Brief HPI:
A middle-aged female with no known medical history is brought to the emergency department with altered mental status. Her family notes worsening confusion over the past 2-3 days associated with vomiting and yellow discoloration of skin and eyes.
Initial vital signs were normal, though with borderline hypotension (99/64mmHg). Examination demonstrated an alert, but lethargic patient with jaundice and scleral icterus, no skin lesions were appreciated. Laboratory studies were obtained:
CBC
- WBC: 21.3 (N: 83%, Bands: 11%)
- Hb: 5.5
- Plt: 6k
- Marked schistocytes
Coagulation Panel
- INR: 1.26
- PTT: Normal
- Fibrinogen: Normal
- FDP: Normal
- D-dimer: >9,000 (normal 250)
- Haptoglobin: Undetectable
- LDH: 1493
CMP
- Creatinine: 1.1
- AST/ALT: Normal
- TB: 4.3, DB: 0.8
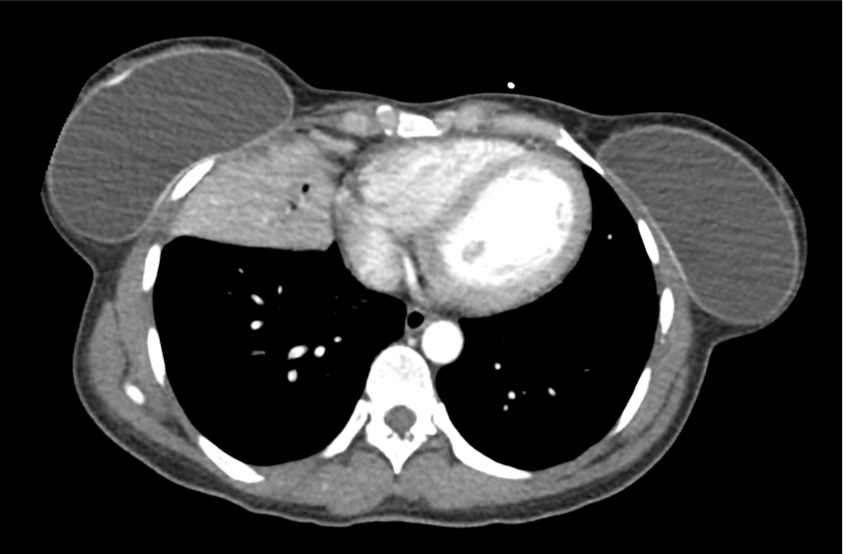
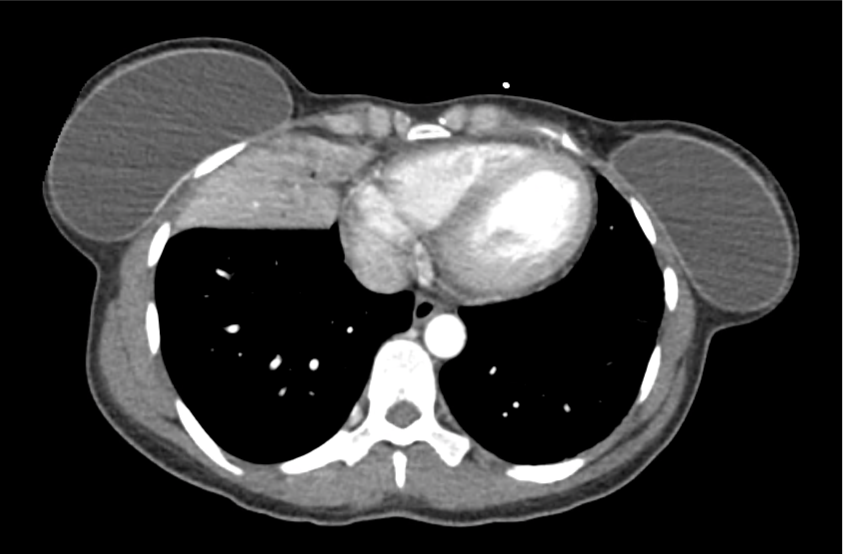
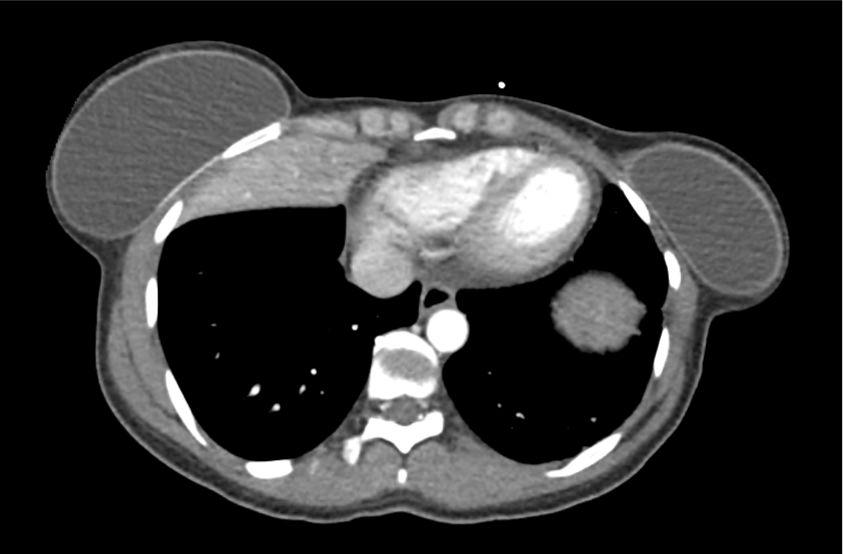
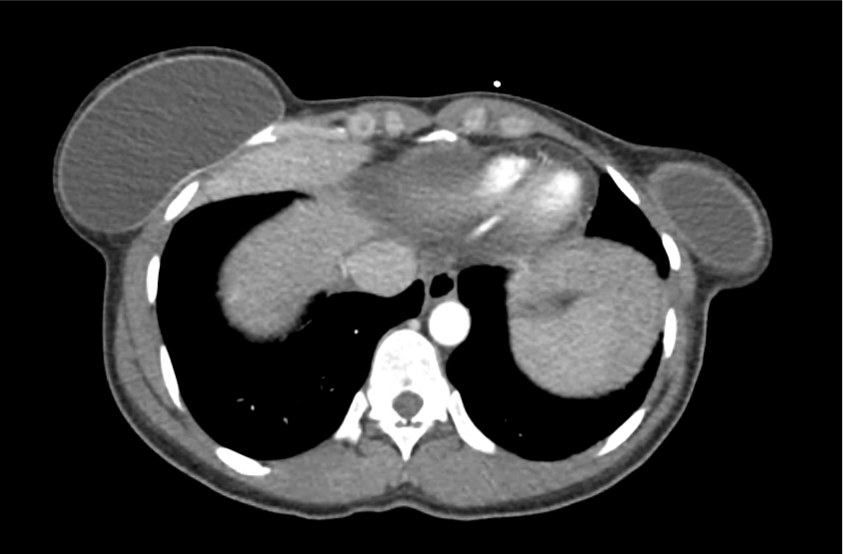
Imaging:
CT Head: No acute intracranial process.
