Brief H&P:
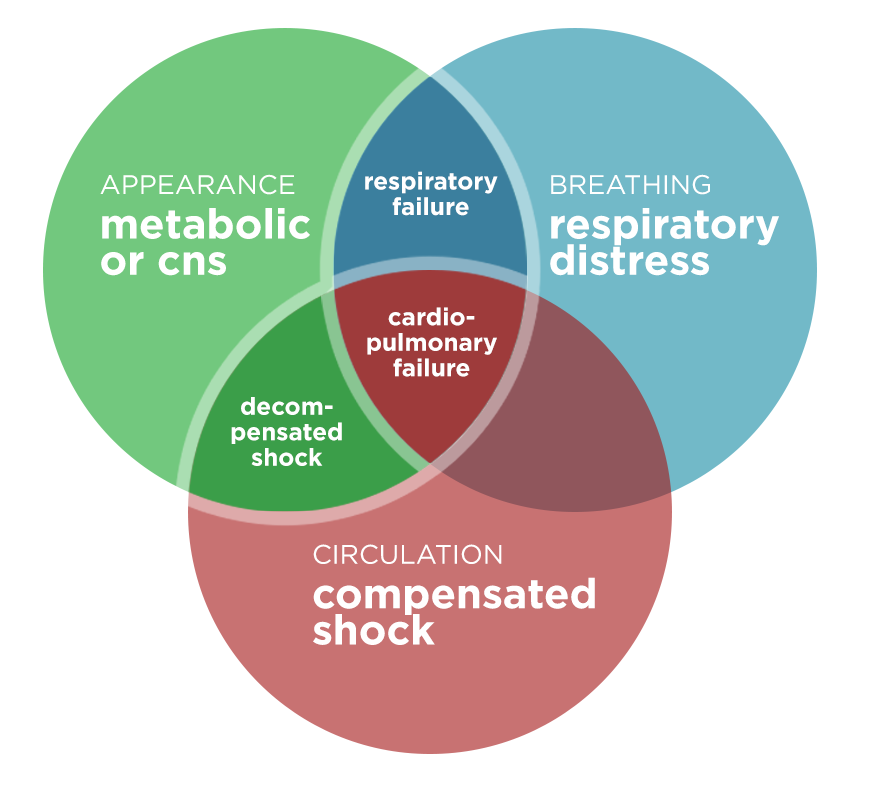
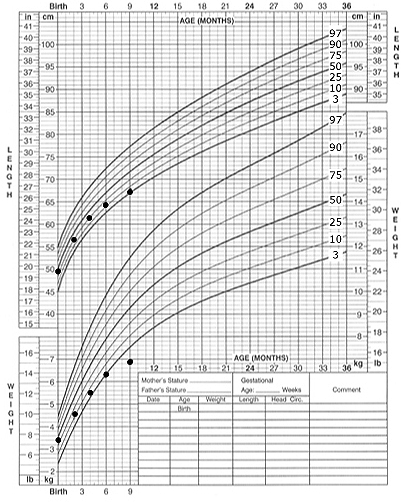
A 4 month-old male with no past medical history and fully-immunized is brought to the emergency department by her mother after an episode of breathing difficulty. She describes that just prior to presentation she noted her child had stopped breathing. She lifted him from the bed and noted some blue discoloration to the mouth with limp extremities. She began to stimulate him by rubbing his chest and abdomen and he began crying after approximately 30 seconds.
