 CC:
CC:
Consultation for bowel obstruction
HPI:
The patient is a 40yo male with a history of alcohol abuse, and seizure disorder secondary to traumatic brain injury who was admitted to this hospital 4d ago after an altercation with law enforcement officials. On arrival, the patient was reported to be acutely intoxicated with ecchymosis and bleeding from left lateral/posterior head and ear. No other significant injuries were found and the patient underwent CT imaging of head and c-spine, with notable findings of left occipital epidural hematoma, subarachnoid hemorrhage, but no significant midline shift. Neurosurgery was consulted and no emergent surgical intervention was required, the patient underwent serial imaging to monitor the bleed which was found to be stable and the patient slowly returned to baseline mental status.
On HOD4, the patient developed nausea/vomiting and abdominal pain, a nasogastric tube was placed with feculent output. CT abdomen/pelvis showed high grade SBO and possible mesenteric ischemia/infarct, and general surgery was consulted for further evaluation. The patient reported experiencing some abdominal pain since the altercation, but could not recall if he was hit in the abdomen.
PMH:
- Alcohol abuse
- Seizure disorder
PSH:
- Tibia fracture
- No prior abdominal surgery
FH:
SHx:
- Current alcohol, marijuana use, no tobacco use
- History of homelessness
Medications:
- Norco PRN
- Ativan PRN
- LISS, SQH, Thiamine
- NKDA
Physical Exam:
- VS: T 99.5°F HR 108 RR 16 BP 128/82 O2 99% RA
- Gen: NAD
- HEENT: PERRL, EOMI, sclera clear, anicteric
- CV: RRR, normal S1/S2
- Lungs: CTAB
- Abd: Distended, diffuse tenderness to palpation, no rebound tenderness, no ecchymoses or signs of trauma
- Ext: Warm, well-perfused
- Neuro: AAOx4, appropriate
Assessment/Plan:
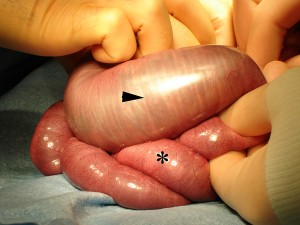
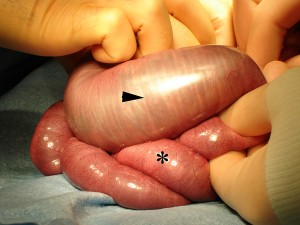
40M w/hx alcohol abuse, TBI and seizure disorder, presented initially with evidence of head trauma which was stabilized. However, the development of abdominal pain, N/V, and