HPI:
51 year-old male with a history of HTN, DM and chronic alcohol abuse presenting with lower extremity swelling. He notes one month of progressive, bilateral lower extremity swelling, in the past two weeks associated with increasing pain and redness and is now no longer able to ambulate due to pain. He denies fevers/chills, chest pain or shortness of breath. He also denies orthopnea and paroxysmal nocturnal dyspnea. He states that he has not had these symptoms prior to one month ago. On review of systems he denies nausea/vomiting, abdominal pain, and changes in bowel or urinary habits. He has a history of GI bleeding (unknown treatment) but denies hematemesis, hematochezia or melena. He has previously experienced alcohol withdrawal, which manifested as tremors, but no hallucinations or seizures.
PMH:
- HTN
- DM
- Chronic EtOH abuse
SHx:
- Drinks 1-2 pints of alcohol daily, last drink this morning.
- Denies current tobacco or drug abuse, no prior IVDA.
Physical Exam:
| VS: |
T |
37.6 |
HR |
86 |
RR |
16 |
BP |
128/84 |
O2 |
99% RA |
| Gen: |
Adult, non-obese male, lying in bed. Tremors noted in upper extremities. |
| HEENT: |
PERRL, EOMI, no scleral icterus. Mucous membranes moist. |
| CV: |
RRR, normal S1/S2, no additional heart sounds, JVP 3cm above sternal angle at 30°. |
| Lungs: |
CTAB, no crackles. |
| Abd: |
Soft, non-distended, with normoactive bowel sounds. Liver edge palpated 1cm below costal margin at mid-clavicular line, non-tender. No rebound/guarding. |
| Ext: |
Warm, well-perfused with 2+ distal pulses (PT, DP). 3+ pitting edema symmetric in bilateral lower extremities to knee. Erythema and warmth bilaterally extending from ankles to mid-shin. Mild tenderness to palpation. No pain with passive dorsiflexion. 3x3cm shallow ulceration below medial malleolus on right lower extremity without underlying fluctuance or expression of purulent material. No venous varicosities noted. Decreased sensation to light touch below knee bilaterally. |
| Rectal: |
Normal rectal tone, brown stool, guaiac negative. |
| Neuro: |
Alert and oriented, CN II-XII intact, gait intact, normal FTN/RAM. |
Labs/Studies:
- CBC: 7.4/13.1/39/180
- Creatinine: 0.84
- Albumin: 4.3
- BNP: 28
Imaging:
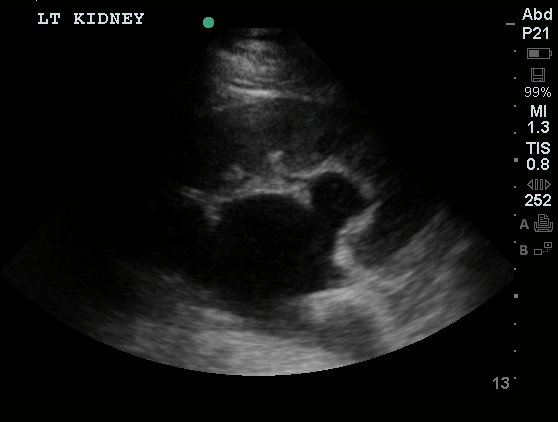
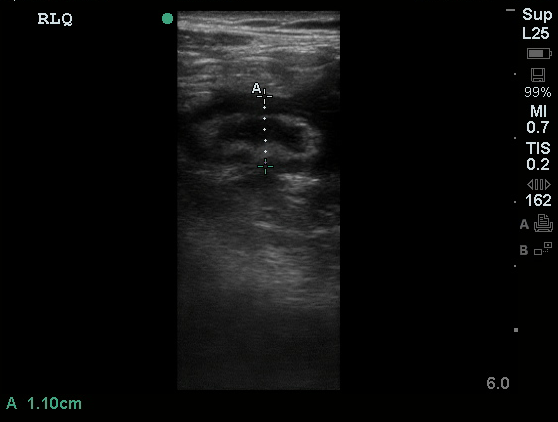
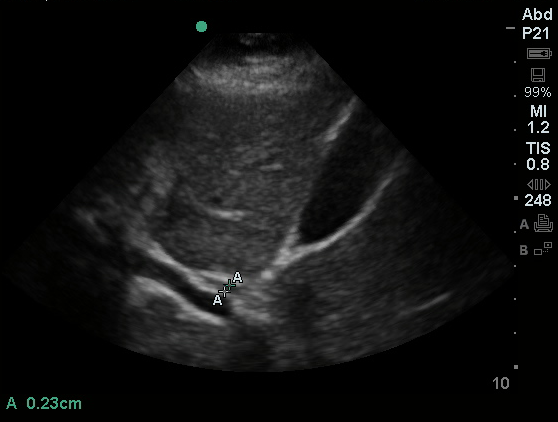
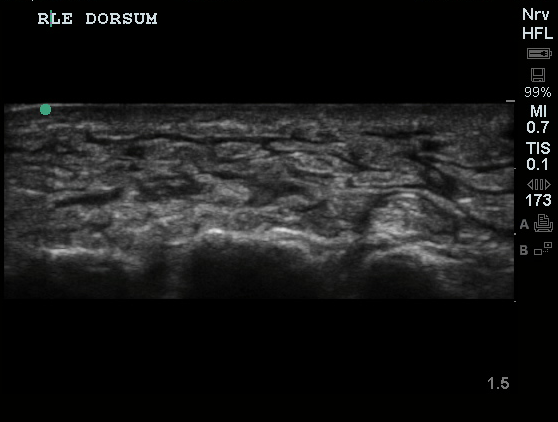
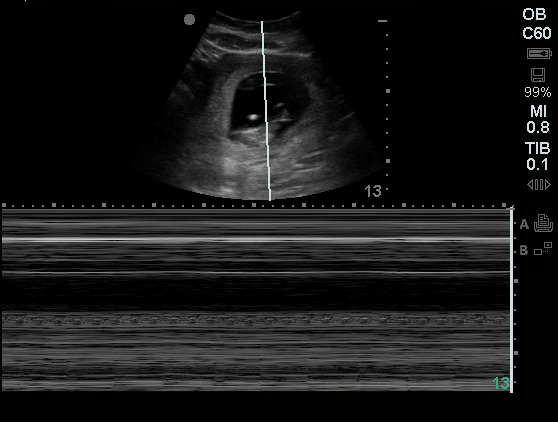
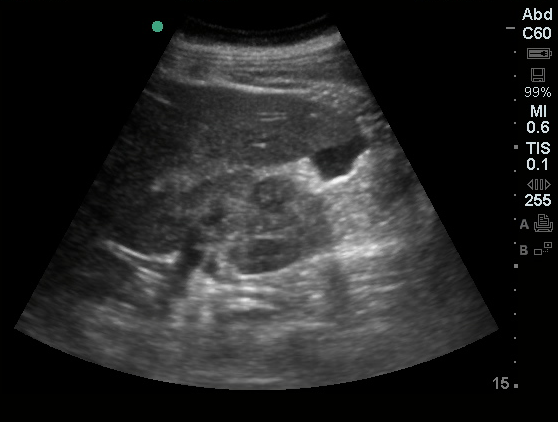
Venous Lower Extremity Ultrasound
- No DVT.