She states that he has since returned to normal and she was able to feed him upon arrival to the emergency department without apparent difficulty or vomiting. Prior to the episode, the patient had been in his usual state of health (normal oral intake, urine/stool). No family history of sudden death.
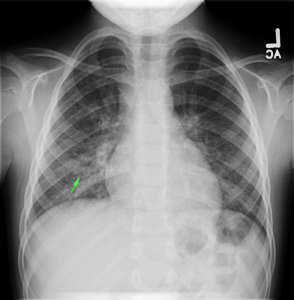
On physical examination, vital signs are normal. The child appears comfortable. Head is normocephalic and atraumatic with normal anterior fontanelle. Mucous membranes are moist, heart sounds are normal and lungs are clear. The abdomen is soft and without organomegaly. The remainder of a detailed physical examination is unremarkable.
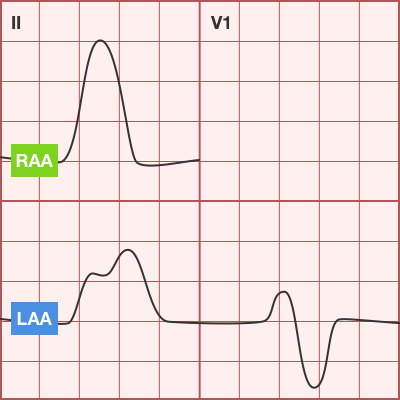
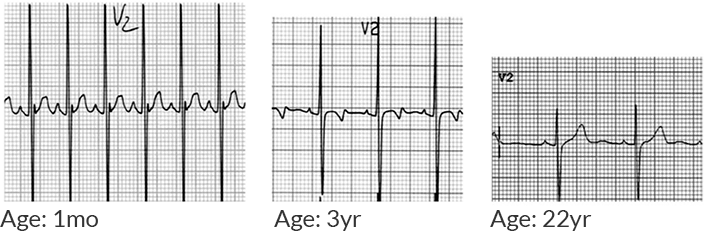
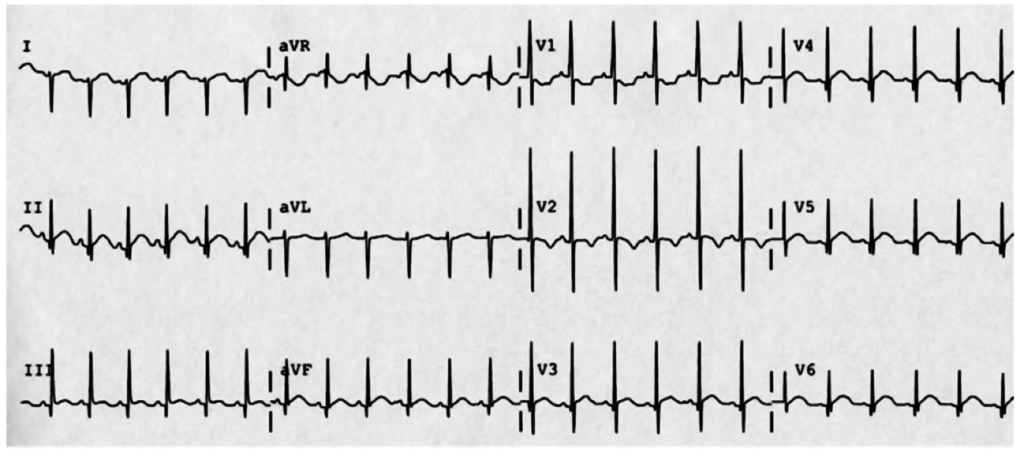
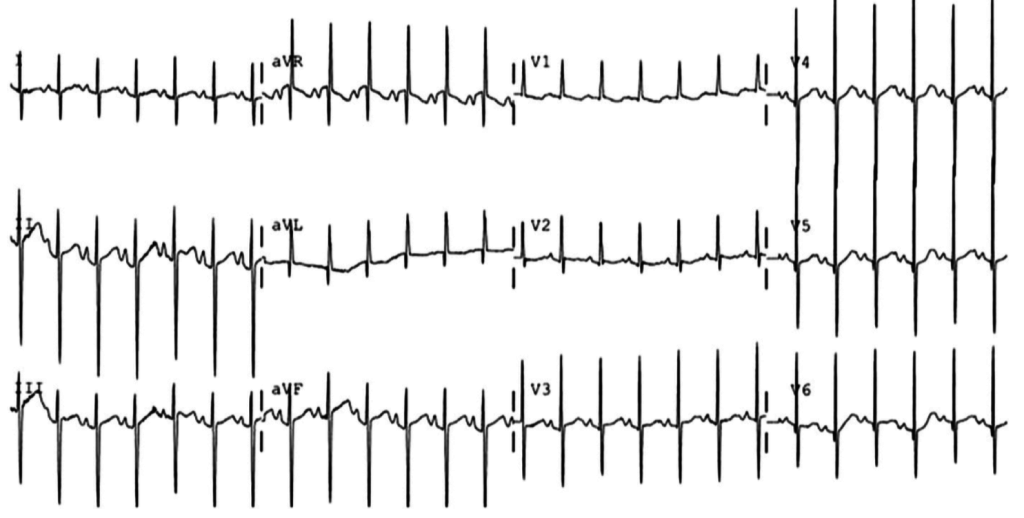
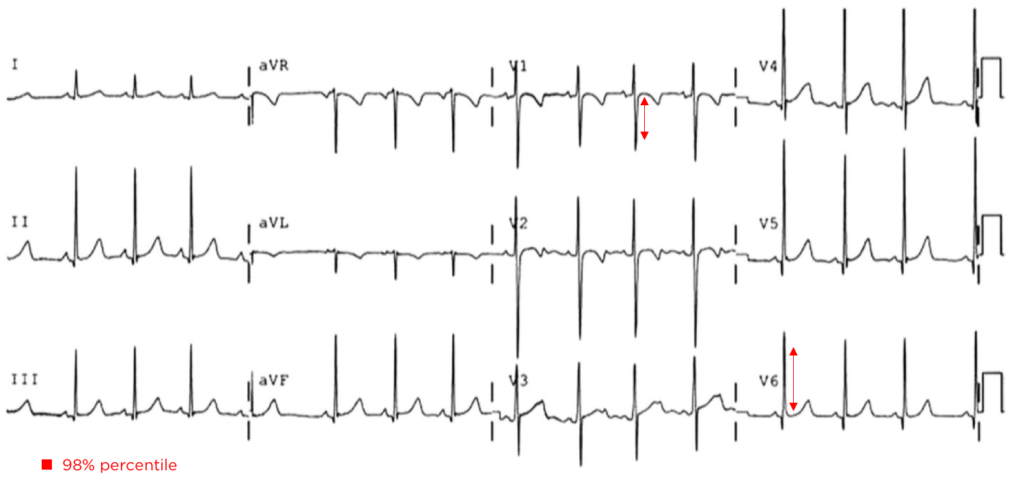
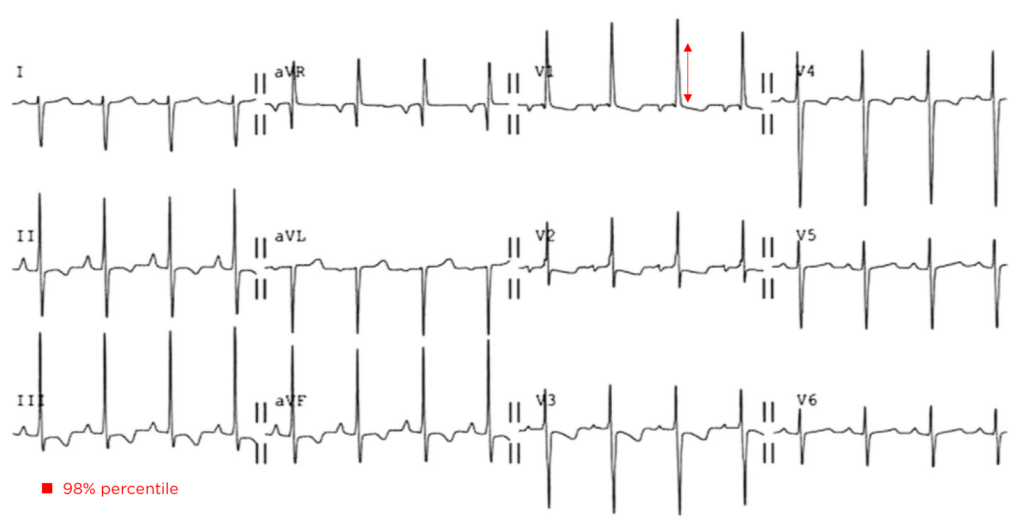
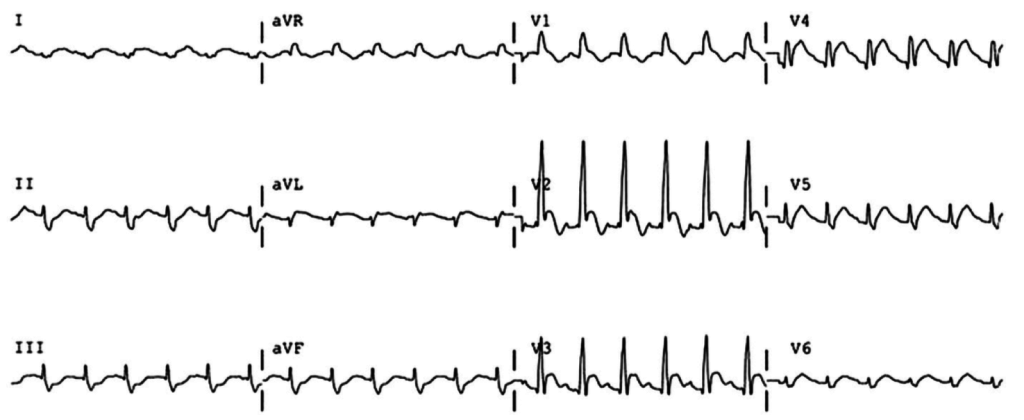