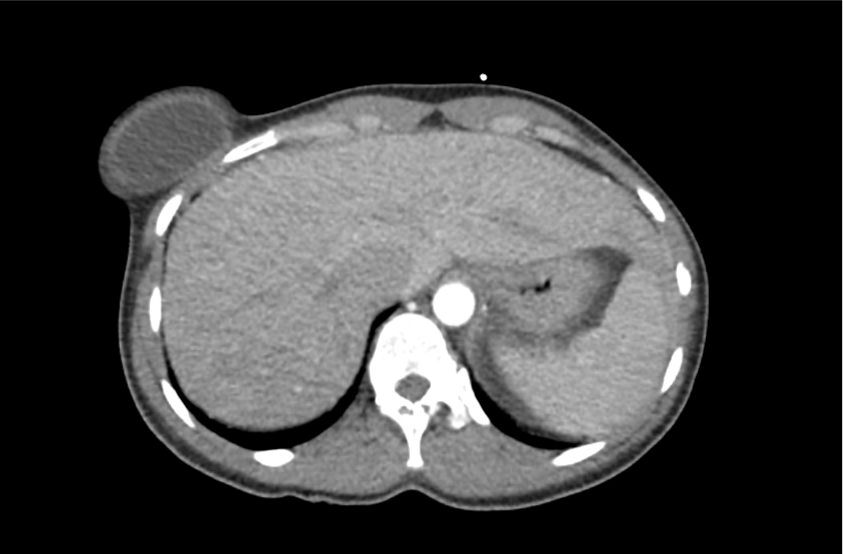
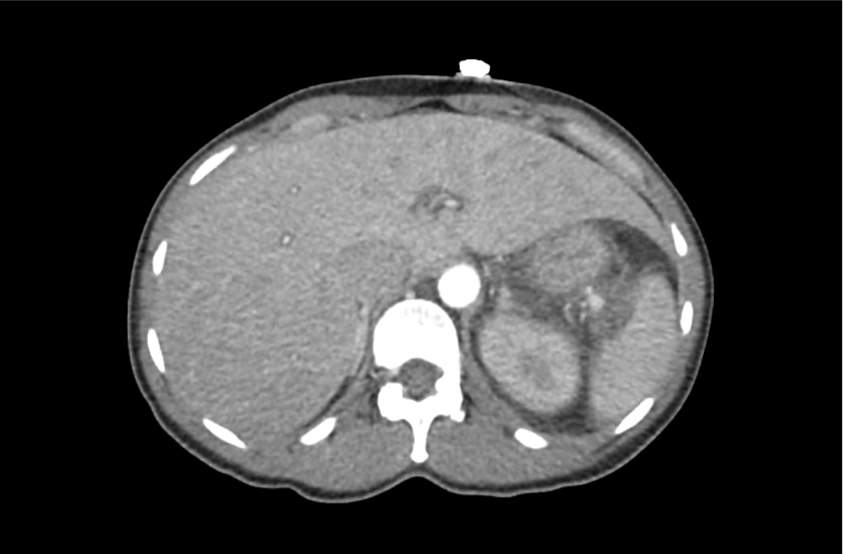
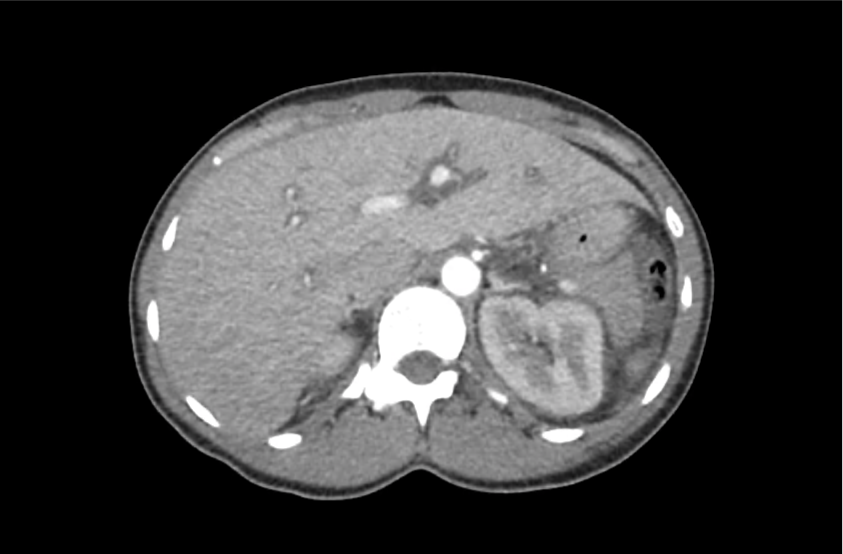
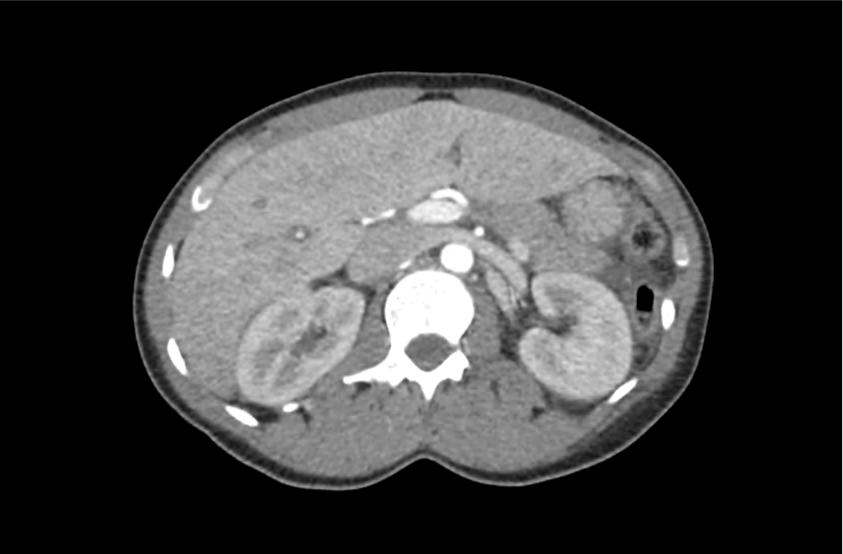
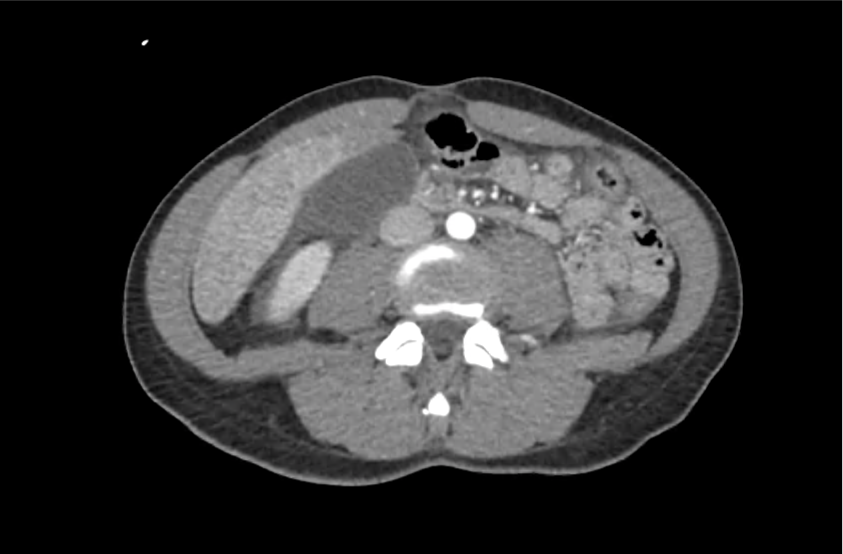
CT Abdomen/Pelvis with Contrast
Moderate free intra-abdominal fluid, heterogeneous liver with periportal edema, dense right middle lobe consolidation.
ED Course:
The patient developed worsening respiratory failure with hypoxia and tachypnea requiring endotracheal intubation. Thrombotic thrombocytopenic purpura was suspected and while awaiting emergent plasma exchange transfusion, the patient arrested and resuscitation efforts were unsuccessful.
