ID:
ID:
19yo G0, hCG negative, presenting with lower abdominal pain for 3 weeks.
HPI:
The patient states that she has had progressively worsening lower abdominal pain for the past three weeks. She describes the pain as constant, cramping, currently 8/10 in severity with radiation to the right flank. The pain is improved somewhat with ibuprofen and worsened with movement. She reports subjective F/C, some vaginal bleeding, but no other discharge and no dysuria. She is sexually active with one partner, using condoms occasionally. She has no significant PMH, no history of STI and a PSH of appendectomy. She denies any current or prior T/E/D use.
PE:
- VS: 110/60mmHg, 60bpm, 99.5°, 16/min
- HEENT: NC/AT, PERRL, EOMI, MMM w/o lesions
- CV: RRR, no M/G/R
- Lungs: CTAB
- Abd: +BS, soft, non-distended, TTP RLQ > LLQ, no rebound/guarding
- Back: no CVAT
- Pelvic: external genitalia normal, scant blood in vault, os closed, no discharge, + CMT, + uterine tenderness, + adnexal tenderness
Labs/Imaging:
- TVUS: normal appearing uterus/adnexa, possible free fluid (hemorrhagic vs. inflammatory) in pelvis
- Wet mount: negative
- Urine dip: -LE/nitrites, -protein, +blood
Assessment:
19yo G0, hCG negative, with pelvic pain and vaginal bleeding. Findings of lower abdominal tenderness, cervical motion/uterine/adnexal tenderness on examination, and low-grade fever are suggestive of PID. Other considerations include UTI, however, absence of dysuria, CVAT, and negative urine dip do not support this diagnosis. Will evaluate further with GC/CT, and treat empirically with ceftriaxone 250mg IM x1 and doxycycline 100mg PO BID x14d with follow-up in 48h.
Differential Diagnosis of Acute Pelvic Pain:
Common causes:
- Gynecologic
- PID, TOA
- Neoplasm (torsion, rupture)
- Leiomyoma (torsion, degeneration)
- Endometriosis
- Endometritis
- Ectopic pregnancy
- SAB
- Obstetric
- Labor
- Uterine rupture
- Abruptio placentae
- Diastasis symphesis pubis
- Non-gynecologic
- Appendicitis
- Cystitis (UTI)
- Diverticulitis
- Urinary tract calculi
- Abdominal wall trauma
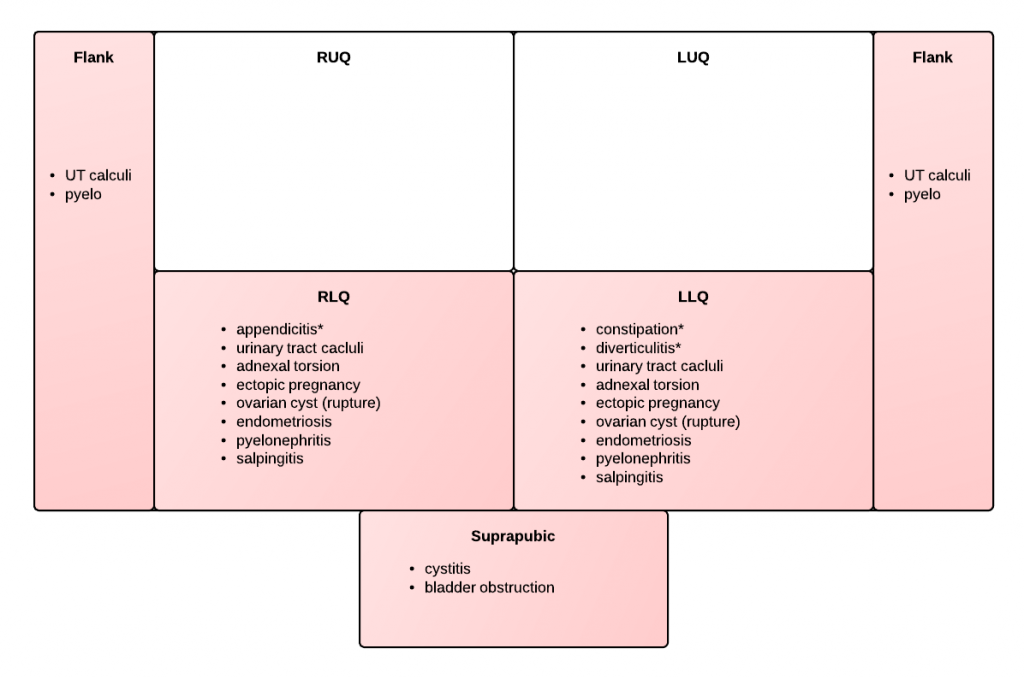
Location of pain:
ROS:
- discharge + dyspareunia: PID
- missed menses + cramping/bleeding: SAB, ectopic
- anorexia, N/V: appendicitis, torsion
A System for the Evaluation and Management of PID:
- Pathogens: GC, CT, gardnerella, haemophilus
- Evaluation:
- Pelvic exam: CMT, uterine tenderness, adnexal tenderness, abnormal discharge, wet mount WBC’s
- Labs: + GC/CT, ↑ ESR/CRP
- VS: T > 101°
- Imaging: thickened tubes, free pelvic fluid, TOA
- Indications for admission:
- Acute abdomen, toxic appearance, unstable VS
- Pregnancy
- Failed outpatient, can’t tolerate PO
- TOA
- Outpatient management:
- Ceftriaxone 250mg IM x1
- Doxycycline 100mg PO BID x14d
- ± Metronidazole 500mg PO BID x14d
References:
- Hacker and Moore’s essentials of obstetrics and gynecology. Philadelphia, PA: Saunders/Elsevier, 2010.
- CDC – Pelvic Inflammatory Disease – 2010 STD Treatment Guidelines: http://www.cdc.gov/std/treatment/2010/pid.htm