finding of distension on exam associated with copious output of feculent material from NGT suggests bowel obstruction. This patient has no history of abdominal surgeries to suggest adhesions as a possible cause. Though the patient cannot recall any abdominal trauma, and there was no e/o trauma on exam, findings on CT abdomen/pelvis are suggestive of traumatic cause (hematoma causing obstruction or ischemia resulting from mesenteric injury). The patient was monitored for several days, continuing NGT to suction and with serial abdominal films. However, abdominal pain persisted, abdominal radiographs showed worsening obstruction and the patient developed leukocytosis and on HOD7 the patient was taken to the OR for exploratory laparotomy. Upon entering the peritoneal cavity, there was obvious blood and very distended small bowel which was run distally with finding of a mesenteric laceration in the distal ileum which was walled off by omentum. Additionally, a grade 2 splenic laceration was found. Ultimately, a small bowel resection with primary anastomosis along with a repair of the splenic laceration was performed.
Imaging:
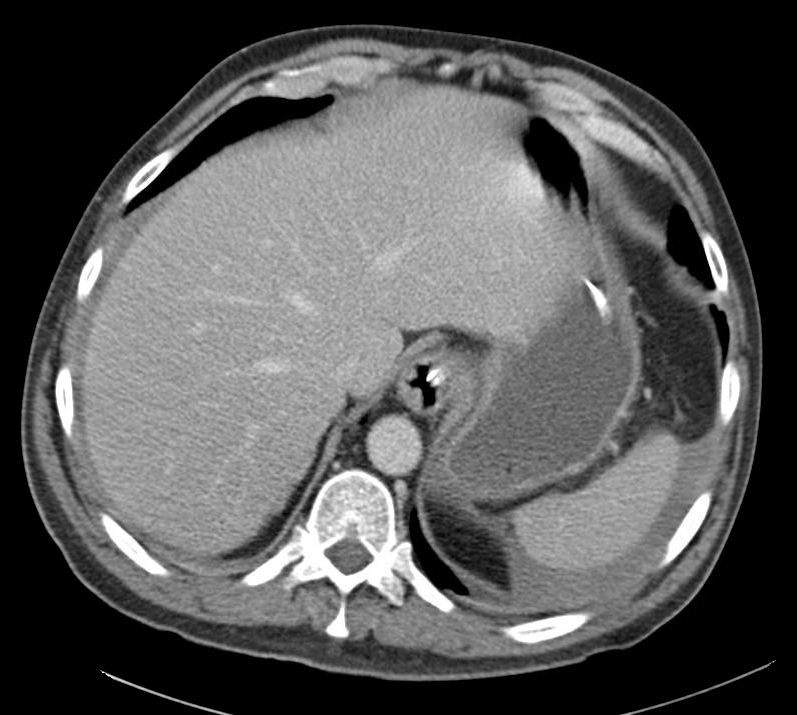
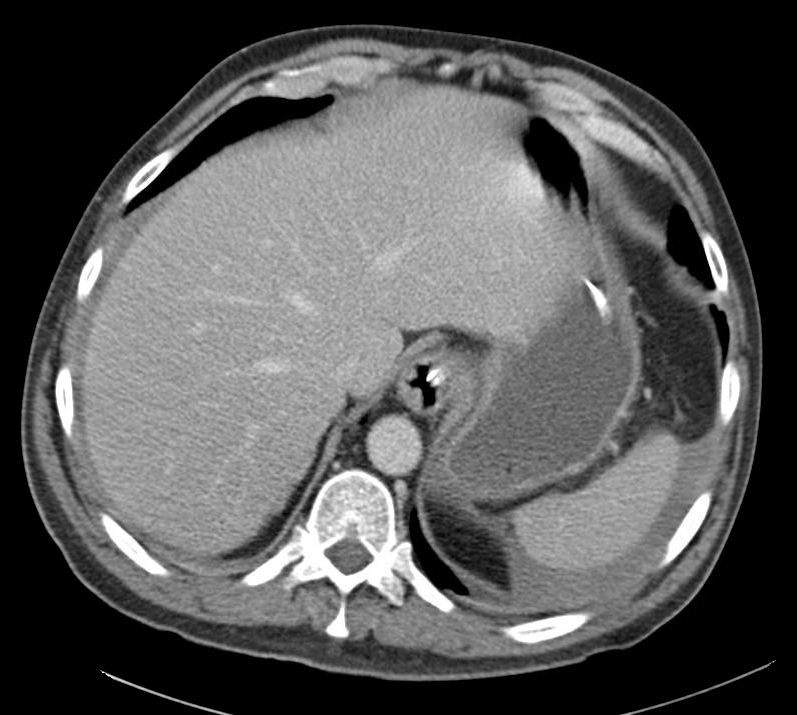
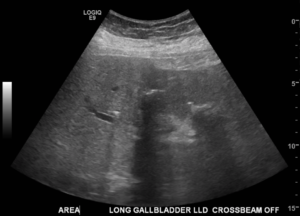
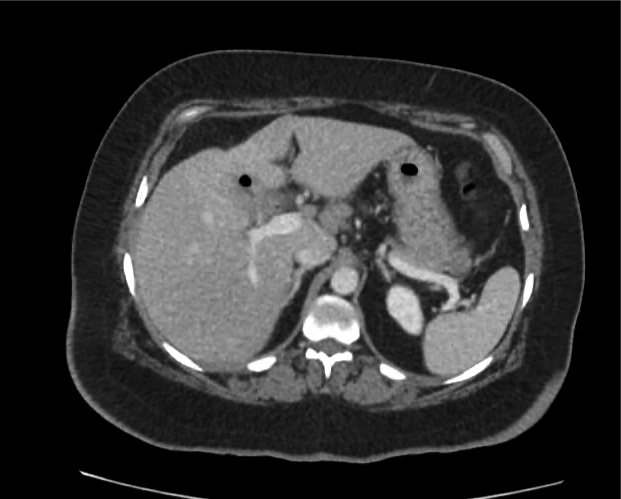
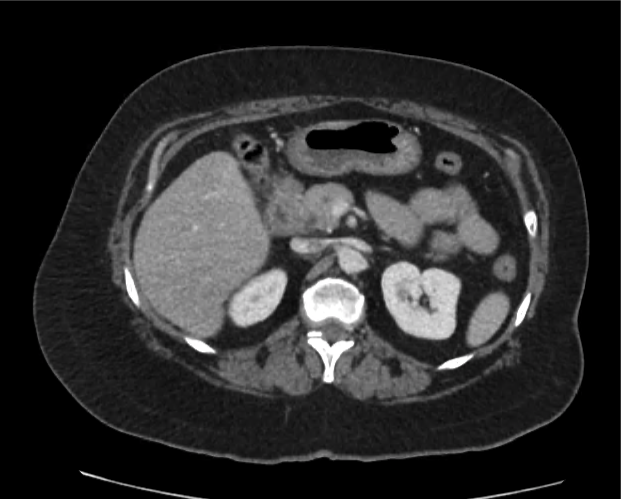
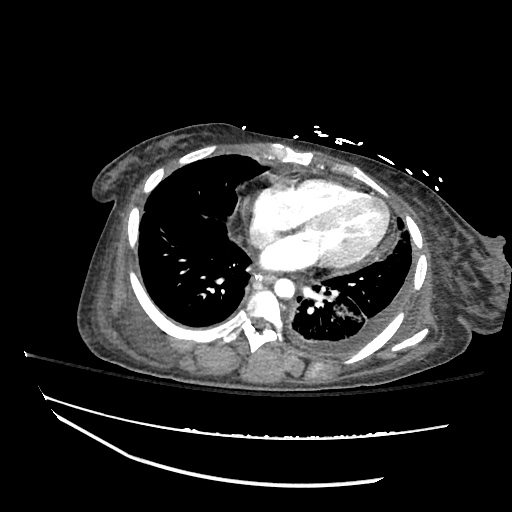
