Brief H&P
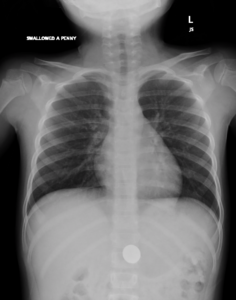
A 47-year-old male with no known medical history presents with dysphagia. He reports 3 weeks of symptoms, describing difficulty predominantly with swallowing solid foods which is aided by the concomitant ingestion of liquids. He points to his throat as the area of discomfort, but has not noted any choking or coughing after attempts at swallowing. He occasionally suffers from “heartburn”, describing a burning sensation in his chest provoked by certain foods and was previously prescribed omeprazole which he has not taken for several years. He denies any prior surgeries, tobacco or alcohol use, relevant family history or similar symptoms in the past.
Physical examination was unrevealing, demonstrating a normal neurological examination, normal phonation, normal oropharynx and no appreciable neck masses. The patient was observed to comfortably swallow water.
He was discharged with gastroenterology follow-up and ultimately underwent esophagogastroduodenoscopy which demonstrated narrowing of the distal esophagus suggestive of a peptic stricture. Dilation was deferred in favor of resumption of proton pump inhibitor therapy.
Types of Dysphagia1,2
- Oropharyngeal3
- Characterized by difficulty initiating swallowing and accompanied by choking/coughing, nasopharyngeal regurgitation or aspiration.
- Involved anatomy: Tongue, muscles of mastication, soft palate (elevation to close nasopharynx), suprahyoid muscles (elevate larynx), epiglottis (occlude airway), cricopharyngeus muscle (release upper esophageal sphincter). Neurological control predominantly coordinated by cranial nerves (V, VII, IX, X, XII)
- Esophageal4
- Delayed after initiating swallowing and characterized by a sensation of food bolus arresting in transit.
- Involved anatomy: Skeletal and smooth muscle along the esophagus and lower esophageal sphincter. Neurological control predominantly coordinated by medulla
Important Historical Features5,6
- Difficulty with liquids suggests motility problem
- Difficulty with solids only or solids progressing to liquids suggests mechanical obstruction
- Identify a history of head and neck surgery or radiation therapy
- Identify a personal or family history of connective tissue disorder (scleroderma, RA, SLE) which may be associated with esophageal dysmotility
- Review home medications (NSAID, bisphosphonate, potassium chloride, ferrous sulfate)
- Immunocompromised patients are at risk for infectious esophagitis (Candida, CMV, HSV) which are generally associated with odynophagia
- A history of heartburn may be associated with reflux-mediated complications such as erosive esophagitis, peptic stricture, and adenocarcinoma of the esophagus
- Young patients are more likely to be affected by eosinophilic esophagitis
- Patient localization of site of obstruction is generally accurate, patients are more accurate at localizing proximal than distal obstructions7
Algorithm for the Evaluation of Dysphagia8

Management9-11
Patients who are safely tolerating oral intake can be referred for outpatient gastroenterology evaluation. Admission should be considered for patients at high-risk for aspiration.
References
- Spieker MR. Evaluating dysphagia. Am Fam Physician. 2000;61(12):3639-3648.
- Abdel Jalil AA, Katzka DA, Castell DO. Approach to the patient with dysphagia. Am J Med. 2015;128(10):1138.e17-.e23. doi:10.1016/j.amjmed.2015.04.026.
- Shaker R. Oropharyngeal Dysphagia. Gastroenterol Hepatol (N Y). 2006;2(9):633-634.
- Galmiche JP, Clouse RE, Bálint A, et al. Functional esophageal disorders. Gastroenterology. 2006;130(5):1459-1465. doi:10.1053/j.gastro.2005.08.060.
- McCullough GH, Martino R. Clinical Evaluation of Patients with Dysphagia: Importance of History Taking and Physical Exam. In: Manual of Diagnostic and Therapeutic Techniques for Disorders of Deglutition. New York, NY: Springer New York; 2012:11-30. doi:10.1007/978-1-4614-3779-6_2.
- Cook IJ. Diagnostic evaluation of dysphagia. Nat Clin Pract Gastroenterol Hepatol. 2008;5(7):393-403. doi:10.1038/ncpgasthep1153.
- Wilcox CM, Alexander LN, Clark WS. Localization of an obstructing esophageal lesion. Is the patient accurate? Dig Dis Sci. 1995;40(10):2192-2196.
- Trate DM, Parkman HP, Fisher RS. Dysphagia. Evaluation, diagnosis, and treatment. Prim Care. 1996;23(3):417-432.
- American Gastroenterological Association medical position statement on management of oropharyngeal dysphagia. Gastroenterology. 1999;116(2):452-454. doi:10.1016/S0016-5085(99)70143-5.
- Spechler SJ. American Gastroenterological Association medical position statement on treatment of patients with dysphagia caused by benign disorders of the distal esophagus. Gastroenterology. 1999;117(1):229-232. doi:10.1016/S0016-5085(99)70572-X.
- Varadarajulu S, Eloubeidi MA, Patel RS, et al. The yield and the predictors of esophageal pathology when upper endoscopy is used for the initial evaluation of dysphagia. Gastrointest Endosc. 2005;61(7):804-808.