The patient’s ADAMTS13 activity level was <3%. Autopsy demonstrated consolidation of the right middle lobe with possible lymphoproliferative mass, and lung petechial hemorrhages from microvascular thrombi.
Differential Diagnosis of Thrombocytopenia 1-7
Algorithm for the Evaluation of Thrombocytopenia 8
Definition 9
- Mild: <150k
- Moderate: 100-150k
- Severe: <50k
- 10-30k: bleeding with minimal trauma
- <10k: increased risk spontaneous bleeding
History 9,10
- Prior platelet count
- Family history bleeding disorders
- Medications
- Heparin
- Quinine, quinidine
- Rifampin
- Trimethoprim-sulfamethoxazole
- Vancomycin
- Alcohol use
- Travel-related infections
Physical Examination 9,10
- Splenomegaly (liver disease)
- Lymphadenopathy (infection, malignancy)
Workup 10,11
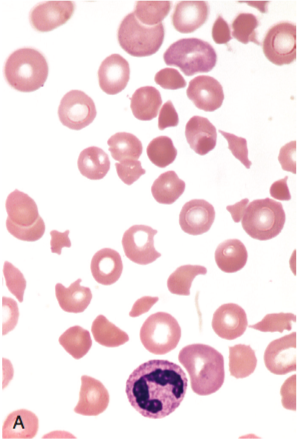
Red blood cell fragments (schistocytes) 11
- hCG
- Repeat CBC
- Detect spurious measure
- Neutrophil-predominant leukocytosis: bacterial infection
- Immature leukocytes (blasts): leukemia, myelodysplasia
- Peripheral smear
- Schistocytes: microangiopathic process (DIC, TTP, HUS)
- Atypical lymphocytes: viral infection
- Intracellular parasites: malaria
- Hypersegmented neutrophils: nutritional deficiency
- Infectious features: HIV, HCV, EBV, H.pylori, blood cultures
- Autoimmune features: ANA, APL-Ab
- Suspected occult liver disease: LFT, PT/PTT/INR
- Suspected thrombotic microangiopathy: PT/PTT/INR, haptoglobin, LDH, fibrinogen, FDP, d-dimer
Specific Conditions 2-6,9,12-20
| Disease | Cause | Presentation | Laboratory Findings | Treatment |
|---|---|---|---|---|
| DIC | Sepsis Trauma Burn Malignancy |
Bleeding Multi-organ failure Shock |
INR Fibrinogen FDP D-dimer |
Directed at underlying cause Transfusion thresholds for hemorrhage: FFP for INR >1.5 Platelets if <50k Cryoprecipitate of fibrinogen <100mg/dL |
| TTP | Insufficient ADAMTS-13 activity | Non-specific constitutional symptoms (ex. weakness) Neuro: headache, AMS, focal neuro deficit GI: abdominal pain, nausea/vomiting |
LDH Reticulocyte Unconjugated bilirubin Haptoglobin |
Plasma exchange |
| HUS | Shiga-toxin-producing bacteria, E. coli O157:H7 | Bloody diarrhea, anuria, oliguria, and hypertension | Aggressive supportive care | |
| HELLP | Spectrum of eclampsia | Hypertension Visual symptoms Headache RUQ abdominal pain |
AST/ALT Uric acid Unconjugated bilirubin LDH Reticulocyte Haptoglobin |
Delivery, MgSO4 |
| ITP | Primary ITP
Secondary ITP |
Usually asymptomatic, may have petechiae or easy bruising | Isolated thrombocytopenia | Steroids |
| HIT | Exposure to heparin or LMWH | Thrombocytopenia or a 50 percent reduction in platelet count between 5-10d exposure New thrombosis or skin necrosis 4 T’s score |
Platelet factor 4 antibodies | Withdraw heparin |
References
- Greinacher A, Selleng S. How I evaluate and treat thrombocytopenia in the intensive care unit patient. Blood. 2016;128(26):3032-3042. doi:10.1182/blood-2016-09-693655.
