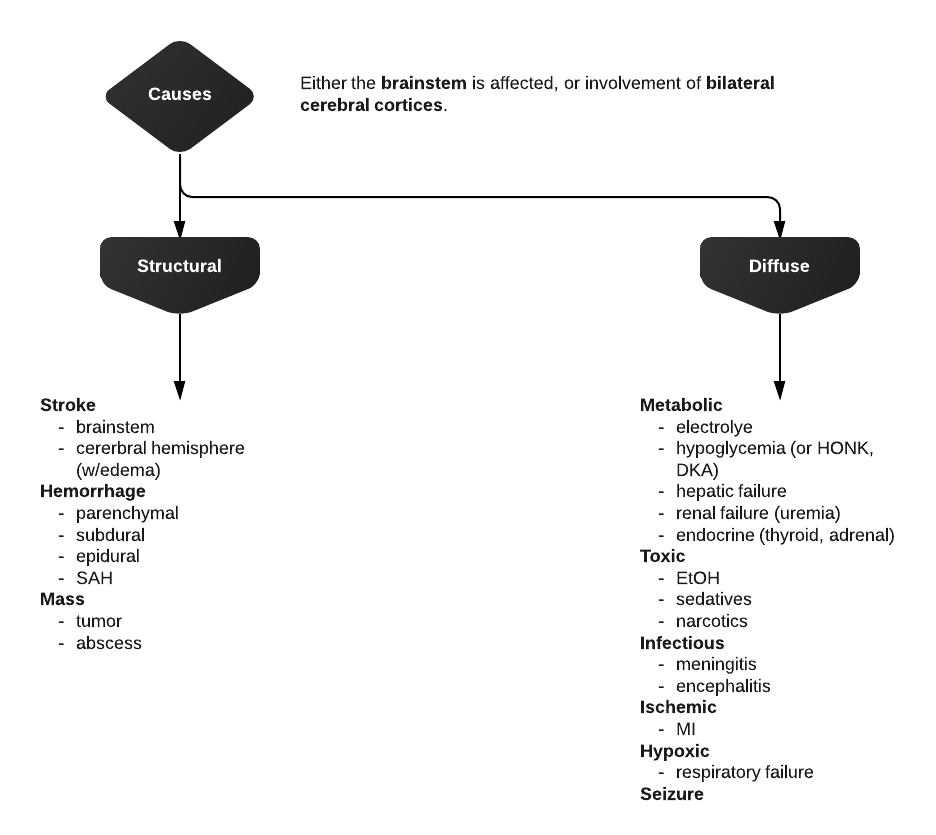
Differential Diagnosis for Altered Mental Status
References:
- Inouye, S. K. (2006). Delirium in Older Persons. The New England journal of medicine, 354(11), 1157–1165. doi:10.1056/NEJMra052321
- Blueprints neurology. Philadelphia: Wolters Kluwer Health/Lippincott William & Wilkins, 2009.
- Tindall SC. Level of Consciousness. In: Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition. Boston: Butterworths; 1990. Chapter 57. Available from: http://www.ncbi.nlm.nih.gov/books/NBK380/