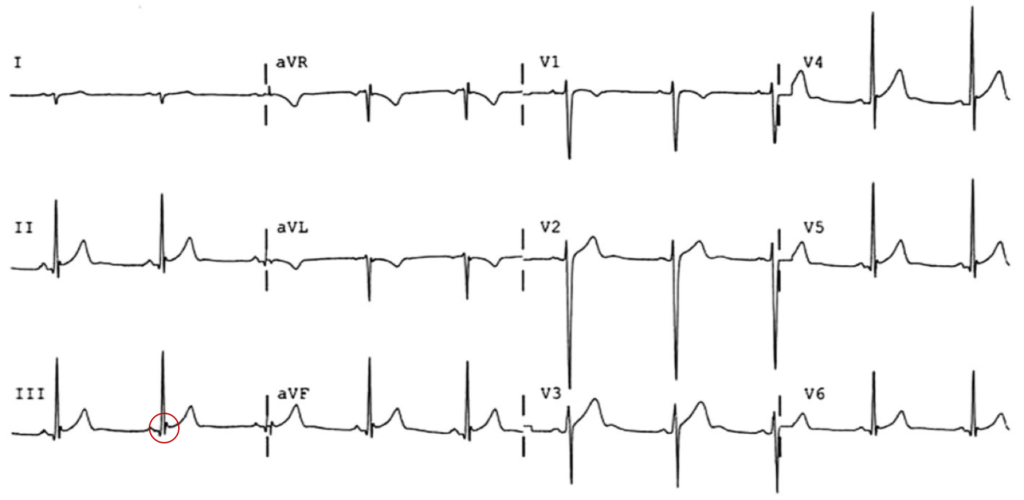
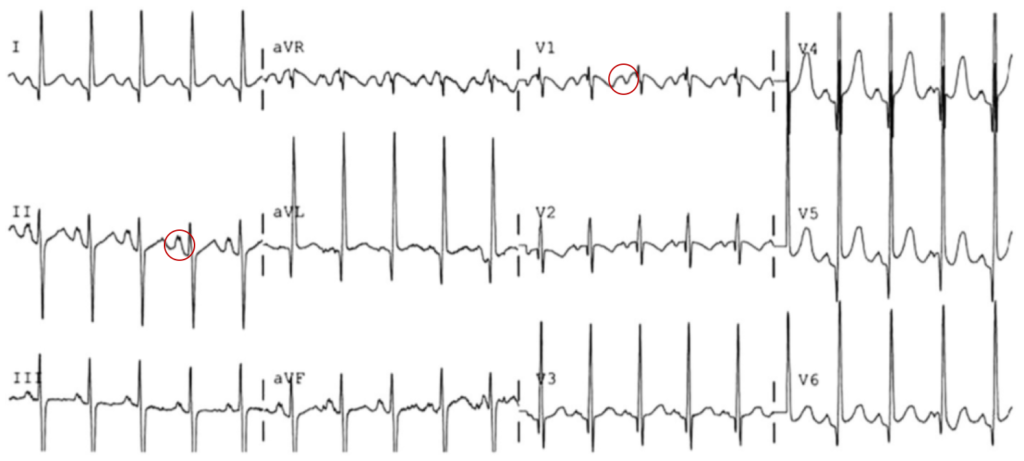
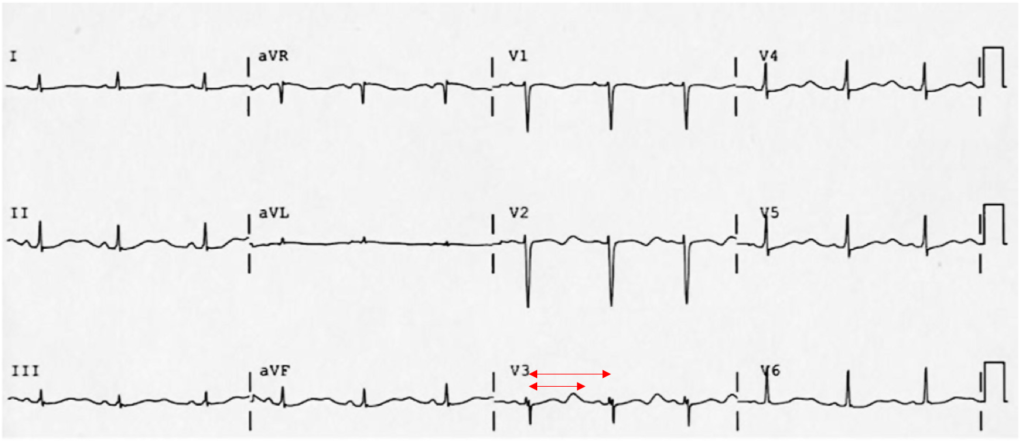
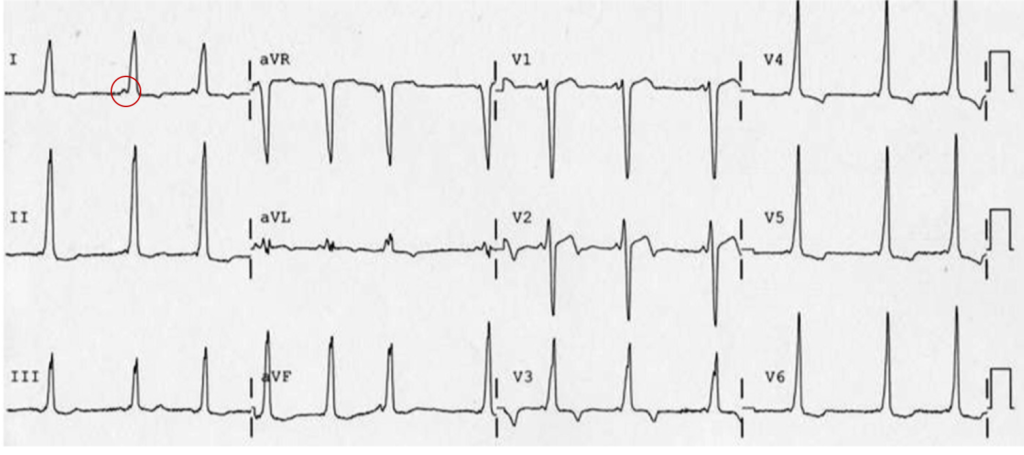
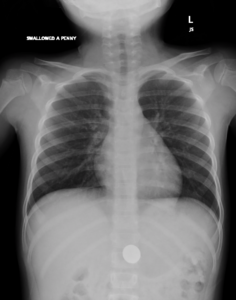
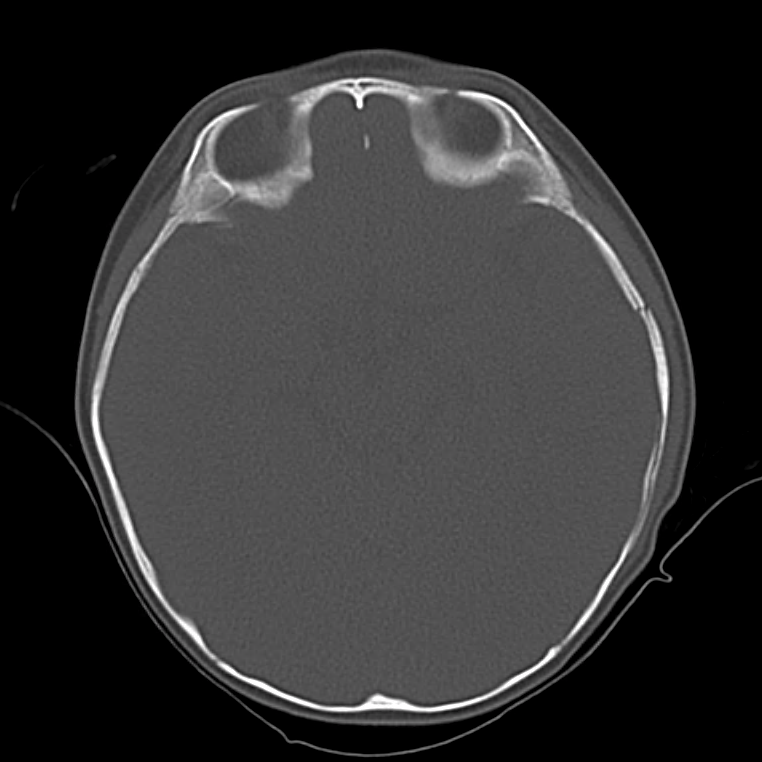
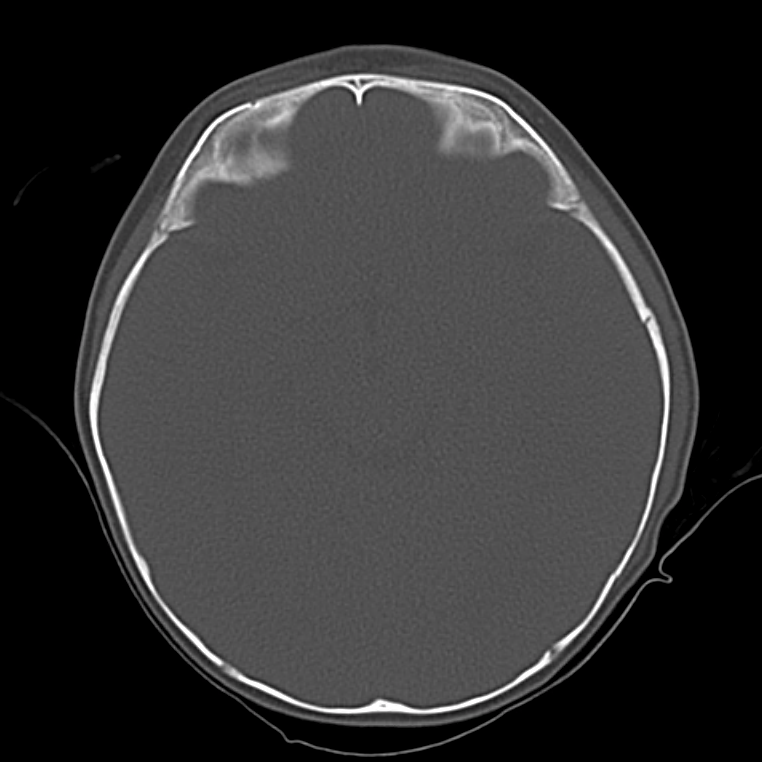
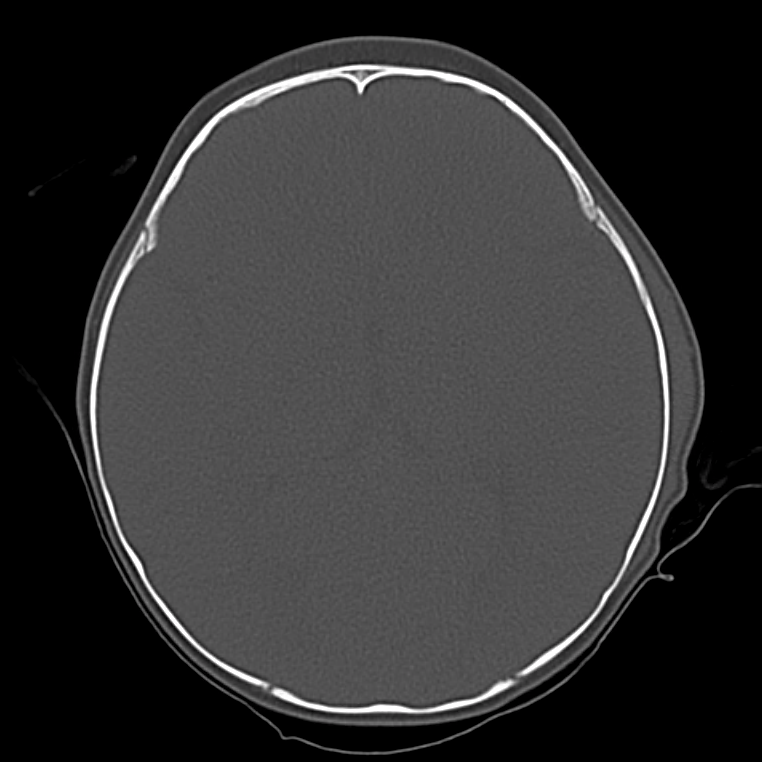
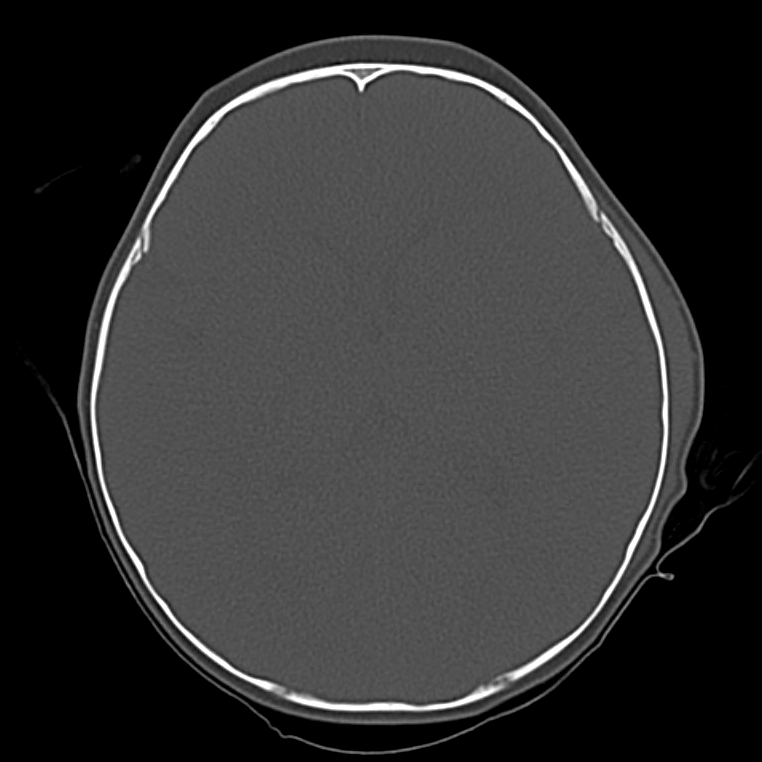
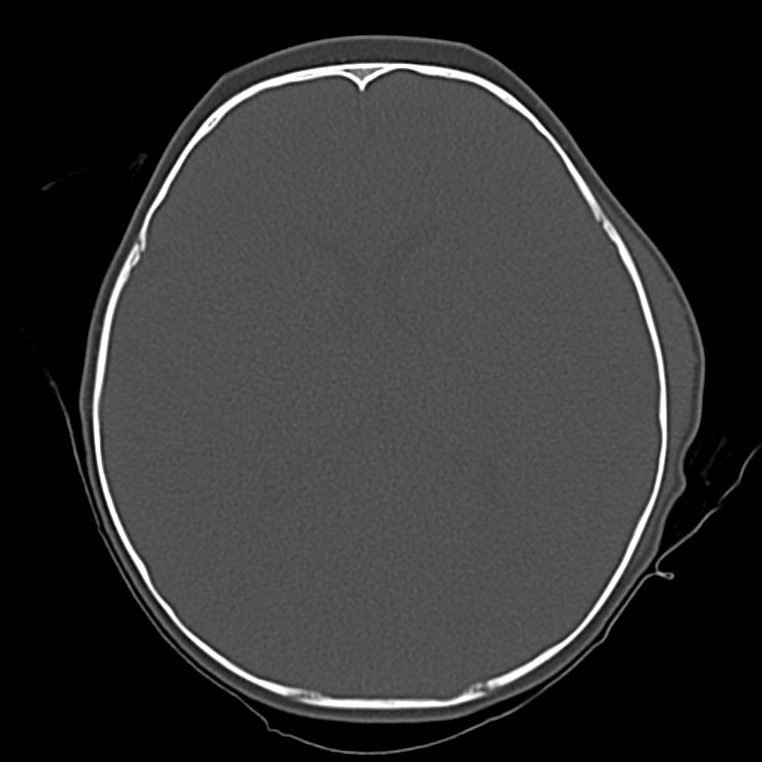
The patient was placed on continuous pulse oximetry, remained well-appearing on serial reassessments and