- Joly BS, Coppo P, Veyradier A. Thrombotic thrombocytopenic purpura. Blood. 2017;129(21):2836-2846. doi:10.1182/blood-2016-10-709857.
- Leslie SD, Toy PT. Laboratory hemostatic abnormalities in massively transfused patients given red blood cells and crystalloid. Am J Clin Pathol. 1991;96(6):770-773.
- Neunert C, Lim W, Crowther M, et al. The American Society of Hematology 2011 evidence-based practice guideline for immune thrombocytopenia. Blood. 2011;117(16):4190-4207. doi:10.1182/blood-2010-08-302984.
- Kappler S, Ronan-Bentle S, Graham A. Thrombotic microangiopathies (TTP, HUS, HELLP). Emerg Med Clin North Am. 2014;32(3):649-671. doi:10.1016/j.emc.2014.04.008.
- Greinacher A. Heparin-Induced Thrombocytopenia. Solomon CG, ed. N Engl J Med. 2015;373(3):252-261. doi:10.1056/NEJMcp1411910.
- Reardon JE Jr., Marques MB. Evaluation of Thrombocytopenia. Lab Med. 2006;37(4):248-250. doi:10.1309/R7P79KERAJHPRHLT.
- Stasi R. How to approach thrombocytopenia. Hematology Am Soc Hematol Educ Program. 2012;2012:191-197. doi:10.1182/asheducation-2012.1.191.
- Gauer RL, Braun MM. Thrombocytopenia. Am Fam Physician. 2012;85(6):612-622.
- Abrams CS. 172 – Thrombocytopenia. Twenty Fifth Edition. Elsevier Inc.; 2016:1159–1167.e2. doi:10.1016/B978-1-4557-5017-7.00172-0.
- Wilson CS, Vergara-Lluri ME, Brynes RK. Chapter 11 – Evaluation of Anemia, Leukopenia, and Thrombocytopenia. Second Edition. Elsevier Inc.; 2017:195-234.e195. doi:10.1016/B978-0-323-29613-7.00011-9.
- Hui P, Cook DJ, Lim W, Fraser GA, Arnold DM. The frequency and clinical significance of thrombocytopenia complicating critical illness: a systematic review. Chest. 2011;139(2):271-278. doi:10.1378/chest.10-2243.
- Jokiranta TS. HUS and atypical HUS. Blood. 2017;129(21):2847-2856. doi:10.1182/blood-2016-11-709865.
- Neunert CE. Management of newly diagnosed immune thrombocytopenia: can we change outcomes? Hematology Am Soc Hematol Educ Program. 2017;2017(1):400-405. doi:10.1182/asheducation-2017.1.400.
- Lambert MP, Gernsheimer TB. Clinical updates in adult immune thrombocytopenia. Blood. 2017;129(21):2829-2835. doi:10.1182/blood-2017-03-754119.
- Arepally GM. Heparin-induced thrombocytopenia. Blood. 2017;129(21):2864-2872. doi:10.1182/blood-2016-11-709873.
- Aster RH, Bougie DW. Drug-induced immune thrombocytopenia. N Engl J Med. 2007;357(6):580-587. doi:10.1056/NEJMra066469.
- Boral BM, Williams DJ, Boral LI. Disseminated Intravascular Coagulation. Am J Clin Pathol. 2016;146(6):670-680. doi:10.1093/ajcp/aqw195.
- Scully M, Hunt BJ, Benjamin S, et al. Guidelines on the diagnosis and management of thrombotic thrombocytopenic purpura and other thrombotic microangiopathies. Br J Haematol. 2012;158(3):323-335. doi:10.1111/j.1365-2141.2012.09167.x.
- Levine RL, Hursting MJ, Drexler A, Lewis BE, Francis JL. Heparin-induced thrombocytopenia in the emergency department. Ann Emerg Med. 2004;44(5):511-515. doi:10.1016/j.annemergmed.2004.06.004.