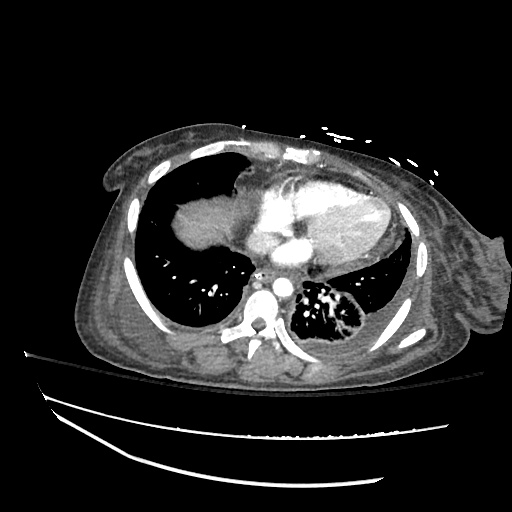
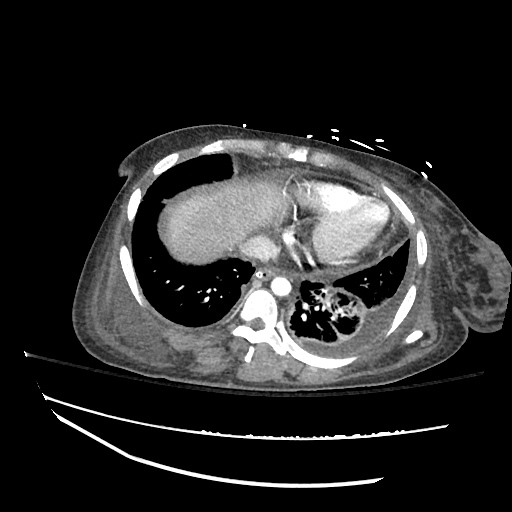
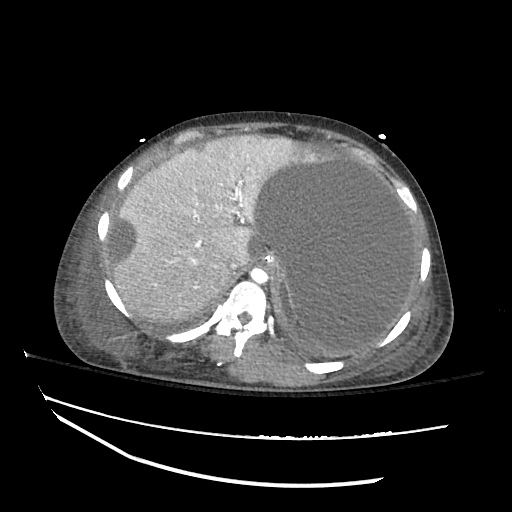
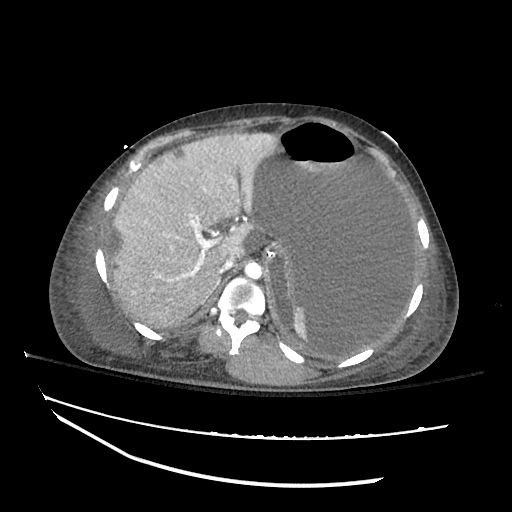
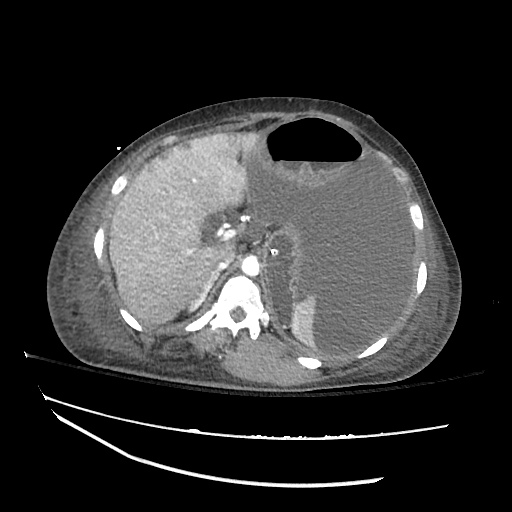
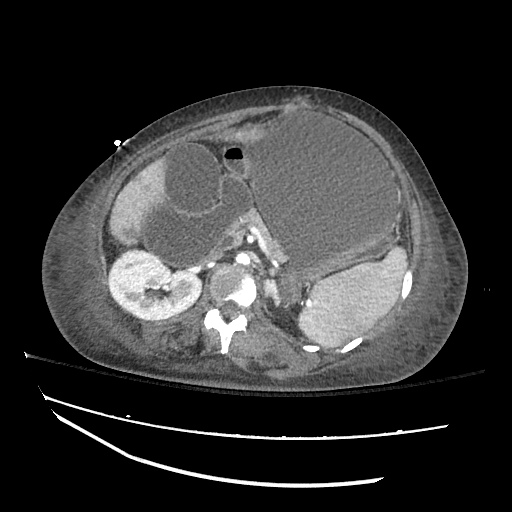
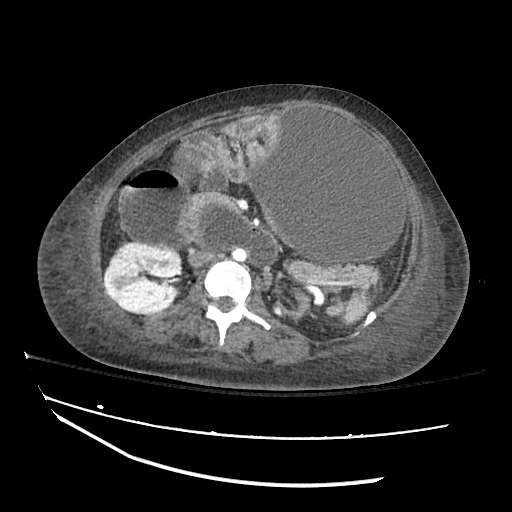
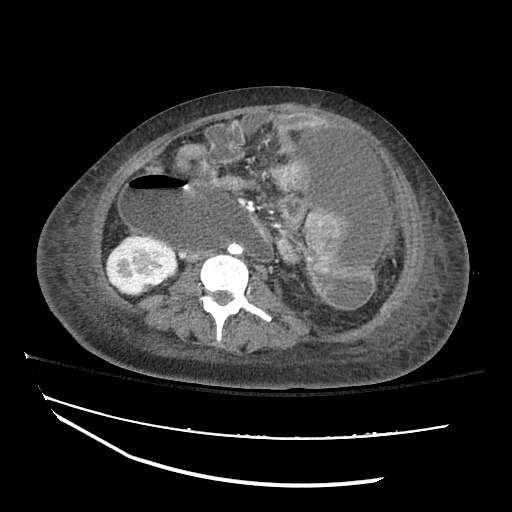
CT abdomen/pelvis
Moderate abdominal and pelvic ascites which has Hounsfield unit attenuation is greater than simple fluid suggestive of blood products.
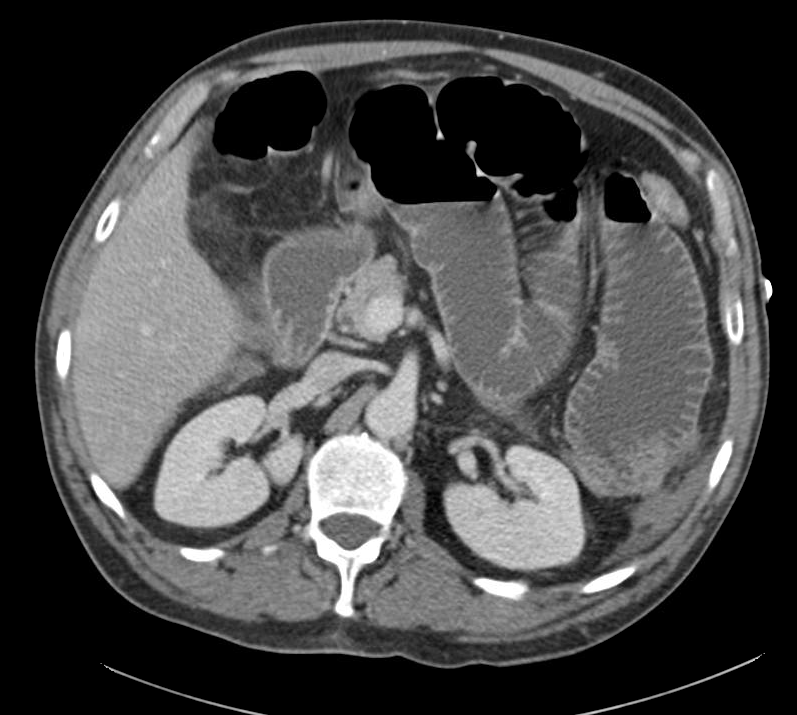
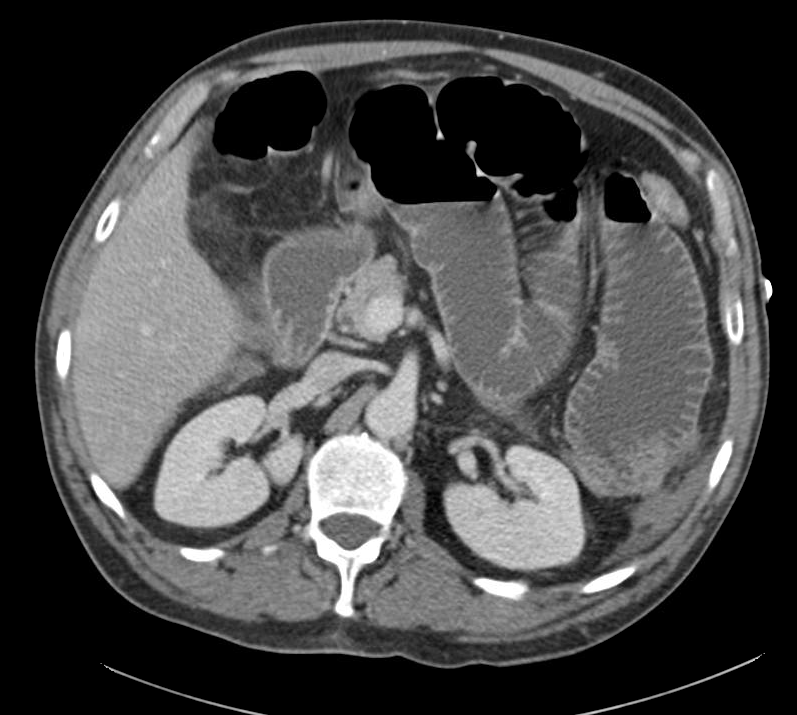
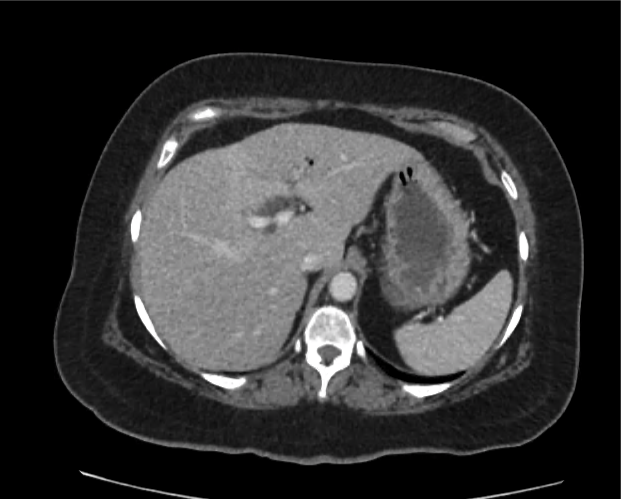
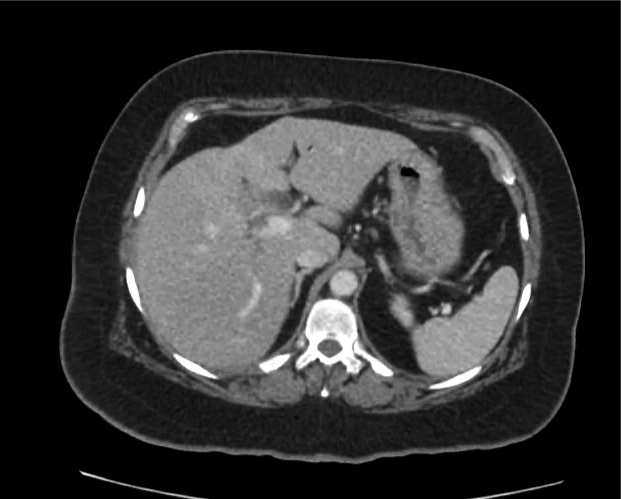
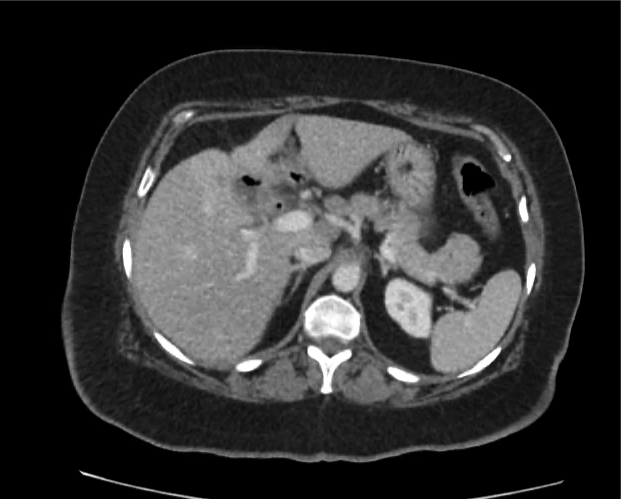