had no further episodes while continuing to feed normally. An ECG was obtained:
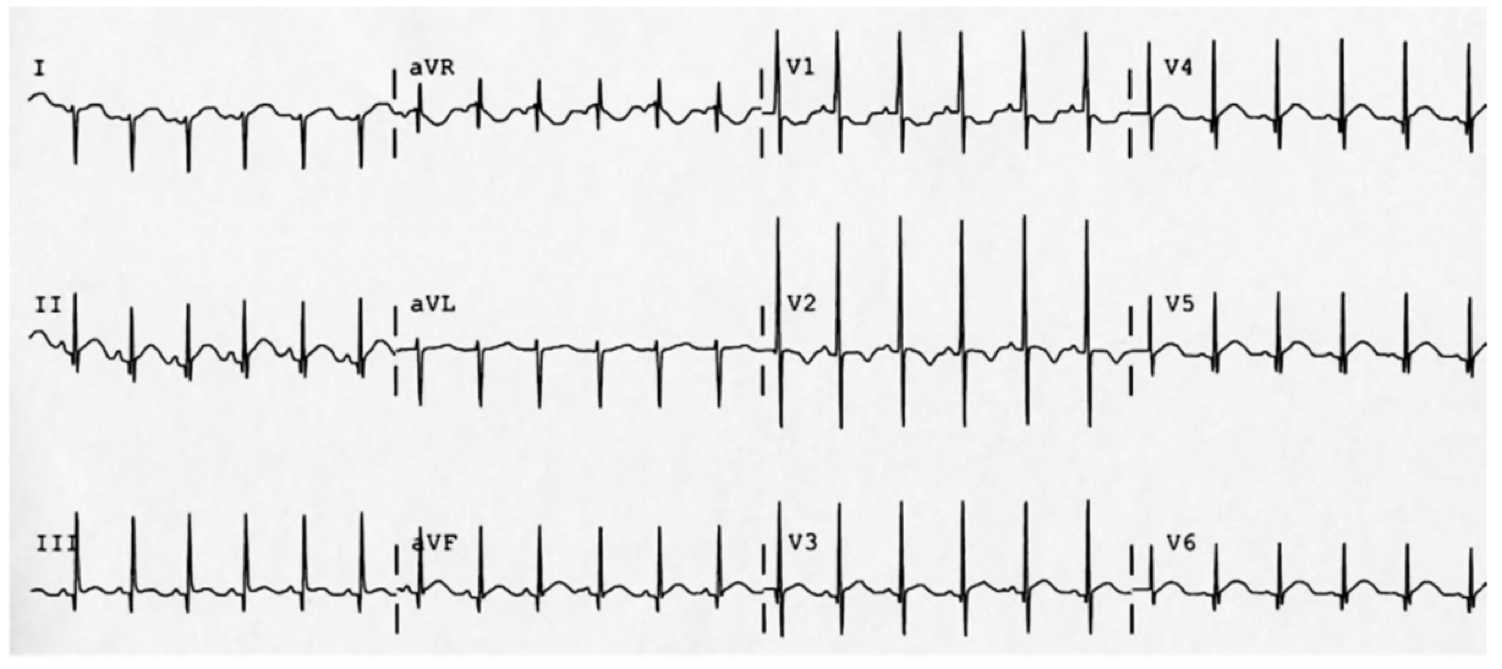
The patient’s mother was counseled regarding the diagnosis of low-risk BRUE and the reassuring evaluation and ED observation period. She states that she is able to present to her pediatrician the subsequent morning for evaluation. She was counseled regarding return precautions prior to discharge.
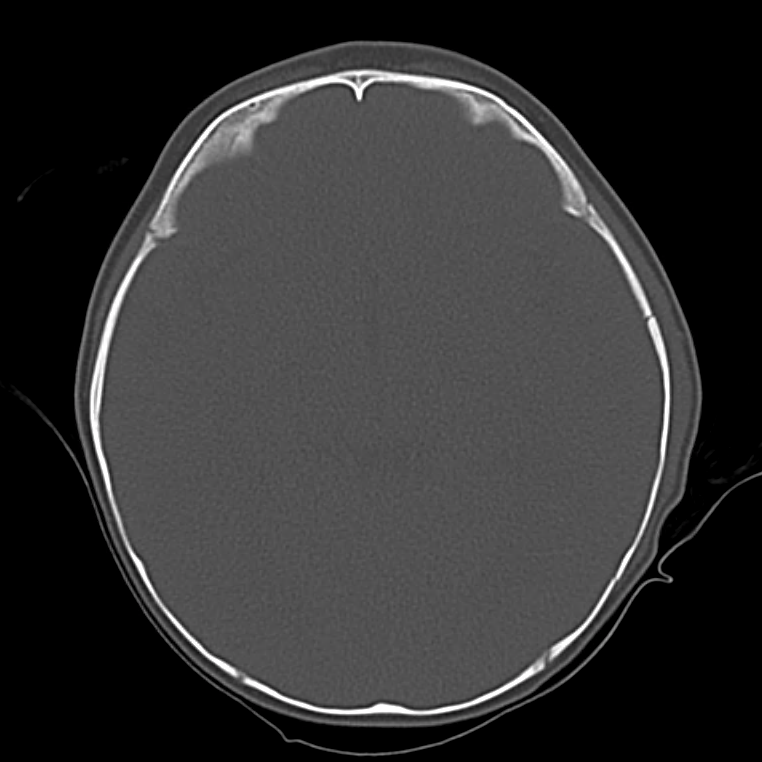
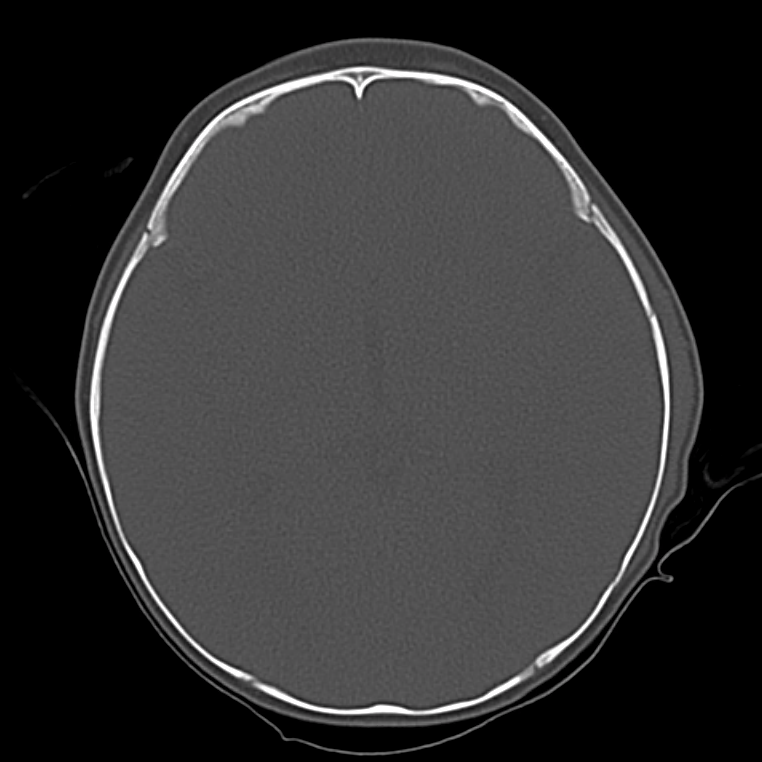