- Pulsatile flow in bilateral EIV (external iliac veins) suggestive of elevated right heart pressure.
Assessment/Plan:
51M with HTN, DM, EtOH abuse presenting with lower extremity edema. Chronic bilateral lower extremity edema likely secondary to chronic venous insufficiency perhaps related to OSA given ultrasound findings of pulsatile flow in EIV’s. Doubt systemic cause: no evidence of heart failure on exam and normal BNP, no stigmata of cirrhosis and normal albumin, normal creatinine. Also, no evidence of DVT on ultrasound though bilateral DVT unlikely. Bilateral cellulitis also unlikely as the patient is afebrile without leukocytosis, however the patient was started on antibiotics including ceftriaxone and TMP/SMX given erythema, warmth and tenderness to palpation. The patient received benzodiazepines which eased withdrawal symptoms and he was admitted for continued treatment.
Mechanisms of Lower Extremity Edema: 1

Differential Diagnosis of Lower Extremity Edema: 1,2

Evaluation:
History 1,2
- Duration: acute (<72h) vs. chronic
- Pain: DVT, CRPS, less severe in venous insufficiency
- Systemic Disease
- Cardiac: orthopnea, PND
- Renal: proteinuria
- Hepatic: jaundice, ascites
- Malignancy: lymphedema
- Improvement with elevation/recumbency: venous insufficiency
- OSA: snoring, daytime somnolence
- Medications: B-blocker, CCB, hormones, NSAID’s
Physical Exam 1,2
- Distribution: unilateral, bilateral, generalized
- Quality: pitting, non-pitting
- TTP: DVT, cellulitis
- Varicose veins: venous insufficiency
- Kaposi-Stemmer: inability to pinch dorsum of foot at base of 2nd toe (lymphedema)
- Systemic Disease
- Cardiac: JVD, crackles
- Hepatic: ascites, scleral icterus, spider angiomas
- Brawny, medial maleolar involvement: venous insufficiency
Key Features Distinguishing Cellulitis: 3
- Typically unilateral and acute
- Often with systemic symptoms (fever, leukocytosis)
- Risk Factors: immunosuppression, previous episodes, DM, PVD
References:
- Trayes, K. P., Studdiford, J. S., Pickle, S., & Tully, A. S. (2013). Edema: diagnosis and management. American family physician, 88(2), 102–110.
- Ely, J. W., Osheroff, J. A., Chambliss, M. L., & Ebell, M. H. (2006). Approach to leg edema of unclear etiology. Journal of the American Board of Family Medicine : JABFM, 19(2), 148–160.
- Keller, E. C., Tomecki, K. J., & Alraies, M. C. (2012). Distinguishing cellulitis from its mimics. Cleveland Clinic journal of medicine, 79(8), 547–552. doi:10.3949/ccjm.79a.11121
- WikEM: Pedal edema