Brief HPI
A 45 year-old female with a history of pre-diabetes and gastroesophageal reflux disease presents with 3 days of epigastric abdominal pain. She describes constant, burning abdominal pain which worsened on the day of presentation associated with two episodes of non-bloody and non-bilious emesis. The patient was tender to palpation in the epigastrium and right upper quadrant.
Laboratory studies were largely normal. A complete blood count demonstrated minimal leukocytosis (11.6 with normal differential), and liver function tests were normal.
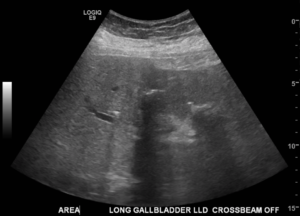
A right-upper quadrant ultrasound was obtained which demonstrated “strongly shadowing structures in the gallbladder fossa which might represent a wall-echo-shadow, calcified gallbladder wall, or air within the gallbladder”.
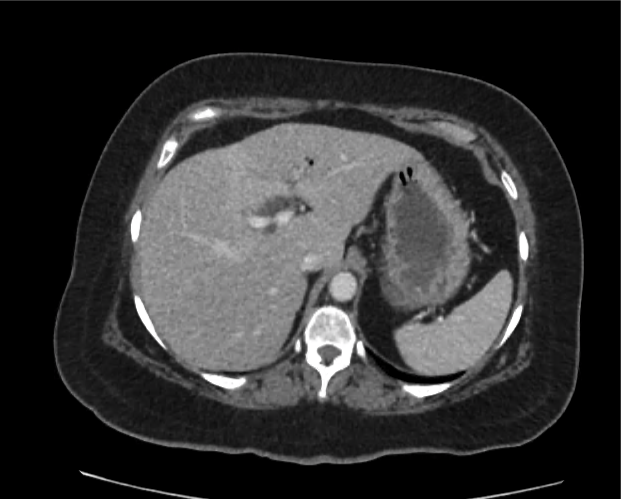
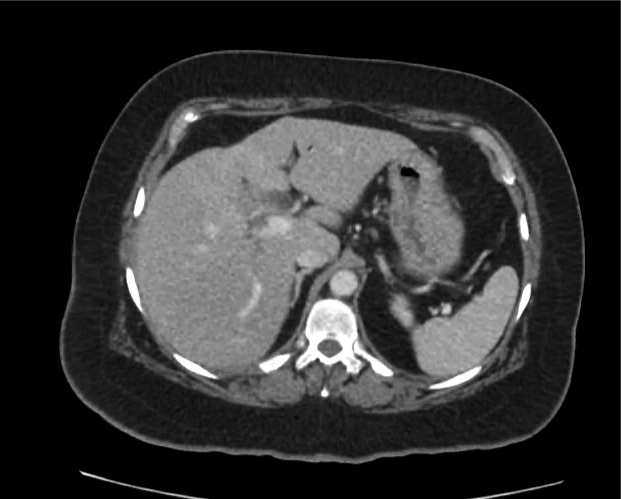
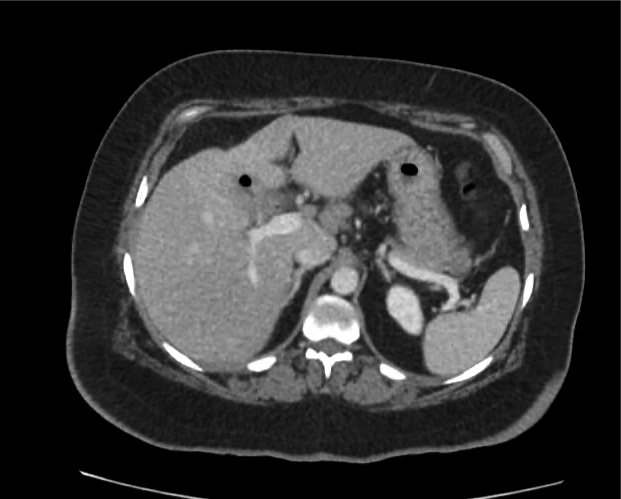
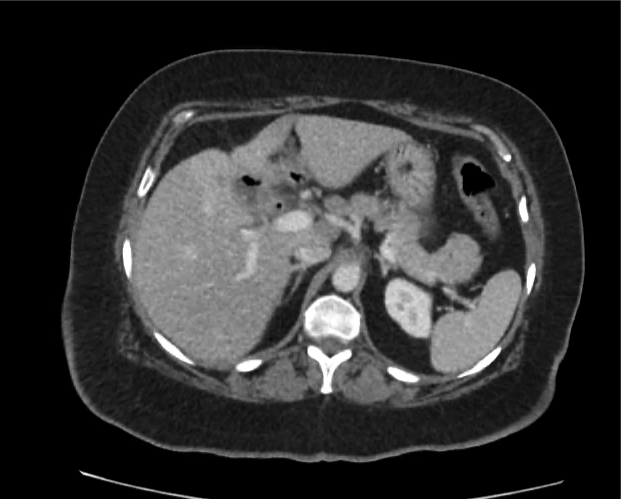
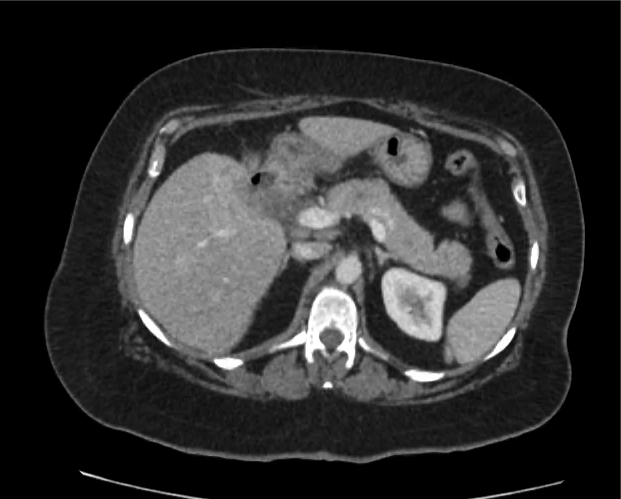
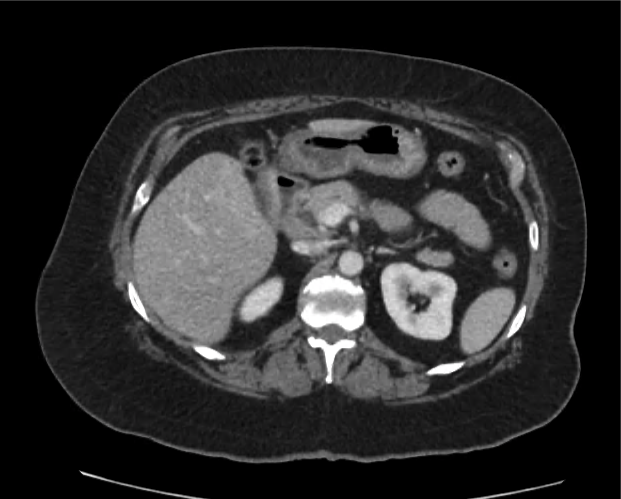
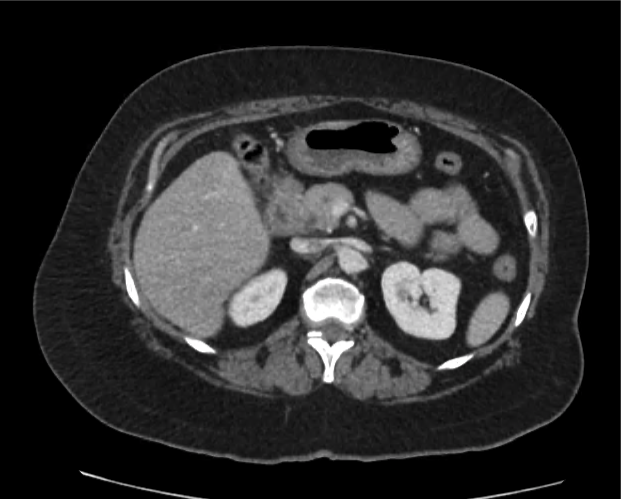
The patient underwent contrast-enhanced computed tomography of the abdomen and pelvis which is shown below.
Imaging
CT Abdomen/Pelvis with Contrast
Pneumobilia, intra- and extra-hepatic biliary duct dilation, pericholecystic fat stranding, and an air-fluid level within a contracted gallbladder. Mildly dilated loops of ileal bowel with a possible transition point in the right lower quadrant. Findings suggestive of possible gallstone ileus.
The patient was taken to the operating room for exploratory laparotomy, possible cholecystectomy and possible small bowel resection for presumed gallstone ileus. Intra-operative findings were notable for a cholecystogastric fistula which was repaired.
Differentiation between Portal Venous Gas and Pneumobilia
The patient’s CT demonstrated mostly central hepatic gas. This finding combined with the presence of an air-fluid level in the gallbladder was most consistent with pneumobilia. This case demonstrates an application of the previously-developed algorithm for the evaluation of hepatic gas in a relatively unique pathologic process.