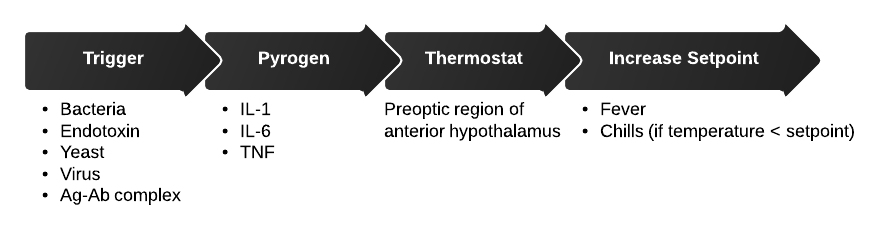
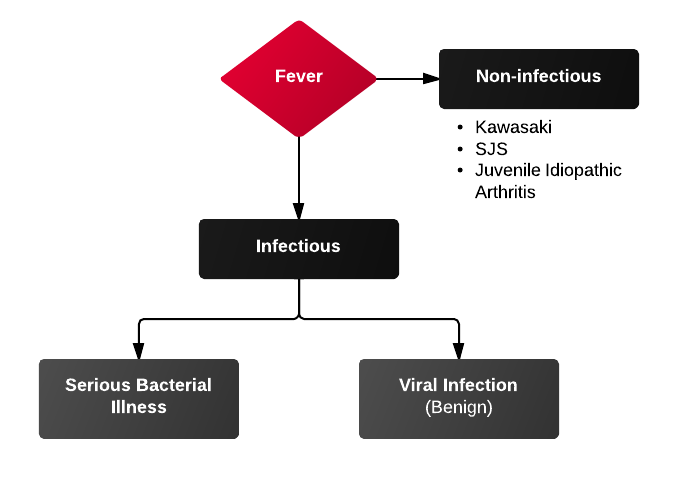
An Algorithm for the Evaluation and Management of Brief Resolved Unexplained Events (BRUE)1,2
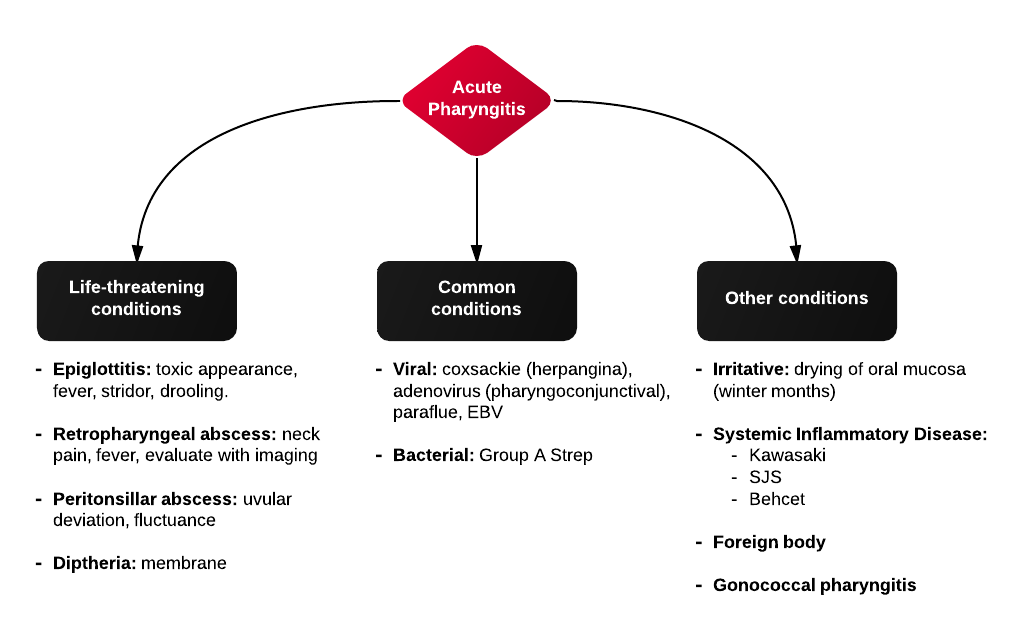
Differential Diagnosis for BRUE3
| Category | Causes |
|---|---|
| Environmental | Abuse/trauma Toxicological |
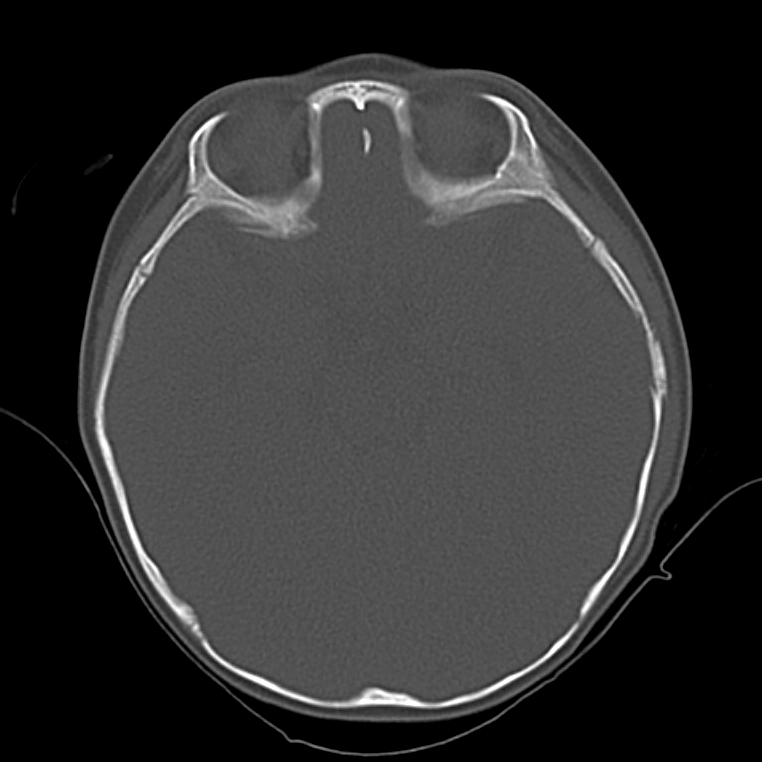
| CNS | Seizure Intracranial mass |
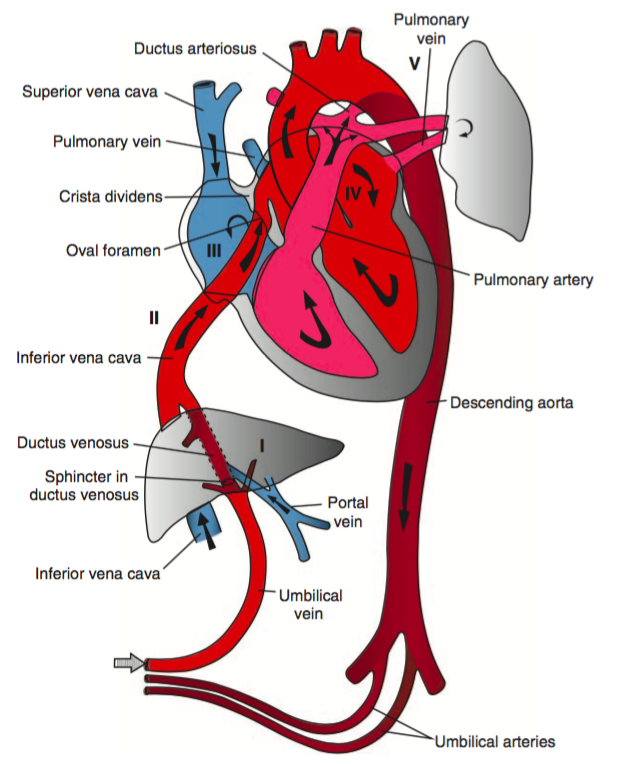
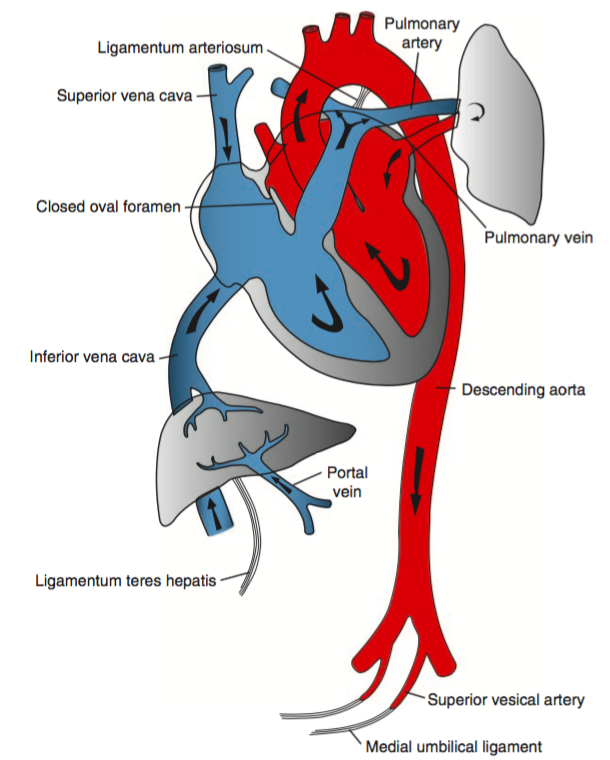
| Cardiovascular | Congenital heart disease Arrhythmia |
| Pulmonary | Airway obstruction Central apnea Apnea of prematurity Pneumonia Bronchiolitis Pertussis |
| Gastrointestinal | GERD |
| IEM | Glycogen storage disease Hyperinsulinism Fatty acid oxidation defects |
Special thanks to Dr. Thomas McCarty, Assistant Professor and Pediatric Emergency Medicine Fellowship Director in the Department of Emergency Medicine at McGovern Med EM for his review of the algorithm.
References:
- Tieder JS, Bonkowsky JL, Etzel RA, et al. Clinical Practice Guideline: Brief Resolved Unexplained Events (Formerly Apparent Life-Threatening Events) and Evaluation of Lower-Risk Infants: Executive Summary. Pediatrics. 2016:137(5):e20160591.
- Merritt JL, Quinonez RA, Bonkowsky JL, et al. A framework for evaluation of the higher-risk infant after a brief resolved unexplained event. Pediatrics. 2019;144(2):e20184101.
- McGovern MC, Smith MBH. Causes of apparent life threatening events in infants: a systematic review. Arch Dis Child. 2004;89(11):1043-1048.