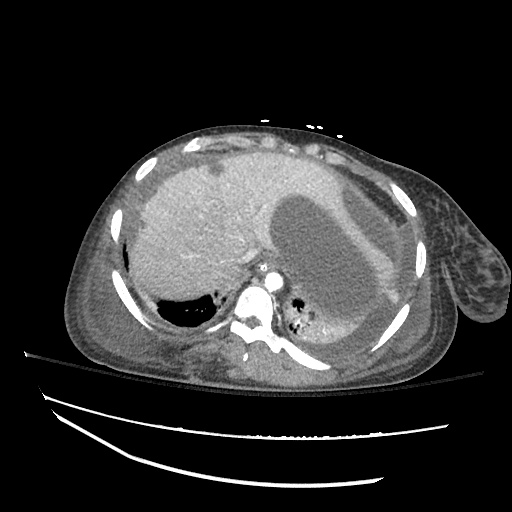
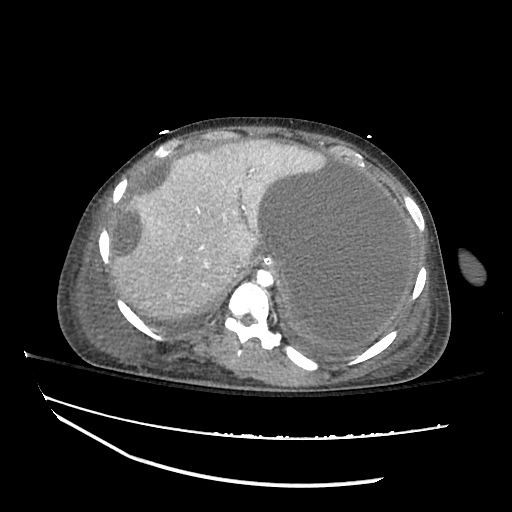
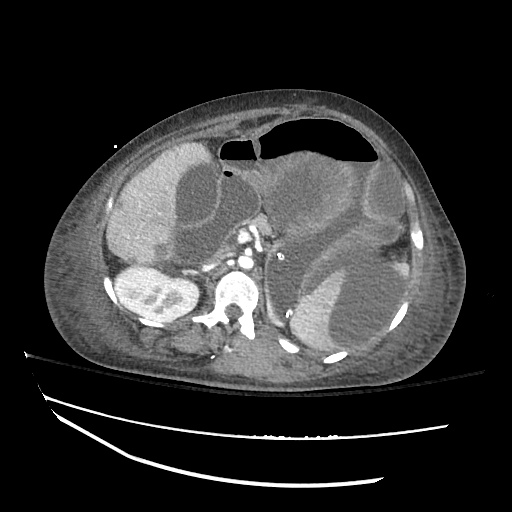
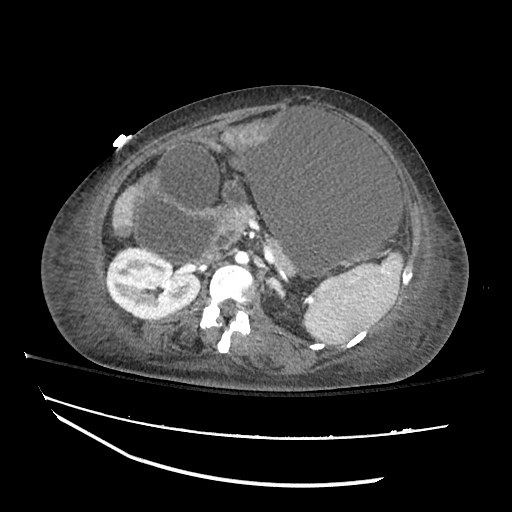
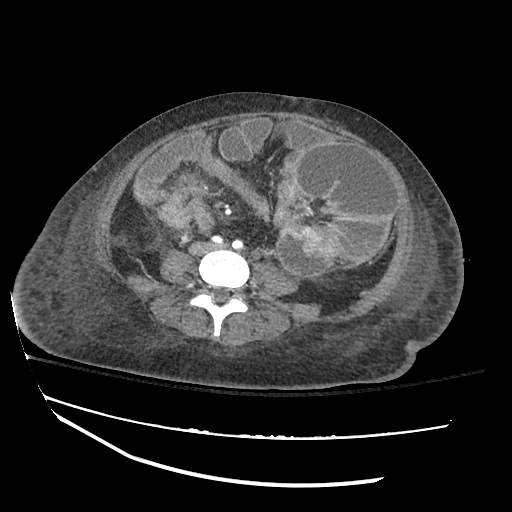
CT abdomen/pelvis
Fluid dilated small bowel

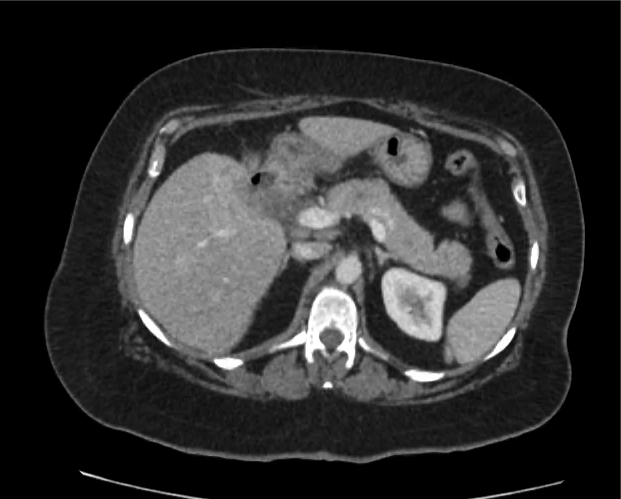
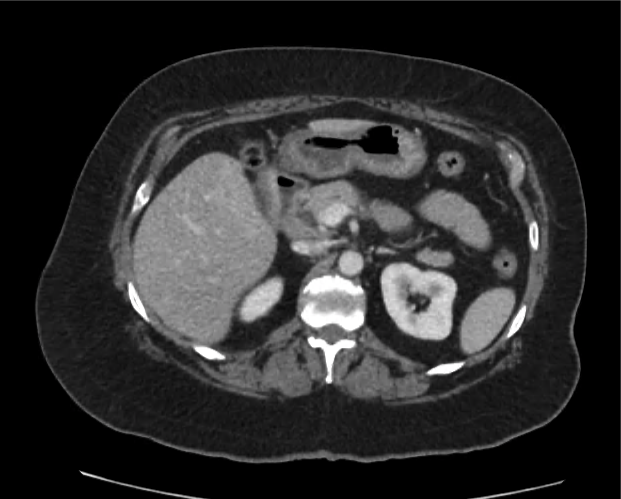
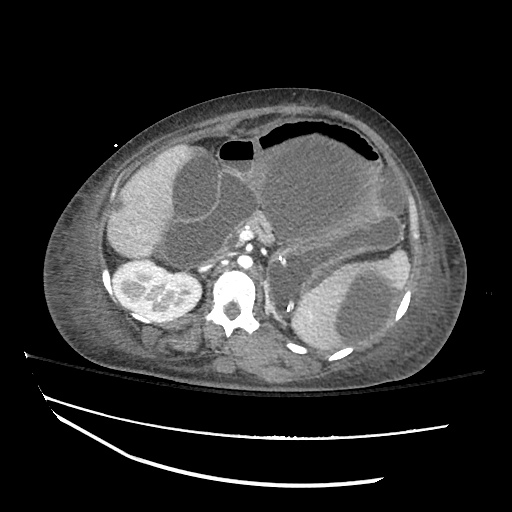
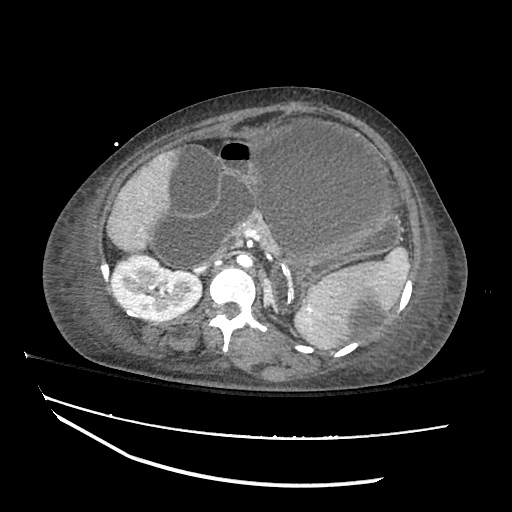
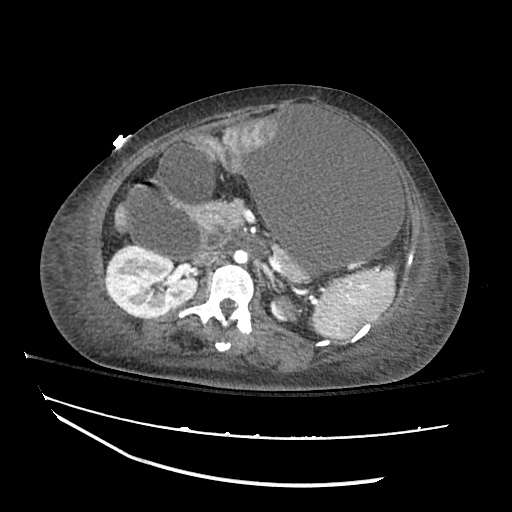
CT abdomen/pelvis
Complex transition point in the central mid abdomen.
Segment of bowel at the transition point has circumferential mural thickening and surrounding complex attenuation mesenteric fluid and mesenteric stranding.

Abdominal X-Ray
Small bowel distention
Nasogastric tube is seen coiled in the gastric fundus
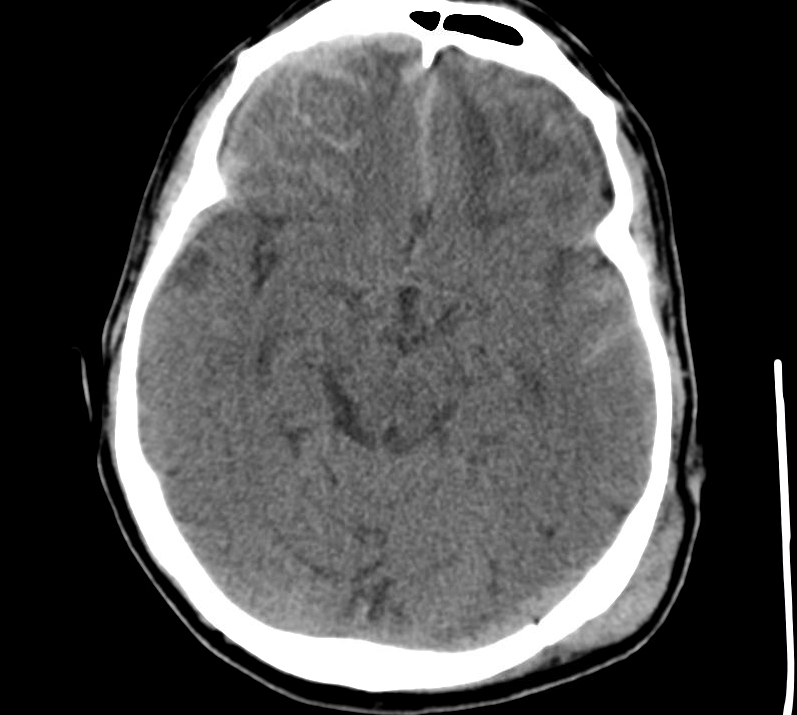
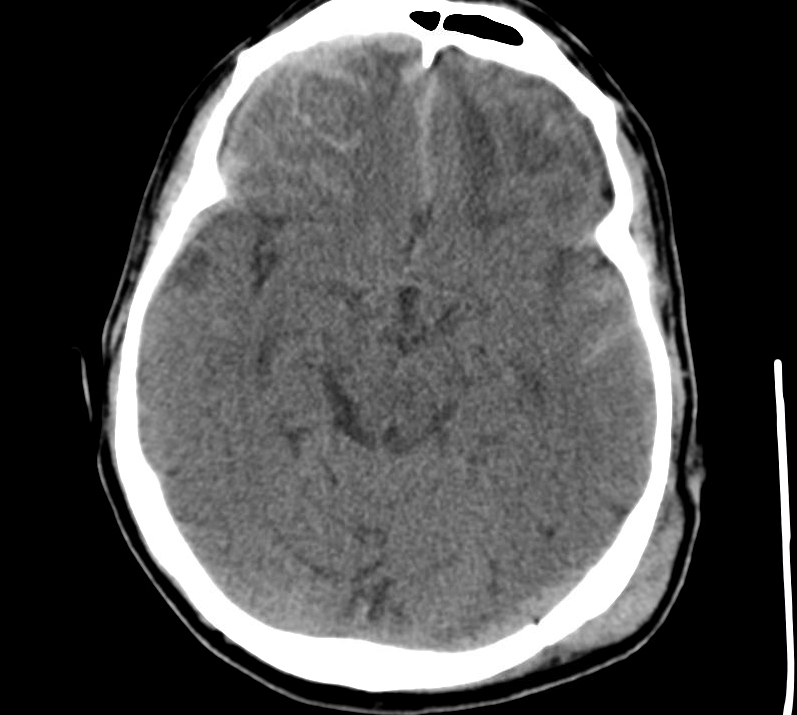
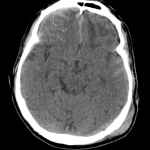
CT Head
Left occipital extracranial soft tissue hematoma
Left occipital epidural hematoma subjacent to the fracture site in addition to subarachnoid hemorrhage within the sulci of the left temporal lobe and interpeduncular cistern
Extra-axial fluid collection along the right frontal convexity, tracking down the anterior falx, compatible with a subdural hematoma
Differential Diagnosis for bowel obstruction: 1, 2, 3

Types of Abdominal Pain: 4

References:
- Kulaylat MN, Doerr RJ. Small bowel obstruction. In: Holzheimer RG, Mannick JA, editors. Surgical Treatment: Evidence-Based and Problem-Oriented. Munich: Zuckschwerdt; 2001. Available from: http://www.ncbi.nlm.nih.gov/books/NBK6873/
- Jackson, P. G., & Raiji, M. T. (2011). Evaluation and management of intestinal obstruction. American family physician, 83(2), 159–165.
- Maung, A. A., Johnson, D. C., Piper, G. L., Barbosa, R. R., Rowell, S. E., Bokhari, F., Collins, J. N., et al. (2012). Evaluation and management of small-bowel obstruction. Journal of Trauma and Acute Care Surgery, 73, S362–S369. doi:10.1097/TA.0b013e31827019de
- Stabile, Bruce. “The Acute Abdomen.” Chairman’s Hour. Harbor UCLA Department of Surgery Student Lecture Series. 5/17/13. Lecture.


































 CC:
CC: